术前LMR和FIB的检测对结直肠中分化腺癌患者的临床意义
2019-10-08朱婷樱鲍扬漪
朱婷樱 鲍扬漪
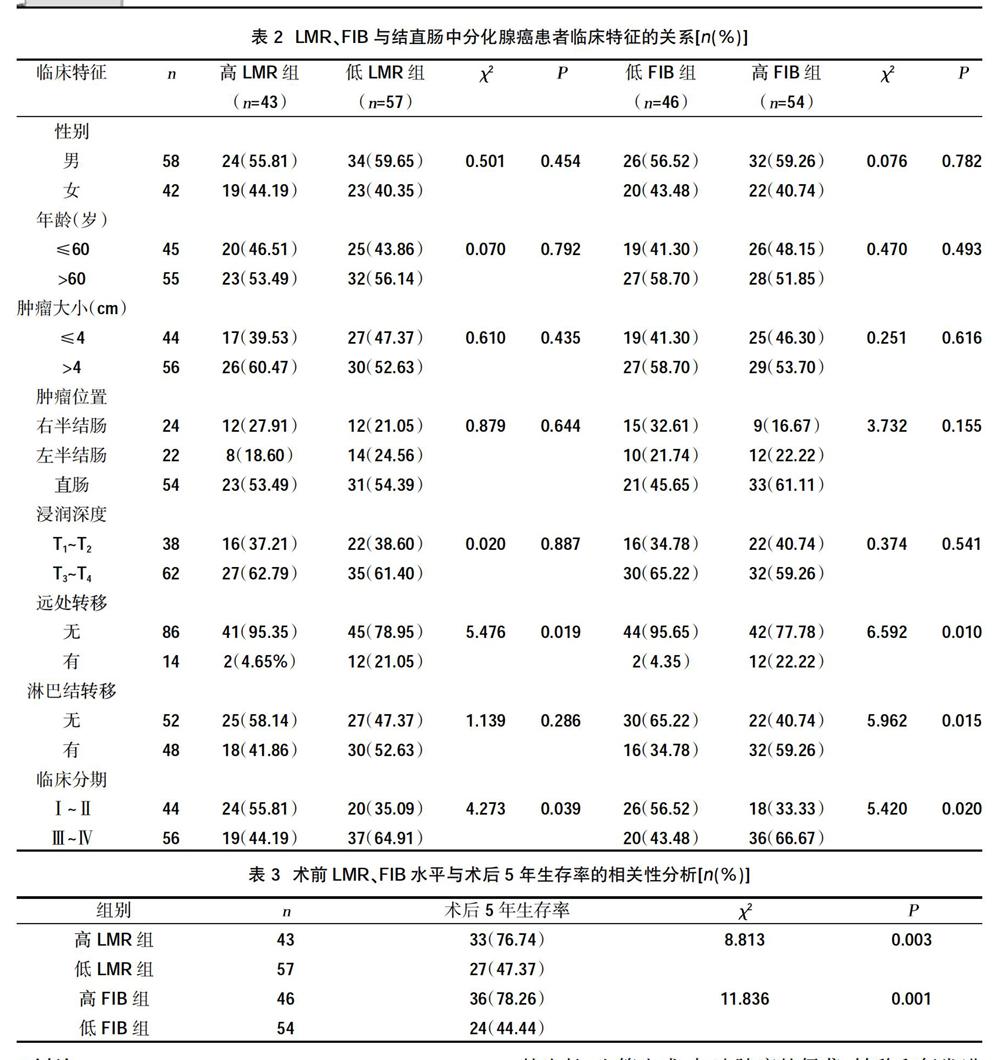
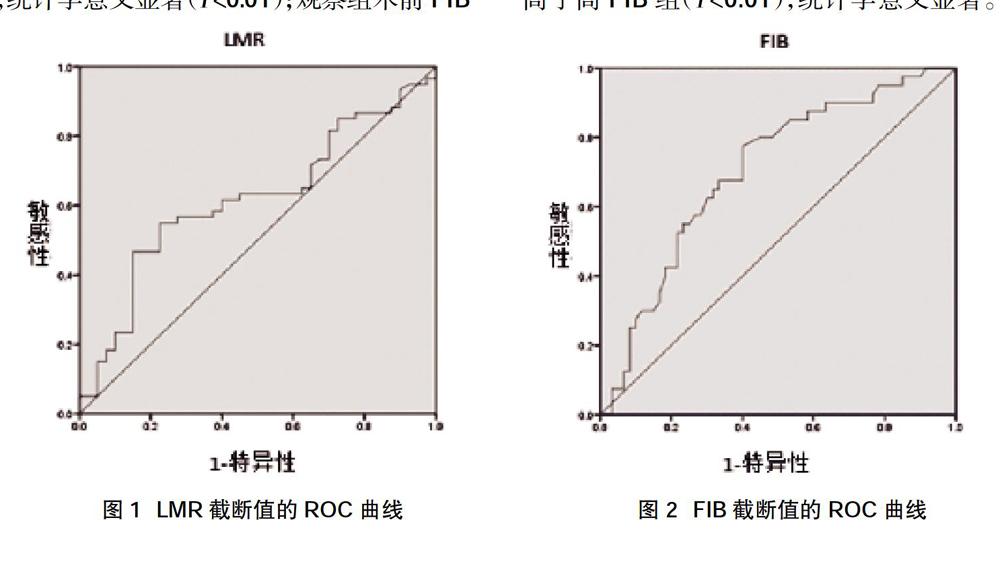
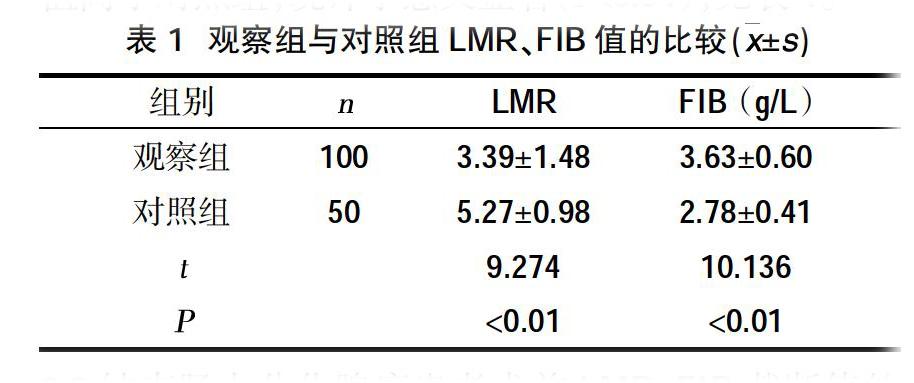
摘要:目的 探討结直肠中分化腺癌患者术前淋巴细胞与单核细胞比值和纤维蛋白原在辅助诊断、术前评估中的价值。方法 收集2010年1月~2013年7月在安徽医科大学第三附属医院接受手术治疗的结直肠中分化腺癌患者100例设为观察组,另选同时期健康体检者50例设为对照组,比较两组LMR、FIB值。通过受试者工作曲线确定结直肠中分化腺癌患者LMR与FIB的最佳截断值,根据截断值分为高、低LMR组,高、低FIB组。分析LMR、FIB与结直肠癌患者临床特征的关系及与术后5年生存率的相关性。结果 观察组LMR值(3.39±1.48)低于对照组(5.27±0.98),观察组FIB值(3.63±0.60)g/L高于对照组(2.78±0.41)g/L,统计学意义显著(P<0.01)。LMR、FIB的最佳截断值分别为3.65、3.495 g/L。高LMR组远处转移率为4.65%,低于低LMR组的21.05%,高LMR组在Ⅲ~Ⅳ期的比率为44.19%,低于低LMR组的64.91%,差异有统计学意义(P<0.05)。高FIB组远处转移率的22.22%,高于低FIB组的4.35%,高FIB组在Ⅲ~Ⅳ的比率为66.67%,高于低FIB组的43.48%,高FIB组淋巴结转移率为59.26%,高于低FIB组的34.78%,差异均有统计学意义(P<0.05)。高LMR组5年生存率为76.74%,高于低LMR组的47.37%,低FIB组5年生存率为78.26%,高于高FIB组的44.44%,统计学意义显著(P<0.01)。结论 术前LMR、FIB对结直肠中分化腺癌患者的辅助诊断、术前评估有一定临床价值。
关键词:结直肠中分化腺癌;淋巴细胞与单核细胞比值;纤维蛋白原;辅助诊断;术前评估
中图分类号:R753.3 文献标识码:A DOI:10.3969/j.issn.1006-1959.2019.04.031
文章编号:1006-1959(2019)04-0094-05
Abstract:Objective To investigate the value of preoperative lymphocyte and monocyte ratio and fibrinogen in the diagnosis and preoperative evaluation of patients with differentiated adenocarcinoma in colorectal. Methods 100 patients with colorectal differentiated adenocarcinoma who underwent surgery in the Third Affiliated Hospital of Anhui Medical University from January 2010 to July 2013 were enrolled in the observation group, and 50 healthy subjects in the same period were selected as the control group. The LMR and FIB values of the two groups were compared. The best cutoff values of LMR and FIB in patients with differentiated adenocarcinoma in colorectal were determined by receiver working curve. According to the cutoff value, they were divided into high and low LMR groups, high and low FIB groups. To analyze the relationship between LMR, FIB and clinical features of colorectal cancer patients and the correlation with 5-year survival rate. Results The LMR value of the observation group (3.39±1.48) was lower than that of the control group (5.27±0.98), and the FIB value of the observation group (3.63±0.60) g/L was higher than that of the control group (2.78±0.41) g/L, which was statistically significant (P <0.01). The optimal cutoff values for LMR and FIB are 3.650 and 3.495 g/L, respectively. The distant metastasis rate of the high LMR group was 4.65%, Below 21.05% of the low LMR group, the ratio of the high LMR group was 44.19% in the III~IV phase, which was lower than the 64.91% in the low LMR group, the difference was statistically significant (P<0.05). The distant metastasis rate was 22.22% in the high FIB group,Compared with 4.35% in the low FIB group, the ratio of III to IV in the high FIB group was 66.67%, which was higher than 43.48% in the low FIB group, and the lymph node metastasis rate in the high FIB group was 59.26%, which was higher than that in the low FIB group 34.78%,the differences were statistically significant (P<0.05). The 5-year survival rate was 76.74% in the high LMR group, which was higher than the low LMR group 47.37%, and the 5-year survival rate was 78.26% in the low FIB group, which was higher than that in the high FIB group 44.44%,Statistically significant (P <0.01). Conclusion Preoperative LMR and FIB have certain clinical value in the auxiliary diagnosis and preoperative evaluation of patients with differentiated adenocarcinoma in colorectal cancer.
Key words:Differentiated adenocarcinoma in colorectal;Lymphocyte to monocyte ratio;Fibrinogen; Assisted diagnosis;Preoperative evaluation
結直肠癌(colorectal cancer,CRC)已被公认为全球第3大最常见癌症[1]。随着人口老龄化、作息及饮食习惯的改变,结直肠癌的发病率及死亡率日益增加。我国结直肠癌的发病率占癌症总人数的第5位,死亡率占第5位,严重威胁着人类的健康安全[2]。越来越多的研究证实肿瘤相关炎症反应对肿瘤的发生发展起着重要作用[3]。炎症反应主要表现为白细胞总数及各亚群比例的变化,其中淋巴细胞及单核细胞在此过程中发挥着重要作用。有研究证实外周血淋巴细胞与单核细胞绝对值的比值(LMR)下降与食管癌、胃癌等多种消化系统肿瘤[4,5]、弥漫大B细胞淋巴瘤[6]、恶性胸膜间皮瘤[7]的预后不佳有关,且凝血级联反应在肿瘤的进展及转移中也起着重要的作用[8]。FIB是凝血过程中的主要组成成分,研究显示FIB水平的升高往往与肿瘤患者预后不良有关,且患者外周FIB值可协助直肠癌诊断,并为病情评估提供参考[9]。以往研究多为单独探讨LMR或FIB与结直肠癌之间的关系,很少有文献将二者联合。本研究旨在评估术前LMR和FIB在结直肠中分化腺癌患者辅助诊断、术前评估中的临床价值。
1资料与方法
1.1一般资料 收集2010年1月~2013年7月安徽医科大学第三附属医院(合肥市第一人民医院及合肥市滨湖医院)接受手术治疗的结直肠癌患者为研究对象。本研究经医院伦理委员会审批通过,患者及家属知情同意并签署同意书。纳入标准:①年龄42~82岁;②影像学、结直肠镜等诊断为结直肠癌并已行手术治疗,术后病理证实为结直肠中分化腺癌;③术前未接受任何新辅助放化疗。④术后均行辅助放化疗。排除标准:①患有血液系统疾病、自身免疫系统疾病、肝病和近期感染者;②近期使用抗凝药物及其他影响血常规结果的药物;③合并其他肿瘤或消化系统疾病等慢性疾病患者;④临床资料不完整。共纳入100例结直肠癌患者,随机选取同期50例相同年龄段的健康体检者设为正常对照组。
1.2方法 收集两组研究对象性别、年龄等一般资料及血液学指标,血液学指标包括淋巴细胞绝对值、单核细胞绝对值、FIB值,患者均为术前3 d内抽取,对照组为体检时抽取;收集观察组的病理资料,包括肿瘤大小、淋巴结转移、远处转移、浸润深度、肿瘤位置、TNM分期。肿瘤分期第8版TNM分期确定;以首次治疗作为观察起点,对治疗后的患者采用电话、门诊、住院方式进行随访,随访截止日期为术后5年或术后5年期间死亡的时间。
1.3统计学方法 采用SPSS 22.0软件进行统计学分析。计量资料用(x±s)表示,组间比较用t检验;计数资料用(%)表示,组间比较用χ2检验。采用ROC曲线确定LMR、FIB最佳截断值,兼顾敏感性及特异性。以P<0.05认为差异有统计学意义,P<0.01认为统计学意义显著。
2结果
2.1两组LMR、FIB值的比较 观察组术前LMR值低于对照组,统计学意义显著(P<0.01);观察组术前FIB值高于对照组,统计学意义显著(P<0.01),见表1。
2.2结直肠中分化腺癌患者术前LMR、FIB截断值的确定与分组 在ROC曲线分析中,术前LMR的理想截断值为3.65(AUC:0.618,95%CI:0.506~0.729,P<0.05),敏感度为55.00%,特异度为77.50%,见图1。由此将入组病例分为两组,即高LMR组(LMR≥3.65,n=43)和低LMR组(LMR<3.65,n=57)。FIB的理想截断值为3.495 g/L(AUC:0.703,95% CI:0.600~0.807,P<0.01),敏感性为77.50%,特异度为60.00%,见图2。将病例分为两组,即低FIB组(FIB≤3.495 g/L,n=46),高FIB组(FIB>3.495 g/L,n=54)。将FIB及LMR联合后,其特异性为87.50%,敏感性为61.70%。
2.3 LMR、FIB与结直肠中分化腺癌患者临床特征的关系 LMR与远处转移、临床分期成负相关,差异有统计学意义(P<0.05);与性别、年龄、肿瘤大小、肿瘤位置、肿瘤浸润深度、淋巴结转移无相关,差异无统计学意义(P>0.05)。FIB与远处转移、临床分期、淋巴结转移成正相关,差异有统计学意义(P<0.05);与性别、年龄、肿瘤位置、肿瘤大小、肿瘤浸润深度无相关,差异无统计学意义(P>0.05),见表2。
2.4术前LMR、FIB值与术后5年生存率的相关性分析 100例结直肠中分化腺癌患者5年生存率为60.00%,其中高LMR组为76.74%,低LMR组为47.37%,高LMR组的5年生存率高于低LMR组,统计学意义显著(P<0.01)。低FIB组5年生存率为78.26%,高FIB组为44.44%,低FIB组5年生存率高于高FIB组(P<0.01),统计学意义显著。见表3。
3讨论
虽然结直肠癌的诊断及治疗取得了重大进展,但其早期诊断率和生存率仍不能令人满意。准确的术前评估是为患者制定更为合适的治疗方案的基础,从而能提高患者的生存率。传统影像学检查如CT检查和超声虽能评估疾病的进展情况,但对较小和隐匿的淋巴结转移则难以检出,对微小远处转移病灶的检出率也较低,故寻找可辅助常规诊断的生物学标志分子或指标极为关键。
有研究证实,炎症相关细胞如淋巴细胞、单核细胞等在肿瘤的发生、发展和预后中发挥着重要作用[10,11]。此类细胞可释放细胞因子进入肿瘤微环境(tumor microenvironment,TME),从而促进肿瘤细胞的生长、血管生成,加速肿瘤的侵袭、转移和复发进程[12]。其中,淋巴细胞是机体免疫应答过程中的主要效应细胞,淋巴细胞直接攻击肿瘤细胞可能是阻止肿瘤生长的最有效机制,淋巴细胞和肿瘤细胞之间的接触更好地激活了分子信号来控制肿瘤的侵袭性,肿瘤浸润淋巴细胞(TILs)的存在与良好的临床进程有关,并被认为是几种癌症的积极预后因素[13,14]。外周血单核细胞浸润到肿瘤组织后,可以转变为肿瘤相关巨噬细胞,并分泌血管内皮生长因子(VEGF)、基质金属蛋白(MMP)等细胞因子,从而促进肿瘤新生血管的形成、肿瘤细胞的侵袭和增殖,同时抑制抗肿瘤免疫[15],促进肿瘤的进展及免疫逃逸发生。淋巴细胞绝对数高对患者有一定的保护作用,而单核细胞计数高则相反,此两者的比值可能反映肿瘤的发生及进展状态。LMR是一种全身炎症指数,其计算方法是淋巴细胞计数与单核细胞计数的比值。既往研究证实,LMR与肿瘤的临床表现及预后均相关。
本研究结果提示,观察组LMR值水平低于对照组,统计学意义显著(P<0.01)。高LMR组远处转移率(4.65%)低于低LMR组(21.05%),高LMR组在Ⅲ-Ⅳ期的比率(44.19%)低于低LMR组(64.91%),差异有统计学意义(P<0.05),这与周超等[16]、Yang J等[17]的报道相似。且高LMR组的5年生存率(76.74%)高于低LMR组(47.37%),统计学意义显著(P<0.01),与周超等[16]的报道一致,说明LMR可能与肿瘤的进展与预后相关,可用于术前辅助评估。
FIB是一种急性期反应蛋白,主要由肝脏合成并分泌,最近有研究证实肿瘤细胞也可分泌FIB[18],在肿瘤细胞与基质的联系中发挥着重要作用。FIB作为血管内皮生长因子等生长因子结合的支架,可促进肿瘤细胞增殖、转移和粘附[19]。当纤维蛋白原转化为纤维蛋白后,可参与转移和新生血管的形成,且其在肿瘤组织周围可保护肿瘤细胞免受自然杀伤细胞的破坏[20]。研究证实,胃癌[21]及非小细胞肺癌[22]患者FIB水平的升高与疾病的严重程度成正比,与生存率成反比。本研究结果显示,观察组FIB值高于对照组,统计学意义显著(P<0.01)。FIB与临床特征的相关性分析结果显示,患者术前FIB水平与远处转移、临床分期、淋巴结转移成正相关,差异有统计学意义(P<0.05),这与Tang L等[23],覃罗等[24]报道相似,且低FI对照组的5年生存率(78.26%)高于高FI对照组(44.44%),统计学意义显著(P<0.01),说明FIB也可用于术前评估,且其评估淋巴结转移方面可能优于LMR。
本研究显示,观察组的LMR值低于对照组,观察组的 FIB值高于对照组,LMR、FIB与5年生存率密切相关,且与癌细胞转移以及临床分期有一定关联,说明LMR、FIB均可作为结直肠中分化腺癌患者辅助诊断、术前评估的指标。本研究将二者联合后,发现其特异性(87.50%)更高,敏感性(61.70%)也较高。故单独或联合检测LMR、FIB对结直肠癌辅助诊断和评估病情进展、预后有一定的临床价值,且其方便、痛苦少、可靠、经济、重复性好,可广泛应用于临床。但本研究为回顾性研究,且样本量较小,可能对结果产生一定影响,故还需进一步前瞻性研究或扩大样本量来证实。
综上所述,术前LMR、FIB对结直肠中分化腺癌患者的辅助诊断、术前评估有一定价值,能为是否需要进行术前辅助放化疗及术前治疗方案的制定等提供一定的参考,从而提高患者的生存率。
参考文献:
[1]Jemal A.Cancer statistics,2015[J].Ca A Cancer Journal for Clinicians,2015,60(5):277-300.
[2]Chen W,Zheng R,Baade PD,et al.Cancer statistics in China,2015.[J].Ca A Cancer Journal for Clinicians,2016,66(2):115-132.
[3]O'Malley G,Treacy O,et al.Stromal cell PD-L1 inhibits CD8+ T-cell antitumor immune responses and promotes colon cancer[J].Cancer Immunol Res,2018,6(11):1426-1441.
[4]Han LH,Jia YB,Song QX,et al.Prognostic significance of preoperative lymphocyte-monocyte ratio in patients with resectable esophageal squamous cell carcinoma[J].Asian Pac J Cancer Prev,2015,16(6):2245-2250.
[5]Lieto E,Galizia G,Auricchio A,et al.Preoperative neutrophil to lymphocyte ratio and lmphocyte to monocyte ratio are prognostic factors in gastric cancers undergoing surgery[J].J Gastrontest surg,2017,21(11):1764-1774.
[6]Li YL,Pan YY,Jiao Y,et al.Peripheral blood lymphocyte/monocyte ratio predicts outcome for patients with diffuse large B cell lymphoma after standard first-line regimens[J].Annals of Hematology,2014,93(4):617-626.
[7]Yamagishi T,Fujimoto N,Nishi H,et al.Prognostic significance of the lymphocyte-to-monocyte ratio in patients with malignant pleural mesothelioma[J].Lung Cancer,2015,90(1):111-117.
[8]周建剛,邵荣.术前癌胚抗原、D-二聚体、纤维蛋白原水平与结直肠癌患者临床病理学特征及分期的相关性研究[J].国际消化病杂志,2017(5):330-333.
[9]Pichler M,Hutterer GC,Stojakovic T,et al.High plasma fibrinogen level represents an independent negative prognostic factor regarding cancer-specific,metastasis-free,as well as overall survival in a European cohort of non-metastatic renal cell carcinoma patients[J].British Journal of Cancer,2013,109(5):1123-1129.
[10]Tsai YD,Wang CP,Chen CY,et al.Pretreatment circulating monocyte count associated with poor prognosis in patients with oral cavity cancer[J].Head Neck,2014,36(7):947-953.
[11]Tuting T,de Visser KED.How neutrophils promote metastasis[J].Science,2016,352(6282):145-146.
[12]Qu X,Tang Y,Hua S.Immunological Approaches Towards Cancer and Inflammation A Cross Talk[J]. Frontiers in Immunology,2018(9):563.
[13]Mandarano M,Bellezza G,Belladonna ML,et al.Assessment of TILs,IDO-1,and PD-L1 in resected non-small cell lung cancer:an immunohistochemical study with clinicopathological and prognostic implications[J].Virchows Archiv,2018:1-10.
[14]Zeng DQ,Yu YF,Ou QY,et al.Prognostic and predictive value of tumor-infiltrating lymphocytes for clinical therapeutic research in patients with non-small cell lung cancer[J].Oncotarget,2016,7(12):13765-13781.
[15]Chen X,Wu J,Ying L,et al. Prognostic Significance of Pre-Operative Monocyte-to-Lymphocyte Ratio in Lung Cancer Patients Undergoing Radical Surgery[J].Laboratory Medicine,2018, 49(2):29-39.
[16]周超,闫军浩,唐坚,等.淋巴细胞单核细胞比值与结直肠癌临床特征及预后的相关性分析[J].肿瘤,2017,37(12):1297-1303.
[17]Yang J,Xu H,Guo X,et al.Pretreatment Inflammatory Indexes as Prognostic Predictors for Survival in Colorectal Cancer Patients Receiving Neoadjuvant Chemoradiotherapy[J].Scientific Reports,2018,8(1):3044.
[18]Sahni A,Simpsonhaidaris PJ,Sahni SK,et al.Fibrinogen synthesized by cancer cells augments the proliferative effect of fibroblast growth factor-2 (FGF-2)[J].Journal of Thrombosis & Haemostasis,2010,6(1):176-183.
[19]Chen P,Wang C,Cheng B,et al.Plasma fibrinogen and serum albumin levels (FA score) act as a promising prognostic indicator in non-small cell lung cancer[J]. Oncotargets & Therapy,2017 (10):3107-3118.
[20]Huang W,Wang S,Zhang H,et al.Prognostic significance of combined fibrinogen concentration and neutrophil-to-lymphocyte ratio in patients with resectable non-small cell lung cancer[J]. Cancer Biology & Medicine,2018,15(1):88-96.
[21]Lee SE,Lee JH,Ryu KW,et al.Preoperative plasma fbrinogen level is a useful predictor of adjacent organ involvement in patients with advanced gastric cancer[J].Gastric Cancer,2012(12): 81-87.
[22]Li Y,Wei S,Wang J,et al.Analysis of the factors associated with abnormal coagulation and prognosis in patients with non-small cell lung cancer[J].Zhongguo Fei Ai Za Zhi,2014,17(11):789-796.
[23]Tang L,Liu K,Wang J,et al.High preoperative plasma fibrinogen levels are associated with distant metastases and impaired prognosis after curative resection in patients with colorectal cancer[J].Journal of Surgical Oncology,2010,102(5):428-432.
[24]覃羅,姚晖,徐亮,等.中性粒细胞与淋巴细胞比值联合检测纤维蛋白原对结直肠癌预后的判断价值[J]. 中国免疫学杂志,2017,33(4):527-532.
收稿日期:2018-11-24;修回日期:2018-12-2
编辑/肖婷婷
