乳腺导管内癌的X线表现与分子分型的对照研究
2017-08-22黄社磊马捷蒋华景
黄社磊+马捷+蒋华景
[摘要] 目的 探討乳腺导管内癌的X线表现与分子分型的关系。 方法 回顾性分析133例136侧DCIS的X线表现及组织病理学、免疫组织化学结果。 结果 (1)136侧乳腺导管内癌X线表现为单纯钙化(32.4%)、钙化伴局灶性不对称/肿块(29.4%),钙化出现率61.8%。钙化形态以细小多形性(58.3%)、段样分布多见(54.8%);形态分布组合以细小多形性钙化成簇分布多见。肿块的形态多为不规则形(62.5%)、边缘模糊(43.8%)、高密度(75%)。(2)DCIS以Luminal A型多见,Her-2过表达型次之。(3)ER/PR(+)、Her-2(-)X线表现单纯钙化多见35.6%、34.6%,形态为细小多形性68.6%、71.7%、成簇分布52.9%、52.2%;ER/PR(-)、Her-2过表达多表现为钙化伴局灶性不对称/肿块38.8%、36.2%,钙化形态前者为细小多形性57.6%、段样分布69.7%,后者为线样分支状52.6%、段样分布65.8%。(4)Ki-67增殖指数≤10%时,83.3%ER(+)、80.6%Her-2(-),钙化形态多为细小多形性(88.2%);当Ki-67增殖指数>31%时,56.4%ER(+)、48.7%Her-2(-),钙化形态为线样分支状48.3%。 结论 DCIS分子分型以Luminal A型多见。X线以钙化为主要表现,形态多为细小多形性、线样分支状;分布以段样及成簇多见。钙化的分布、形态及形态分布组合与ER、PR、Her-2及Ki-67增殖指数有关。
[关键词] 数字化乳腺X线摄影;癌;导管;激素受体;人表皮生长因子受体;分子分型
[中图分类号] R737.9 [文献标识码] A [文章编号] 2095-0616(2017)13-13-04
[Abstract] Objective To explore the relationship the X-ray appearance and molecule subtype of the Breast DCIS (Ductal Carcinoma In Situ,DCIS),in order to know more about them. Methods The main X-ray appearance,histopathology and immunhistochemistry of the 133 cases DCIS (all 136 latero-breast) were retrospectively analyzed. Results (1)The main X-ray appearance of the 136 laterals DCIS were calcification 32.4%,calcification with focal dissymmetry/mass 29.4%,the frequency of calcification of all cases was 61.8%.The main morphous and distribution of calcifications was fine pleomorphic calcifications 58.3% and segmental 54.8% respectively,the main combination of morphous and distribution of calcifications was clustering fine pleomorphic calcifications.The appearance of the mass were irregular 62.5%,ambigutiy boundary 43.8%,high density 75%.(2)The molecule subtype of the Luminal A was the most frequent found in the different grade DCIS.(3)The main X-ray appearance of the ER/PR(+) and Her-2(-) DCIS were purely calcifications (35.6% vs 34.6%),the appearance of calcifications of them were fine pleomorphic calcifications (68.6% vs 71.7%),cluster(52.9% vs 52.2%).However,the main X-ray appearance of the ER/PR(-) and Her-2(+) DCIS were calcification with focal dissymmetry/mass (38.8% vs 36.2%),the appearance of calcifications the ER/PR(-)DCIS were fine pleomorphic (57.6%),segment (69.7%).While the Her-2(+) DCIS were linear branching (52.6%),segment (65.8%).(4)The proliferation index of the Ki-67≤10%,the proportion of ER(+) and Her-2(-) DCIS were 83.3% vs 80.6%,and the morphous of calcification was fine pleomorphic calcifications (88.2%).While the proliferation index of the Ki-67>31%,the proportion of ER (+) and Her-2(-) DCIS were 56.4% vs 48.7%,and the morphous of calcification was linear branching (48.3%). Conclusion The Luminal A is the most frequent found in the molecule subtypes of the DCIS.The main X-ray appearance of the DCIS is calcifications,the main morphous of the calcifications are fine pleomorphic and linear branching,the main distrutions of them are segment and clustered.The morphous,distrutions,combination of the morphous and distrutions of the calcifications are relevanted with ER, PR, Her-2 and the proliferation index of the Ki-67.
[Key words] Digital mammographic screening;Carcinoma;Duct;Hormone receptors;Her-2;Molecular typing
乳腺导管内癌(ductal carcinoma in situ,DCIS)是局限于导管内基底膜内而不侵犯间质的一类乳腺导管上皮细胞恶性增生,约占全部乳腺癌的20%,影像学(X线等)的发展和广泛应用显著提高了DCIS的检出率[1]可根据雌激素受体(ER)、孕激素受体(PR)、人类上皮生长因子(HER-2)的表达水平以及细胞增殖指数(Ki-67)将乳腺癌划分为4类分子亚型:包括Luminal A型、Luminal B型、HER-2阳性和三阴性乳腺癌,分子分型与乳腺癌治疗和预后具有密切关系[2]。本研究分析DCIS的X线各种表现,重点观察在钙化方面的X线形态及分布表现,探讨其与分子分型之间的联系。
1 资料与方法
1.1 一般资料
回顾性分析133例我院于2010年1月~2016年12月期间收治的DCIS女性患者的临床资料。纳入标准:(1)经手术病理组织检查确诊为DCIS;(2)患者临床资料及X线、术后病理资料完整。排除标准:(1)接受放化疗治疗;(2)合并浸润性导管癌;(3)合并其他类型肿瘤。本研究经我院医学伦理委员会审核通过,所有患者均知情同意。
1.2 仪器与方法
采用飞利浦数字化乳腺X线机(Digital Mammography,DM),由两位具有10年以上X线图像诊断经验的医师进行双盲法阅片,X线表现根据美国放射学会的乳腺影像报告和数据系统2003年第四版(BI-RADS分类)[2]标准分为:(1)主要征象:①肿块:形态、边缘及密度;②钙化:形态、分布;③钙化伴肿块;④结构扭曲;⑤特殊征象;⑵相关征象包括:局部血运增加、病变结构扭曲、乳头及皮肤回缩、相邻皮肤增厚、腋窝淋巴结肿大等。记录患者主要征象和相关征象。
1.3 病理学诊断
根据病理组织切片中细胞核的异型性、核分裂、管腔内坏死程度将DCIS划分为低、中、高病变级别。应用4种标记免疫组化雌激素受体(ER)、孕激素受体(PR)、人类上皮生长因子(HER-2)及细胞增殖指数(Ki-67)将乳腺癌划分为4类分子亚型:包括Luminal A型、Luminal B型、HER-2阳性和三阴性乳腺癌。
1.4 统计学处理
采用SPSS19.0软件进行统计学处理和分析,计数资料采用百分比表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1 一般情况
133例患者,年龄24~79岁。体格检查结果:肿块67侧,乳头溢液10侧,其中血性溢液7侧,检查前触诊阴性59侧。前哨淋巴结有转移4侧、腋窝淋巴结转移7侧。
2.2 病理结果
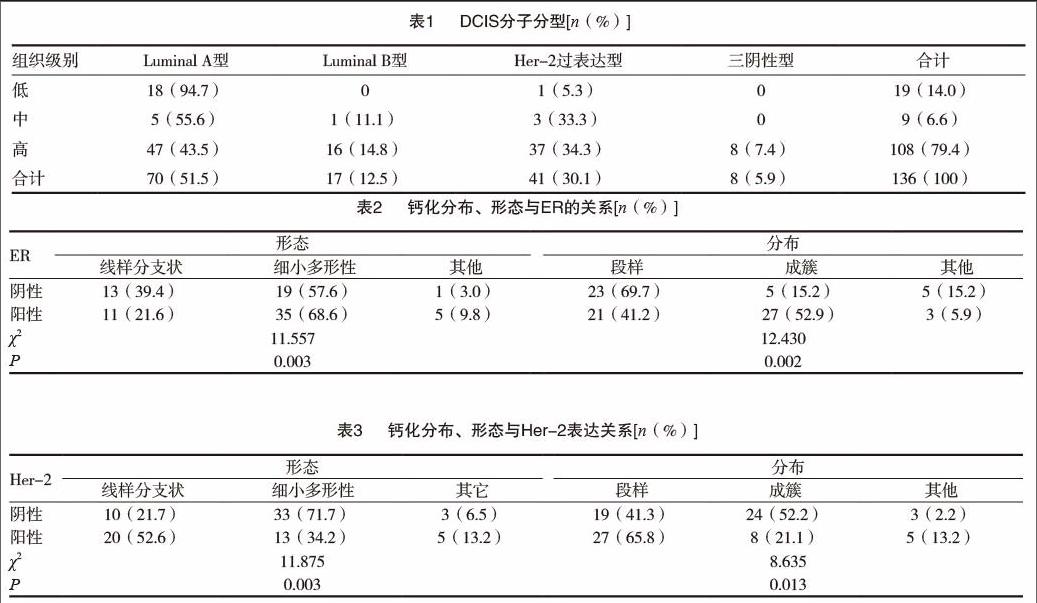
三种组织级别分子分型结果差异有统计学意义(χ2=17.731,P=0.007),低级别病变组织Luminal A型比例显著高于中高级别,三阴性型均为高级别病变。见表1。
2.3 X线表现
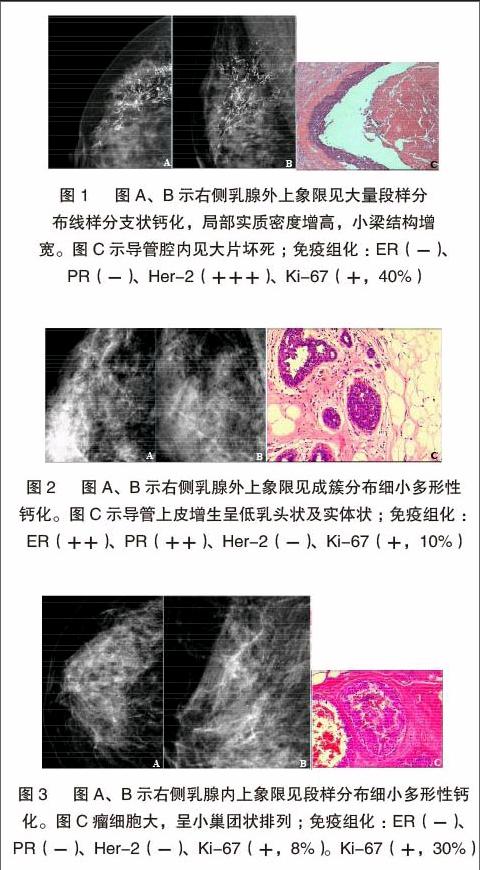
(1)钙化伴局灶性不对称/肿块40例(29.4%)、单纯钙化44例(32.4%)。钙化形态:细小多形性49例(58.3%)、线样分支状30例(35.7%);段样分布46例(54.8%)、成簇分布30例(35.7%);形态分布组合多以细小多形性钙化成簇分布,有23例(27.7%),以段样分布的细小多形性钙化22例(26.5%)。形态:不规则形20例(62.5%),椭圆形7例(21.9%),肿块边缘模糊14例(43.8%)、毛刺状表现8例(25%);密度:高密度24例(75%)、等密度7例(21.9%)。(2)单纯钙化多见于三阴性、Luminal A型及Luminal B型乳腺癌,钙化伴局灶性不对称/肿块为主要表现见于Her-2阳性乳腺癌,差异无统计学意义(P>0.05)。(3)单纯钙化多见于ER/PR阳性者(36%),此类患者钙化形态以细小多形性钙化成簇多见(占42.3%),其次为单纯肿块(25.3%);钙化伴局灶性不对称/肿块多见于ER/PR阴性者(占38%),其次表现为单纯钙化(26%);钙化形态分布多以线樣分支状钙化段样分布为主(45.2%),此类差异有统计学意义(P<0.05)。因此,得出结论:钙化的分布及形态与Her-2及ER/PR的表达有关,见下表2 ~ 3及图1 ~ 3。(4)当细胞增殖指数(Ki-67)≤10%时,83.8%ER表现为阳性、81.1%Her-2表现为阴性;当细胞增殖指数(Ki-67)>30%时,56.4%ER表现为阳性、48.7%Her-2表现为阴性,差异有统计学意义(P<0.05)。
3 讨论
目前对DCIS的病程演变的认识还不是很透彻。相关文献报道,低级别DCIS的女性中有14%~60%的患者可进展为浸润性乳腺癌。由于DCIS患者在治疗过程中多采取了相关干预措施,因此尚不清楚高级别DCIS女性进展为浸润性乳腺癌的风险度[3]。研究表明,钙化是DCIS患者最主要的X线表现,细小多形性钙化、线样或线样分支状钙化是其主要征象[4]。极少数(约5%)的患者是在因其他原因进行乳腺手术切除标本中偶然发现。DCIS的组织学分型能够用来预测经保守治疗乳腺癌患者复发风险,并用来评估保乳手术的临床疗效,Wang[5]等研究认为X线、分子分型与肿瘤标记物等联合应用能提高对DCIS患者预后的评估,并给予个体化治疗方案。本研究表明,DCIS患者钙化灶的形成与肿瘤细胞的分泌、变性及坏死后的钙盐沉积具有一定相关性,钙化形态与病理分型及其预后亦存在有相关性。研究数据提示线样钙化通常预示发生高级别的浸润性癌的风险较高,患者预后也较差[6-8]。Muttarak[9] 等认为,段样分布的线样或线样分支状钙化常见于高级别 DCIS中;单发或多发成簇分布的细小多形性钙化常见于中级别DCIS中;成簇分布的细点状钙化常见于低级别DCIS中。本研究也表明,钙化的形态、分布及形态分布组合与ER/PR、Her-2表达有关,差异有统计学意义(P<0.05)。ER/PR(+)钙化形态为细小多形性(69.2%)、成簇分布(51.9%);ER/PR(-)为细小多形性(59.4%)、段样分布(75%)。Her-2(-)患者中,钙化为细小多形性(67.3%),成簇分布(80%),Her-2(+)为线样分支状66.7%、段样分布多见(58.7%)。ER/PR(弱+)及Her-2(强+)与段样分布线样分支状钙化的出现有关;若ER/PR(-),Her-2(强+)与线样分支状钙化有关。
Tanei[10]等研究认为ER/PR与Ki-67的表达负相关,表明肿瘤内分泌的治疗效果不理想,细胞增殖指数Ki-67较大时与较差的临床治疗结果相关。本研究中,Ki-67增殖指数与ER/PR、Her-2表达差异无统计学意义(P>0.05),但与钙化形态、分布有关,差异有统计学意义(P<0.05)。当Ki-67增殖率≤10%时,83.3%ER(+)、80.6%Her-2(-),细小多形性钙化形态(占88.2%);当Ki-67增殖率为>30%时,56.4%ER(+)、48.7%Her-2(-),线样分支状钙化形态(占48.3%)。提示细小多形性钙化、ER(+)与低细胞增殖指数Ki-67相关。
大多数学者将ER(-)/Her-2(强+)与ER(-)/Her-2(-)DCIS对比研究发现,前者更易出现微小钙化,同时在ER(-)DCIS中,肿块的边缘、出现的钙化及肿瘤分期和Her-2表达的情况密切相关[11-16]。本研究显示ER(-)/Her-2强+)与ER(-)/Her-2(-)DCIS的出现钙化率分别为63.4%(26/41)、75%(6/8),与相关文献报道不一致,究其原因,笔者认为可能与ER(-)/Her-2(-)病例过少有一定关系。
总之,DCIS大多以细小多形性钙化为主,不同病理分子分型的DCIS患者,其X线表现也不一样。本研究表明,DCIS钙化的分布及形态可以反映PR、ER、、Her-2及Ki-67的表达情况;X线表现以单纯细小多形性钙化为主并呈成簇分布时,预示着ER/PR(+)、Her-2(-)及细胞增殖指数Ki-67较低可能。而钙化为线样分支状并段样分布的出现,提示ER/PR(-)、Her-2(强+)及细胞增殖指数Ki-67较高可能。通过对DCIS钙化分布及形态的全面、仔细地分析,对推断其病理分型、为临床提供治療方案信息及评估患者预后具有较高应用价值。
[参考文献]
[1] Virnig BA,Tuttle TM,Shamliyan T,et al.Ductal carcinoma in situ of the breast:a systematic review of incidence,treatment,and outcomes[J].J Natl Cancer Inst,2010,102(3):170-178.
[2] Radiology ACO.Breast imaging reporting and data system (BI-RADS)[M].American College of Radiology,2003.
[3] Vaidya Y,Vaidya P,Vaidya T.Ductal Carcinoma In Situ of the Breast[J].Indian Journal of Surgery,2015,77(2):1-6.
[4] Evans A,Clements K,Maxwell A,et al.Lesion size is a major determinant of the mammographic features of ductal carcinoma in situ: findings from the Sloane project[J].Breast Cancer Research,2008,65(3):181-184.
[5] Wang X,Chao L,Chen L,et al.Correlation of mammographic calcifications with Her-2/neu overexpression in primary breast carcinomas[J].Journal of Digital Imaging,2008,21(2):170-176.
[6] Stomper PC,Geradts J,Edge SB,et al.Mammographic predictors of the presence and size of invasive carcinomas associated with malignant microcalcification lesions without a mass[J].Ajr American Journal of Roentgenology,2003,181(6):1679-1684.
[7] Tabár L,Chen HH,Duffy SW,et al.A novel method for prediction of long-term outcome of women with T1a,T1b,and 10-14 mm invasive breast cancers:a prospective study[J].Lancet,2000,355(9202):429-433.
[8] Berg WA,Arnoldus CL,Teferra E,et al.Biopsy of amorphous breast calcifications:pathologic outcome and yield at stereotactic biopsy[J].Radiology,2001,221(2):495-503.
[9] Muttarak M,Kongmebhol P,Sukhamwang N.Breast calcifications:which are malignant?[J].Singapore Medical Journal,2009,50(9):907.
[10] Tanei T,Shimomura A,Shimazu K,et al.Prognostic significance of Ki67 index after neoadjuvant chemotherapy in breast cancer[J].European Journal of Surgical Oncology the Journal of the European Society of Surgical Oncology & the British Association of Surgical Oncology,2011,37(2):155.
[11] Shin HJ,Kim HH,Huh MO,et al.Correlation between mammographic and sonographic findings and prognostic factors in patients with node-negative invasive breast cancer[J].British Journal of Radiology,2011,84(997):19.
[12] Ayadi L,Khabir A,Amouri H,et al.Correlation of HER-2 over-expression with clinico-pathological parameters in Tunisian breast carcinoma[J].World Journal of Surgical Oncology,2008,6(1):1-8.
[13] Ko ES,Lee BH,Kim HA,et al.Triple-negative breast cancer:correlation between imaging and pathological findings[J].European Radiology,2010,20(5):1111-1117.
[14] Almasri NM,Hamad MA.Immunohistochemical evaluation of human epidermal growth factor receptor 2 and estrogen and progesterone receptors in breast carcinoma in Jordan[J].Breast Cancer Research,2005,7(5):R598.
[15] Huang HJ,Neven P,Drijkoningen M,et al.Hormone receptors do not predict the HER2/neu status in all age groups of women with an operable breast cancer[J].Annals of Oncology,2005,16(11):1755-1761.
[16] Seo BK,Pisano ED,Kuzimak CM,et al.Correlation of HER-2/neu overexpression with mammography and age distribution in primary breast carcinomas[J].Academic Radiology,2006,13(10):1211-1218.
(收稿日期:2017-05-02)
