不同麻醉方法对超高龄髋部骨折手术患者围术期血压的影响
2019-12-17张虎汪海钢李艳玲何艳娟李跃兵黄余亮
张虎 汪海钢 李艳玲 何艳娟 李跃兵 黄余亮
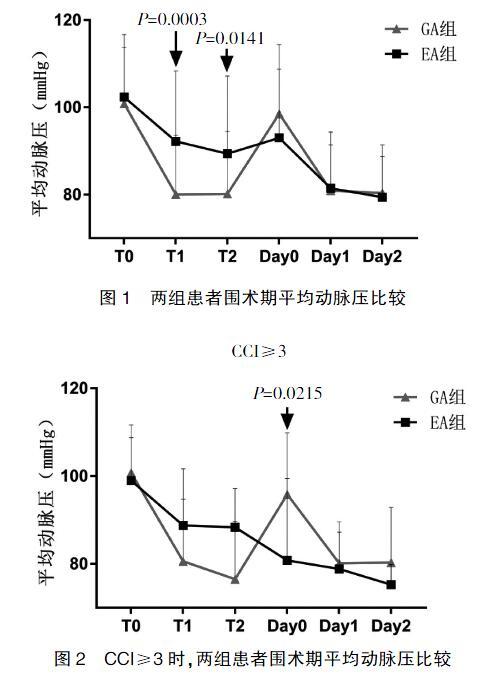

[摘要] 目的 探討不同麻醉方法对超高龄髋部骨折患者围术期血流动力学的影响。 方法 选择2017年5月~2019年2月在我院行髋部骨折手术的患者92例,年龄≥90岁,随机分为全身麻醉(general anesthesia,GA)组和硬膜外麻醉(epidural anesthesia,EA)组,每组46例。GA组患者行全身麻醉,EA组患者行硬膜外麻醉。记录术前静息血压(T0)、麻醉诱导或硬膜外起效后血压(T1)、切皮时血压(T2)和术后当天(Day 0)、术后第1天(Day 1)、术后第2天(Day 2)的血压及术中低血压次数。用查尔森合并症指数(Charlson Comorbidity Index,CCI)比较有和无分层情况下两组各时间点的平均动脉血压(MAP)及术中低血压次数。 结果 T1、T2时间点GA组MAP低于EA组(P<0.05),其余时间点MAP无统计学差异。EA组患者低血压次数少于GA组(P<0.05)。亚组分析中,CCI≥3时,Day 0时间点EA组MAP低于GA组(P<0.05),其余时间点MAP无统计学差异(P>0.05)。CCI≥3时,两组低血压次数无统计学差异(P>0.05)。 结论 超高龄髋部骨折手术患者硬膜外麻醉较全身麻醉在血流动力学上更稳定。但在有多个合并症的患者中,两者差异并不明显,且硬膜外麻醉术后当天容易发生低血压。
[关键词] 髋部骨折手术;超高龄患者;麻醉方法;平均动脉压;低血压
[中图分类号] R614 [文献标识码] B [文章编号] 1673-9701(2019)29-0108-05
Effects of different anesthesia methods on perioperative blood pressure of super-aged patients with hip fractures
ZHANG Hu WANG Haigang LI Yanling HE Yanjuan LI Yuebing HUANG Yuliang
Department of Anesthesiology, the Second Affiliated Hospital of Zhejiang University of Traditional Chinese Medicine, Hangzhou 310005, China
[Abstract] Objective To investigate the effects of different anesthesia methods on the perioperative hemodynamics of super-aged patients with hip fractures. Methods Ninety-two patients ≥90 years old who received hip fracture surgery in our hospital from May 2017 to February 2019 were selected and randomly divided into the general anesthesia(GA) group and the epidural anesthesia(EA) group, with 46 patients in each group. The GA group was given general anesthesia and the EA group was given epidural anesthesia. Preoperative resting blood pressure(T0), blood pressure after anesthesia induction or epidural onset(T1), blood pressure at the time of skin incision(T2) and blood pressure on the day of surgery(Day 0), first day after surgery(Day 1), second day after surgery(Day 2) and the number of times of intraoperative hypotension were recorded. The mean arterial blood pressure(MAP) and the number of times of intraoperative hypotension at different time points of the two groups with and without stratification were compared by Charlson Comorbidity Index(CCI). Results The GA group was lower than the EA group in the MAP at T1 and T2(P<0.05), and the MAPs were not statistically different at the other time points(P>0.05). The EA group was less than the GA group in the number of times of hypotension(P<0.05). In the subgroup analysis, when CCI≥3, the EA group was lower than the GA group in the MAP on Day 0(P<0.05), and the MAPs were not statistically different at the other time points(P>0.05). When CCI≥3, the two groups were not statistically different in the number of times of hypotension(P>0.05). Conclusion Epidural anesthesia is more stable than general anesthesia in terms of hemodynamics for the super-aged patients receiving hip fracture surgery. However, in patients with multiple comorbidities, the difference was not significant between the two anesthesia methods, and hypotension is prone to occur on the day of epidural anesthesia.
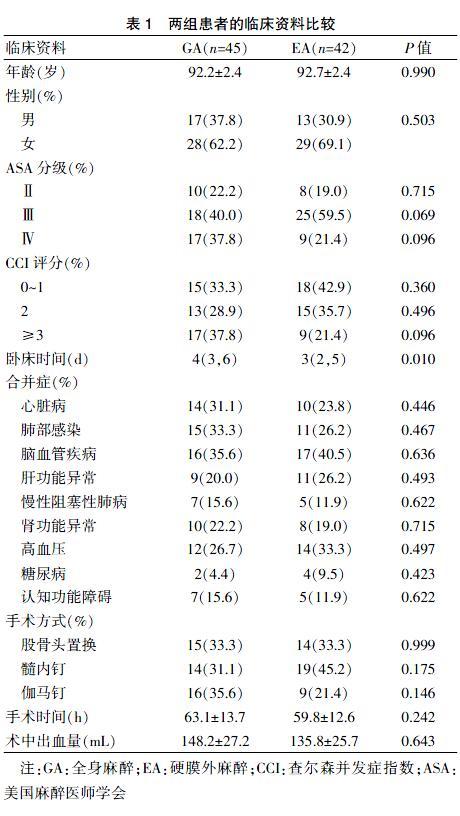
注:GA:全身麻醉;EA:硬膜外麻醉;CCI:查尔森并发症指数;ASA:美国麻醉医师学会
2.2两组患者围术期平均动脉压比較
两组患者围术期T0、T1、T2、Day 0、Day 1、Day 2各时间点平均动脉压比较,T1、T2时间点GA组平均动脉压低于EA组(P<0.05),其余时间点平均动脉压无统计学差异,见表2、图1。各亚组分析中,CCI≥3时,Day 0时间点EA组平均动脉压低于GA组(P<0.05),其余时间点平均动脉压无统计学差异。见表3、图2。
2.3 两组患者术中低血压次数比较
EA组(1.1次)次数少于GA组(2.0次)(P<0.05)。亚组分析中,CCI≥3时,两组低血压次数无统计学差异(1.2次 vs 1.5次)。见图3、4。
3讨论
髋部骨折是常见的外伤性疾病,多见于老年患者,中位年龄约为83岁[11-12]。由于该类患者常伴发多种并存疾病和合并症,麻醉及围术期管理不当,术后并发症和死亡率显著增加。在英国髋部骨折患者30 d的死亡率约为8%,且这一数值长期保持相对不变[13]。尽管现代麻醉技术取得长足发展,但对于老年人髋关节手术的最佳麻醉方法尚未达成一致。Neuman等[9,14]回顾18 158例接受髋部骨折手术的老年患者,全麻后炎症反应综合征、肺炎、咽喉痛、声嘶等并发症发生率明显高。老年患者对麻醉的反应与其他人群不同,心脏储备减少,使老年人在麻醉诱导过程中更容易受到血压变化的影响[15-16]。有研究表明,与年龄有关的血管张力变化,应对自稳态的能力下降,交感系统紧张活动增加,这些因素使全麻诱导时患者的血压显著降低[17]。根据麻醉学神经学学会声明,围术期低血压是导致围术期脑卒中发生的重要相关因素[18]。因此,为避免气管插管相关并发症及全麻诱导时低血压,高龄患者常采用硬膜外麻醉,其潜在好处包括减少阿片类药物的用量、减少手术后患者的精神混乱、减少血栓栓塞,可作为严重呼吸道疾病患者更安全的选择[13]。
查尔森合并症指数(Charlson comorbidity index,CCI)是一种基于患者所患疾病数目及严重程度且涉及权重因素的评分系统。评估与一系列条件相关的合并症风险,以便为医务工作者提供具体筛查或为医疗诊治过程中提供知情决策建议。原始CCI评分源自685例肺癌患者的队列研究,并测试合并疾病在住院病死率和十年病死率的预测能力[19]。2011年Quan H等[20]纳入55 929例患者临床数据的研究结果表明,CCI疾病的权重分配应当更新,细化纳入疾病的种类。CCI量化既往基础疾病,以此评价患者的预后,多个研究中证实CCI评分系统有效,如急性心肌梗死、冠脉综合征、缺血性休克、腹膜透析和急诊老年患者的研究,目前广泛应用于急诊科、肿瘤科、重症医学科等[21-24]。将CCI应用于麻醉科,利用CCI评分将病情复杂的超高龄髋部骨折患者进行分层研究,使术前存在不同合并症的患者潜在获益。2014年Herrera等[17]报道老年髋部手术患者全麻诱导时血压显著降低,而硬膜外组血压下降更大。本次研究表明,CCI≥3时,硬膜外麻醉较全身麻醉失去了血流动力学稳定的优势,且术后当天更容易发生低血压,与此前的临床研究一致。
需要特别报道的是本次研究中硬膜外组排除的2例自动出院患者,在术后当天均发生持续性、难治性低血压。虽然其低血压是否与实施硬膜外麻醉相关无法得到证实,但提示在对病情复杂的超高龄患者实施硬膜外麻醉时,应避免施加易导致围术期低血压发生的医疗措施,并且积极使用血管活性药物维持血流动力学稳定。
综上所述,超高龄髋部骨折手术患者硬膜外麻醉较全身麻醉在术中血流动力学的稳定上具有优势,但在病情复杂术前合并症多的患者中,两种麻醉方法在这方面并没有显著差异,且硬膜外麻醉术后当天更容易产生低血压,带来相关风险。
[参考文献]
[1] Simon MJ,Veering BT,Stienstra R. Effect of age on the clinical profile and systemic absorption and disposition of levobupivacaine after epidural administration[J]. Br J Anaesth,2004,93(4):512-520.
[2] Panula J,Pihlajamaki H,Mattila VM. Mortality and cause of death in hip fracture patients aged 65 or older:A population-based study[J]. BMC Musculoskelet Disord,2011,12:105.
[3] Lonjaret L,Lairez O,Minville V,et al. Optimal perioperative management of arterial blood pressure[J]. Integr Blood Press Control,2014,7:49-59.
[4] Turgut Donmez,Erdem VM,Uzman S,et al. Laparoscopic cholecystectomy under spinal-epidural anesthesia vs general anaesthesia:A prospective randomised study[J]. Ann Surg Treat Res,2017,92(3):136-142.
[5] Berninger MT,Friederichs J,Leidinger W,et al. Effect of local infiltration analgesia,peripheral nerve blocks,general and spinal anesthesia on early functional recovery and pain control in total knee arthroplasty[J]. BMC Musculoskelet Disord,2018,19(1):232.
[6] Charlson ME,Pompei P,Ales KL,et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation[J]. Chronic Dis,1987,40(5):373-383.
[7] Singh M,Rihal CS,Lennon RJ,et al. Influence of frailty and health status on outcomes in patients with coronary disease undergoing percutaneous revascularization[J]. Circ Cardiovasc Qual Outcomes,2011,4(5):496-502.
[8] Chang CM,Yin WY,Wei CK. Adjusted age-adjusted charlson comorbidity index score as a risk measure of perioperative mortality before cancer surgery[J]. Plos One,2016,11(6):e0157900.
[9] Neuman,Rosenbaum,Ludwig,et al. Anesthesia technique,mortality,and length of stay after hip fracture surgery[J]. JAMA,2014,311(24):2508-2517.
[10] Sieber Frederick E,Neufeld Karin J,Gottschalk Allan,et al. Effect of depth of sedation in older patients undergoing hip fracture repair on postoperative delirium: The STRIDE randomized clinical trial[J]. JAMA Surgery,2018, 153(11):987-995.
[11] Bhandari,Swiontkowski. Management of acute hip fracture[J]. N Engl J Med,2017,377(21):2053-2062.
[12] Rockwood PR,Horne JG,Cryer C. Hip fractures:A future epidemic?[J]. J Orthop,1990,4(4):388-393.
[13] Dawe H. Modernising Hip Fracture anaesthesia:[J]. Open Orthopaedics Journal,2017,11(Suppl-7,M3):1190-1199.
[14] Neuman,Mehta S,Bannister ER,et al. Pilot randomized controlled trial of spinal versus general anesthesia for hip fracture surgery[J]. J Am Geriatr Soc,2016,64(12):2604-2606.
[15] Wood RJ,White SM. Anaesthesia for 1131 patients undergoing proximal femoral fracture repair:A retrospective,observational study of effects on blood pressure,fluid administration and perioperative anaemia[J]. Anaesthesia,2011,66(11):1017-1022.
[16] White SM,Moppett IK,Griffiths R. Outcome by mode of anaesthesia for hip fracture surgery. An observational audit of 65535 patients in a national dataset[J]. Anaesthesia,2014,69(3):224-230.
[17] Herrera,De Andrés J,Esta?觡 L,et al. Hemodynamic impact of isobaric levobupivacaine versus hyperbaric bupivacaine for subarachnoid anesthesia in patients aged 65 and older undergoing hip surgery[J]. BMC Anesthesiol,2014,14(1):97.
[18] Benes J,Chytra I,Altmann P,et al. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients:Results of prospective randomized study[J].Crit Care,2010,14(3):R118.
[19] Charlson M,Szatrowski TP,Peterson J,et al. Validation of a combined comorbidity index[J]. J Clin Epidemiol,1994, 47(11):1245-1251.
[20] Quan H,Li B,Couris CM,et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries[J]. Am J Epidemiol,2011,173(6):676-682.
[21] Sachdev M,Sun JL,Tsiatis AA,et al. The prognostic importance of comorbidity for mortality in patients with stable coronary artery disease[J]. J Am Coll Cardio,2004, 43(4):576-582.
[22] Goldstein LB,Samsa GP,Matchar DB,et al. Charlson Index comorbidity adjustment for ischemic stroke outcome studies[J]. Stroke,2004,35(8):1941-1945.
[23] Frenkel WJ,Jongerius EJ,Mandjes-van Uitert MJ,et al. Validation of the charlson comorbidity index in acutely hospitalized elderly adults:A prospective cohort study[J]. J Am Geriatr Soc,2014,62(2):342-346.
[24] Erickson SR,Cole E,Kline-Rogers E,et al.The addition of the charlson comorbidity index to the GRACE risk prediction index improves prediction of outcomes in acute coronary syndrome[J]. Popul Health Manag,2014, 17(1):54-59.
(收稿日期:2019-07-05)
