单发局灶球形肺炎的CT表现特征及鉴别诊断价值
2016-07-19王宗会彭如臣
王宗会,彭如臣
·论著·
单发局灶球形肺炎的CT表现特征及鉴别诊断价值
王宗会,彭如臣
063100 河北省唐山市,开滦(集团)有限责任公司唐家庄医院放射科(王宗会);首都医科大学附属北京潞河医院医学影像中心(彭如臣)
【摘要】目的探讨单发局灶球形肺炎(SLSP)的CT表现特征及鉴别诊断价值,以进一步提高本病的影像诊断水平。方法搜集2006年8月—2015年1月于开滦(集团)有限责任公司唐家庄医院临床、手术病理证实且符合纳入与排除标准的54例SLSP患者的临床资料。观察并分析患者CT表现特征(包括病灶部位、形态、边缘、大小、密度,邻近胸膜改变,肺门侧表现,病灶侧缘肺野表现)及抗炎治疗后动态变化。结果CT表现特征:38例(70.4%)患者病灶部位为双肺下叶后外基底段及背段;46例(85.2%)患者病灶呈楔形,其中34例(73.9%)呈类方形征,9例(19.6%)呈山丘状,3例(6.5%)呈三角形;41例(75.9%)可见毛糙的长毛刺,13例(24.1%)肺窗周围为模糊的带状低密度影,呈晕征;病灶直径2.0~7.5 cm,平均病灶直径3.9 cm;30例(55.6%)病灶密度均匀;48例(88.9%)病灶与胸膜相贴,其中41例周围胸膜均匀性增厚;30例(55.6%)显示局部充血征,17例(31.5%)病变相对应支气管壁略增厚;20例(37.0%)病灶侧缘邻近肺野内可见小斑片状渗出灶。49例(90.7%)患者接受抗炎治疗,其中47例(95.9%)经抗炎治疗后症状减轻、消失,2例(4.1%)抗结核治疗效果不良,再行抗感染治疗病灶消散、吸收;5例(9.3%)手术切除。结论SLSP主要位于双肺下叶后外基底段或背段,以贴近胸膜面常见,表现为楔形或类圆形,边缘多为毛糙的长毛刺或模糊的晕征;可见肺门侧血管、支气管局部充血征,病灶侧缘的小片状炎性渗出表现。贴近胸膜者,胸膜以较广范围均匀性增厚居多。结合临床、实验室检查以及适时的病灶动态演变观察,多能够确诊SLSP,鉴别困难时需穿刺活检或开胸探查。
【关键词】肺炎;单发局灶;体层摄影术;诊断,鉴别
王宗会,彭如臣.单发局灶球形肺炎的CT表现特征及鉴别诊断价值[J].中国全科医学,2016,19(18):2227-2231.[www.chinagp.net]
Wang ZH,Peng RC.CT manifestations of solitary localized spherical pneumonia and its diagnostic value[J].Chinese General Practice,2016,19(18):2227-2231.
单发局灶球形肺炎(solitary localized spherical pneumonia,SLSP)是肺部炎症的一种特殊类型,CT表现为孤立性肺结节或肿块,临床上缺乏特征性表现,与局灶机化性肺炎、炎性假瘤(炎性肌纤维母细胞瘤)、结核球、错构瘤、早期周围型肺癌等CT表现有重叠[1]。选取经临床、手术病理证实的SLSP患者,并复习相关文献,回顾性分析SLSP的CT表现特征及鉴别诊断价值,以进一步加强对本病的系统认识及与肺内其他病变(尤其是肿瘤)的鉴别诊断能力。
1资料与方法
1.1纳入与排除标准纳入标准:(1)首诊发现病灶,未经过治疗;(2)经临床、手术病理证实为SLSP;(3)CT表现为孤立性肺结节或肿块。排除标准:(1)其他医院抗感染治疗后发现的患者;(2)CT表现肺叶分布或弥漫性分布的病变。
1.2一般资料搜集2006年8月—2015年1月于开滦(集团)有限责任公司唐家庄医院临床、手术病理证实且符合纳入与排除标准的54例SLSP患者的临床资料。其中男37例,女17例;年龄13~62岁,中位年龄43岁;病程15 d~2个月;主要症状:咳嗽、咳痰46例(其中伴血丝18例),发热40例,胸疼15例;因主要症状就医发现47例,体检发现7例;实验室检查:白细胞计数(WBC)增加(>10.0×109/L)38例,红细胞沉降率(ESR)增快(>20 mm/1 h)
本研究创新点:
本研究回顾性分析了单发局灶球形肺炎(SLSP)的CT表现特征及鉴别诊断价值,发现SLSP主要位于双肺下叶后外基底段或背段,以贴近胸膜面常见,表现为楔形或类圆形,边缘多为毛糙的长毛刺或模糊的晕征;可见肺门侧血管、支气管局部充血征,病灶侧缘的小片状炎性渗出表现。贴近胸膜者,胸膜以较广范围均匀性增厚居多。以此为临床鉴别确诊SLSP提供依据。
16例。患者均签署知情同意书,本研究经开滦(集团)有限责任公司唐家庄医院医学伦理委员会审批通过。
1.3检查方法患者均采用美国GE Light Speed 16螺旋CT扫描仪进行CT扫描,层厚10 mm,层距10 mm,发现病灶后行3 mm薄层扫描。所有原始数据传递到影像归档和通信系统(PACS)工作站行多平面重组(MPR)。患者均由2名中级以上医学影像学医师共同阅片,主要观察CT表现特征(包括病灶部位、形态、边缘、大小、密度,邻近胸膜改变,肺门侧表现,病灶侧缘肺野表现)及抗感染治疗后动态变化。
2结果
2.1CT表现特征(1)病灶部位:38例(70.4%)患者病灶部位为双肺下叶后外基底段及背段,12例(22.2%)为上叶,4例(7.4%)为右肺中叶。(2)病灶形态:46例(85.2%)患者病灶中心层面略呈楔形,尖端指向肺门侧,其中34例(73.9%)可见病灶中心1~3个层面以胸膜为基底,两侧缘或一侧缘垂直胸膜的类方形征(见图1),9例(19.6%)呈山丘状,3例(6.5%)呈三角形;8例(14.8%)呈类圆形。(3)病灶边缘:41例(75.9%)可见毛糙的长毛刺(见图2),13例(24.1%)肺窗周围为模糊的带状低密度影,呈晕征(见图3)。(4) 病灶大小:病灶直径2.0~7.5 cm,平均病灶直径3.9 cm;(5)病灶密度:30例(55.6%)平扫CT值15~70 Hu,病灶密度均匀;18例(33.3%)中心密度偏高;6例(11.1%)中心密度偏低。(6)邻近胸膜改变:48例(88.9%)病灶与胸膜相贴,其中41例(85.4%)周围胸膜均匀性增厚,胸膜下病灶与胸膜接触面较宽,增厚胸膜长径大于胸膜下病灶与之平行的最大长径(见图4)〔其中30例伴增厚胸膜与胸壁间的脂肪间隙(脂肪密度)〕;6例(11.1%)病灶不与胸膜相贴,其中4例可见胸膜线影。(7)肺门侧表现:30例(55.6%)显示局部充血征,即肺门侧有数条增粗的血管影,大多伴扭曲表现,无僵硬感(见图5);17例(31.5%)病变相对应支气管壁略增厚,未见管腔明显狭窄征象;7例(12.9%)未见肺门侧异常表现。(8)病灶侧缘肺野表现:20例(37.0%)病灶侧缘邻近肺野内可见小斑片状渗出灶(见图4);34例(63.0%)未见斑片状渗出灶。(9)其他:所有患者未见胸膜结节表现,纵隔及肺门未见淋巴结增大征象。
2.2抗感染治疗后动态变化49例(90.7%)患者接受抗炎治疗,其中47例(95.9%)经抗炎治疗后症状减轻、消失(36例2~3周病变吸收、消失,6例4~7周病变消散、吸收,5例8周后病变消散、大部分吸收,仅残存少许索条影),2例(4.1%)抗结核治疗效果不良,再行抗感染治疗病灶消散、吸收;5例(9.3%)手术切除。

图1左肺上叶尖后段病灶以胸膜为基底,两侧缘垂直胸膜的类方形征,其中可见空气支气管征
Figure 1Nidus in the anterior section of the upper lobe tip of the left lung had pleura as base,with square-like sign vertical to the two lateral margins,and air bronchogram can be seen in it

图2 肺窗图像上可见边缘较毛糙的长毛刺
Figure 2Coarse and long burrs on margins can be seen in the pulmonary window image
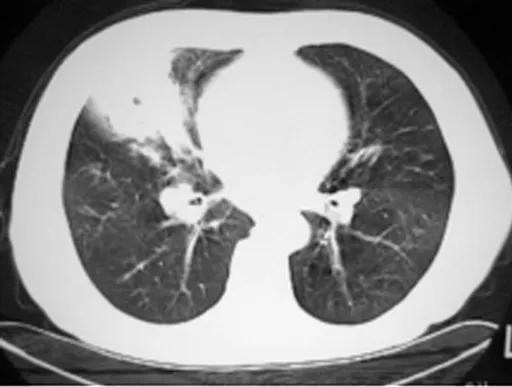
图3 肺窗周围为边缘模糊的带状低密度影,呈晕征
Figure 3Ribbon-like low-density image with vague margins around pulmonary window can be seen,taking on halo sign
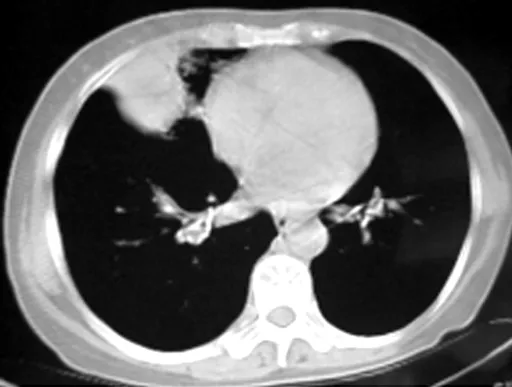
图4与图3为同一患者,胸膜均匀增厚,增厚胸膜长径大于胸膜下病灶与之平行的最大长径,病灶侧缘可见小斑片状渗出灶
Figure 4The image is of the same patient in Figure 3 who had average increase in the thickness of pleura.The longer diameter of the thickened pleura is longer than the maximum diameter beneath pleura parallel to it,and small patchy oozing nidus can be seen at the lateral margins of nidus
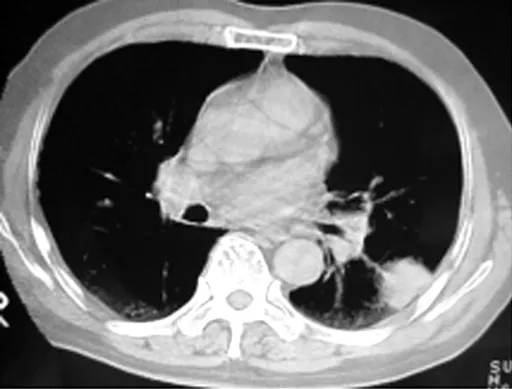
图5 肺门侧有一条增粗的血管影,扭曲表现,无僵硬感
Figure 5There was a thickened vessel shadow at hilus of the lung with distortion but no stiffness
3讨论
3.1SLSP概念、病理机制及临床表现SLSP是指在影像学上多表现为圆形、椭圆形、楔形或类方形的以炎性渗出性病变为主的团块。其病理过程肺结构无损坏、坏死,与机化性肺炎、炎性假瘤(炎性肌纤维母细胞瘤)、结核球、错构瘤及早期周围型肺癌不同[1]。SLSP的病理机制有4种推断[1-2]:(1)肺炎性渗出物经孔氏孔和博兰管向外周离心性等距扩散,显示球形轮廓;(2)不典型大叶性肺炎或节段性肺炎从外周开始吸收消散,CT表现为球形、楔形或类方形;(3)肺脓肿在空洞形成前或坏死物排空不畅时,可表现为球形;(4)支气管内黏液栓引起相应支气管梗阻性炎症和肺不张。本研究患者均为急性期,吸收过程中病灶形态可由球形向椭圆形或不规则形转变;未见支气管黏液栓和不张,故笔者认同第一、二种病理机制推断。炎性渗出物扩散受邻近脏层胸膜(包括叶间胸膜)或小叶间隔阻挡形成类方形征,即为一佐证。徐岩等[3]报道,球形肺炎常发生在年龄较小的儿童中,若发生在成人,常被误诊为肺癌。本研究中仅1例儿童,与上述报道不符,可能与本院未设儿科病房有关。以往文献对SLSP讨论、研究较少,SLSP的发病年龄较大,炎性症状不典型,临床表现缺乏特异性,尤其应与早期周围型肺癌鉴别,首诊误诊率高[1-2,4-5],本研究旨在综合分析SLSP表现特征,进一步提高对其的鉴别诊断水平及影像诊断准确率。
3.2SLSP的CT表现特征及治疗SLSP在CT图像上以双肺下叶后外基底段及背段、贴近胸膜面较为多见,表现为局灶楔形或类圆形病灶[1-2,4],边缘多毛糙的长毛刺或边缘模糊的晕征[6-7],病灶多密度均匀[3]。本研究70.4%患者病灶部位为双肺下叶后外基底段及背段,与宋春燕等[1]报道的66%(37/56)基本一致。本研究88.9%患者病灶与胸膜相贴,其中41例周围胸膜均匀性增厚,比樊庆胜等[2]报道的与胸膜相贴占75%(21/28)的比例略高,可能与病程较长有关。85.2%患者病灶中心层面略呈楔形,其中34例可见病灶中心1~3个层面以胸膜为基底,两侧缘或一侧缘垂直胸膜的类方形征;14.8%患者病灶呈类圆形,考虑与本研究患者病程较长,免疫力正常,炎症从边缘开始吸收消散有关。本研究75.9%患者可见毛糙的长毛刺,24.1%患者肺窗周围为模糊的带状低密度影,呈晕征,反映了病变急性炎性渗出改变的本质。55.6%患者病灶密度均匀,与其他研究结果一致[3]。30例(55.6%)患者显示局部充血征,即肺门侧有数条增粗的血管影,大多伴扭曲表现,无僵硬感,系肺门侧血管充血、炎性渗出所致,有别于周围型肺癌的血管集束征,与肿瘤内间质纤维化牵拉肺门侧血管有关[1-2]。31.5%患者病变相对应支气管壁略增厚,为炎性病变形成的周围充血、水肿。SLSP病灶周围常伴有零星斑片状渗出灶,主要位于病灶侧缘[1,4,8]。
本研究47例接受抗炎治疗的患者中,36例2~3周病变吸收、消失,6例4~7周病变消散、吸收,5例8周后病变消散、大部分吸收,仅残存少许索条影,提示病变吸收、好转时间长短不一。病灶起病后4周内炎症吸收为正常吸收,4~8周为延迟吸收,8周后吸收为不完全吸收,且后两者与高龄、糖尿病、慢性支气管炎、治疗延迟、治疗不完善以及大量使用抗生素有关[2]。延迟吸收、不完全吸收时鉴别诊断相对困难,笔者建议边抗炎,边复查,每2周复查1次,多能明确诊断。
3.3SLSP的鉴别诊断(1)局灶机化性肺炎:好发于肺野外带、胸膜下,密度多不均匀,可见反晕征,边缘常不规则,可见长毛刺征、棘状突出征或弓形凹陷征[9],增强扫描病灶内有坏死腔,且坏死腔似有一定张力感,病灶内可见肺血管穿行,病灶多延迟强化[10]。(2)肺炎性假瘤:是一组肺内瘤样增生的病变,并非真正的肿瘤,多有肺部感染病史,CT表现为球型或团块型,生长缓慢,密度不均匀,形态不规则,边缘多不光整,典型者可见尖角征或切边征,增强扫描后不均匀强化;团块型炎性假瘤内可出现多发、大小不等、类圆形、边界清楚的低密度影而呈脓肿或囊性液化坏死,增强扫描后实性区域明显强化[11]。(3)结核球:多有结核病史,发生于上叶叶尖、后段和下叶背段,边缘大多光整,密度不均匀,可有斑点状钙化,周围可有卫星灶、纤维条索影和胸膜增厚,增强扫描大多无强化,少数呈环状强化[12-13]。(4)错构瘤:边缘光滑整齐,形态规则的圆形或椭圆形结节或肿块。病灶内测到脂肪密度是其特征性征象,典型错构瘤患者其瘤体钙化呈爆米花样[14]。(5)周围型肺癌:肿瘤边缘多不光整,多伴细小毛刺和/或深分叶和/或胸膜凹陷征,可见周围环绕的边缘清楚的磨玻璃晕征、血管集中征,肿瘤密度不均匀,纵隔和肺门可见肿大淋巴结[12,15-16]。
本研究分析了SLSP的CT平扫特征性表现,不足之处是无增强扫描患者,缺少对MPR图像的讨论,有待于将来进一步研究。
总之,SLSP主要位于双肺下叶后外基底段或背段,以贴近胸膜面常见,表现为楔形或类圆形,边缘多为毛糙的长毛刺或模糊的晕征;可见肺门侧血管、支气管局部充血征,病灶侧缘的小片状炎性渗出表现。贴近胸膜者,胸膜以较广范围均匀性增厚居多。结合临床、实验室检查以及适时的病灶动态演变观察,多能够确诊SLSP,鉴别困难时需穿刺活检或开胸探查。
作者贡献:王宗会进行试验设计与实施,资料收集整理、撰写论文,成文并对文章负责;彭如臣进行质量控制及审校。
本文无利益冲突。
参考文献
[1]Song CY,Wang W.Imaging diagnosis of spherical pneumonia(report of 56 cases)[J].Journal of Medical Imaging,2009,19(5):539-540.(in Chinese)
宋春燕,王雯.球形肺炎影像学诊断(附56例分析)[J].医学影像学杂志,2009,19(5):539-540.
[2]Fan QS,Li JL,Cui GQ,et al.CT differentiation diagnosis of spherical pneumonia[J].Journal of Clinical Radiology,2007,26(2):144-147.(in Chinese)
樊庆胜,李继亮,崔国强,等.球形肺炎的CT诊断与鉴别诊断[J].临床放射学杂志,2007,26(2):144-147.
[3]徐岩,马大庆.免疫正常人群肺炎的影像表现[J].中华放射学杂志,2013,47(11):1054-1056.
[4]姚田岭,王汝良,曲世巍,等.64排螺旋CT对球形肺炎的诊断价值[J].牡丹江医学院学报,2011,32(4):62-63.
[5]Li TY.Acute solitary localized pneumonia:CT diagnosis[J].Chinese Journal of Radiology,1999,33(6):368-370.(in Chinese)
李铁一.急性单发局灶肺炎的CT诊断[J].中华放射学杂志,1999,33(6):368-370.
[6]唐光健,秦乃姗.现代全身CT诊断学[M].3版.北京:中国医药科技出版社,2013:588-591.
[7]Zhang J,Zhang YX,Chi BR,et al.An analysis on the clinical differentiating diagnosis and treatment of spherical pneumonia and the early severe acute respiratory syndrome[J].Chinese General Practice,2005,8(19):1588-1589,1591.(in Chinese)
张捷,张云霞,迟宝荣,等.球形肺炎与早期SARS的临床鉴别及诊治分析[J].中国全科医学,2005,8(19):1588-1589,1591.
[8]Li ZJ.Spherical pneumonia:CT diagnosis[J].Journal of Practical Radiology,2000,16(4):215-217.(in Chinese)
李之江.CT诊断球形肺炎[J].实用放射学杂志,2000,16(4):215-217.
[9]Zhu GM,Li ZY,Li YB,et al.Multi-slice spiral CT diagnosis of focal organized pneumonia and its differentiation with peripheral pulmonary carcimona[J].Journal of Clinical Radiology,2014,33(11):1675-1679.(in Chinese)
朱刚明,李兆勇,李扬彬,等.局灶性机化性肺炎的多层螺旋CT诊断及与周围型肺癌鉴别[J].临床放射学杂志,2014,33(11):1675-1679.
[10]Nie X,Li HJ,Nie S,et al.CT features of focal organizing pneumonia[J].Journal of Practical Radiology,2015,31(10):1620-1623.(in Chinese)
聂晓,李海军,聂思,等.局灶性机化性肺炎 CT 表现[J].实用放射学杂志,2015,31(10):1620-1623.
[11]Deng KX,Wei C,Cao DX,et al.Inflammatory pseudotumor of the lung:CT diagnosis[J].Chinese Computed Medical Imaging,2010,16(3):211-214.(in Chinese)
邓克学,韦超,曹东兴,等.肺炎性假瘤CT诊断[J].中国医学计算机成像杂志,2010,16(3):211-214.
[12]Zhou YS,Zhang CH,Huang XM,et al.CT diagnosis of tuberculomas and peripheral carcinomas of lung with diameters less than 3cm[J].Journal of China Clinic Medical Imaging,2003,14(2):91-93.(in Chinese)
周永生,张承惠,黄向名,等.直径小于3cm肺结核球和周围型肺癌的CT诊断[J].中国临床医学影像杂志,2003,14(2):91-93.
[13]Meng YN,Chen YP,Li XL,et al.The clinical application of T-SPOT.TB test combining with fiberoptic bronchoscopy examination in diagnosis of child-hood pulmonary tuberculosis[J]. Chinese Journal of Difficult and Complicated Cases,2014,13(9):907-909,912.(in Chinese)
孟燕妮,陈艳萍,李秀龙,等.结核感染T细胞斑点试验联合纤维支气管镜检在结核病患儿诊断中的应用[J].疑难病杂志,2014,13(9):907-909,912.
[14]Chen RF,Wu XM,Deng Y,et al.Diagnosis of pulmonary harmartomas with multislice spiral CT[J].Journal of Practical Medical Imaging,2011,12(4):208-210,220.(in Chinese)
陈容凤,伍筱梅,邓宇,等.肺错构瘤的多层螺旋CT诊断[J].实用医学影像杂志,2011,12(4):208-210,220.
[15]Lyu Y,Xie RM,Zhou XH,et al.CT and pathology observation of peripheral lung cancer with halo sign[J].Chinese Journal of Medical Imaging Technology,2010,26(6):1096-1099.(in Chinese)
吕岩,谢汝明,周新华,等.磨玻璃晕征环绕的周围型肺癌的CT特征及病理对照观察[J].中国医学影像技术,2010,26(6):1096-1099.
[16]Zhang H,Pei ZJ.Comparison of the therapeutic effect of video thoracoscopic lobectomy and open chest operation in the treatment of peripheral lung cancer:A Meta-analysis[J]. Chinese Journal of Difficult and Complicated Cases,2015,14(12):1288-1295.(in Chinese)
张皓,裴志杰.全电视胸腔镜下肺叶切除术与开胸手术治疗周围型肺癌疗效比较的Meta分析[J].疑难病杂志,2015,14(12):1288-1295.
(本文编辑:崔丽红)
CT Manifestations of Solitary Localized Spherical Pneumonia and Its Diagnostic Value
WANGZong-hui,PENGRu-chen.
DepartmentofRadiology,KailuanTangjiazhuangHospital,Tangshan063100,China
【Abstract】ObjectiveTo investigate the CT manifestations of solitary localized spherical pneumonia(SLSP) and its differential diagnostic value in order to improve the imaging diagnostic ability of the disease.MethodsFrom August 2006 to January 2015,we collected the clinical data of 54 patients who were diagnosed as SLSP by surgery and pathology and accorded with inclusion and exclusion criteria from Kailuan Tangjiazhuang Hospital.CT manifestations of patients were observed and analyzed,including site,shape,margin,size,density,adjacent pleura changes,manifestations close to the hilus of lung,manifestations of the field adjacent to nidus.The dynamic changes after anti-inflammation therapy were also observed and analyzed.ResultsThere were 38(70.4%) patients who had nidus in the posterior basal segments and dorsal segments of the lower lobes;46(85.2%) patients had wedge-shape nidus,including 34(73.9%) patients with square-like nidus,9(19.6%) patients with hill-shape nidus and 3(6.5%) patients with triangle-shape nidus.There were 41(75.9%) patients who had coarse and long burrs and 13(24.1%) patients who had vague ribbon-like low-density shadow which took on halo sign.The diameter of nidus was 2.0-7.5 cm,and the average diameter was 3.9 cm.The density of nidus of 30(55.6%) patients was average.There were 48(88.9%) patients who had nidus close to pleura,and 41 patients had even increase in the thickness of surrounding pleura.Localized hyperemia sign appeared in 30(55.6%) patients,and 17(31.5%) patients had slight increase in the bronchial wall corresponding to lesion;20(37.0%) patients had small patchy oozing focus.There were 49(90.7%) patients who received anti-inflammation therapy;among them,47(95.9%) patients saw symptoms relieve and disappear after anti-inflammation therapy,2(4.1%) patients had unfavorable treatment outcomes after antituberculosis therapy and then received anti-inflammation therapy which dissipated and absorbed nidi,and 5(9.3%) patients received excision.ConclusionSLSP mainly locates in the lateral posterior basal segments and dorsal segments of the lower lobes,mostly being close to pleural surface and taking on the wedge or quasi-circular shape;the margins are mostly coarse long burrs or vague halo signs.Localized hyperemia signs appear in vessels and bronchia at the hilus of the lung,and small patchy inflammatory exudation appear.Patients with SLSP close to pleural surface are mostly with average increase in the thickness of pleura in a wider range.Combined with clinical and laboratory manifestations and observation of the dynamic changes of nidus,SLSP can be definitely diagnosed,and aspiration biopsy or thoracotomy can be conducted when there is difficulty in diagnosis.
【Key words】Pneumonia;Solitary localized nidus;Tomography;Diagnosis,differential
通信作者:彭如臣,101149 北京市,首都医科大学附属北京潞河医院医学影像中心;E-mail:13501271260@163.com
【中图分类号】R 563.1
【文献标识码】A
doi:10.3969/j.issn.1007-9572.2016.18.024
(收稿日期:2015-11-17;修回日期:2016-03-22)
·全科医生技能发展·
