股骨远端肿瘤患者假体置换后远期翻修三例报告
2014-02-14阎洪亮董扬张智长马焕之张春林杨庆诚
阎洪亮 董扬 张智长 马焕之 张春林 杨庆诚
股骨远端肿瘤患者假体置换后远期翻修三例报告
阎洪亮 董扬 张智长 马焕之 张春林 杨庆诚
目的报告 3 例股骨远端肿瘤患者假体置换 25 年后的翻修病例,总结股骨远端肿瘤型假体因远期松动而再次行假体翻修手术的结果与体会。方法回顾性分析 2008 年 1 月至 2012 年 12 月,3 例因股骨远端肿瘤型假体置换术 25 年后松动,在本院行假体翻修术患者的临床资料,包括临床症状( 膝关节周围疼痛、行走困难等 )、影像学表现( X 线示假体松动移位及翻修后假体位置 )、手术方法及技巧、术后功能恢复等,3 例翻修术后随访至少 5 年。结果3 例翻修术后临床症状改善,膝关节周围疼痛缓解,术后 X 线示关节位置可,随访过程中均未出现假体松动、移位、断裂等并发症,根据 1993 年美国骨肿瘤学会评分系统( MSTS93 ),3 例术后功能评分分别为 70%、80% 及 73.3%,术后患者功能恢复良好,同时也未出现肿瘤局部复发及转移。结论肿瘤型假体长期使用,可出现松动、感染及排异等并发症。肿瘤假体远期松动行翻修时,取出松动的假体及骨水泥较容易;初次假体置换术后,假体周围会形成大量瘢痕组织甚至生物假膜,生物假膜切除应尽量彻底;翻修时患者多有软组织缺损,应准备肌瓣转移术。
股骨肿瘤;关节成形术,置换,髋;人工关节;再手术;骨肿瘤;髋关节
随着骨肿瘤保肢手术的开展,肿瘤假体置换是保肢手术中重要的方法之一。然而在肿瘤假体置换的同时,也会出现一系列的并发症,如肿瘤假体的松动[1]、感染及排异等[2-3]。置换后假体的 5 年使用率为 57%~93%[4]。因此,由于假体远期松动所导致的翻修手术也日益增多。我院为股骨远端肿瘤假体置换后 25 年以上的 3 例,进行了翻修手术,现报告如下。
资料与方法
一、一般资料
本组 3 例中,女 2 例,男 1 例,平均年龄63 岁,左侧 1 例,右侧 2 例。3 例均因数年前患侵袭性股骨远端骨巨细胞瘤,在外院行股骨远端瘤段切除及全膝关节置换术[5-6],病理诊断均为骨巨细胞瘤。术后患者功能恢复尚可,没有出现肿瘤局部复发、转移等情况。但分别于数年后出现膝关节周围疼痛,行走后加重或无法行走等症状。
二、翻修原因
在行股骨瘤段切除肿瘤假体置换术数年后,3 例均出现了不同程度的膝关节周围疼痛,2 例行走后加重,1 例无法行走,3 例均有不同程度的假体松动移位,1 例松动移位穿破骨皮质。
三、翻修时间
3 例从前次手术到此次翻修术时间间隔分别为30、29、26 年,平均 28.3 年( 表1 )。
四、手术方法
由于 3 例均未出现假体周围感染,因此均一期行假体翻修。患者假体时间久远,术前应准备全套翻修假体。
患者全麻后,取仰卧位,手术区域常规消毒,铺巾并上消毒止血带。在原手术入路进入,逐层切开皮肤、皮下及筋膜。值得一提的是二次手术后膝关节周围的组织通常较厚,因此切口应比原来稍加延长,以便充分暴露。将膝关节脱位,由于 3 例假体均不同程度松动,因此可直接将松动假体部件取出,但其中 1 例较为牢固,须用专用打拔器将其取出。如果假体部件牢固,上述方法难以取出时,可先在骨干钻孔、开槽,去除部分骨水泥后,再去除假体。待假体部件全部去除后,再用球形髓腔钻磨去除大部分腔内残留的骨水泥,后改用薄鼓捣凿除剩余少量骨水泥,注意不要造成骨折及皮质穿透。相对于假体和骨水泥的去除,生物假膜的去除就困难很多,3 例术中均见不同程度的生物假膜及周围组织瘢痕形成,可以用电刀、脑膜剪、咬骨钳等去除生物假膜及瘢痕组织,彻底清创,直至正常组织。最后安装翻修假体。2 例可直接安放假体,1 例因残端皮质极薄,因此将残端适当截除,然后放置新的骨水泥假体。由于 1 例软组织缺损较为严重,因此对其行腓肠肌内侧头肌皮瓣转移修复术[7]。确切止血,大量生理盐水冲洗,C 型臂机下透视肿瘤假体在位,位置满意,放置引流,逐层缝合切口。
五、术后处理及功能锻炼
术后对 3 例行常规抗炎补液支持治疗,患肢抬高,膝关节屈曲 30°,引流管放置 3~5 天( 当引流量<50 ml 时拔出 )。术后患者疼痛缓解后( 一般在术后 2 天 )可行股四头肌收缩锻炼,在伤口良好情况下,5~7 天可用 CPM 机进行屈曲锻炼。术后 2 周患者可部分负重与关节活动练习,术后 3~4 周逐渐负重行走。
3 例肿瘤假体翻修均为骨水泥固定,术后随访时间 68~82 个月,均在 5 年以上。
结 果
二次翻修术后,3 例均无肿瘤复发,亦未出现假体松动、假体感染、假体移位、假体断裂等并发症。患者术后功能恢复良好( 表2~4 )( 图1 )。

表1 本组 3 例一般资料Tab.1 The general data of the 3 patients
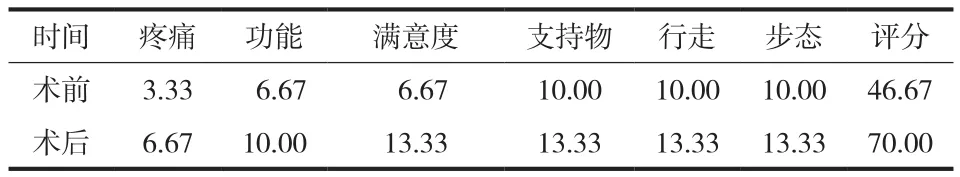
表2 例 1 术前及术后 MSTS( 93 )评分( % )Tab.2 The preoperative and postoperative MSTS 93 scores of the 1st patient
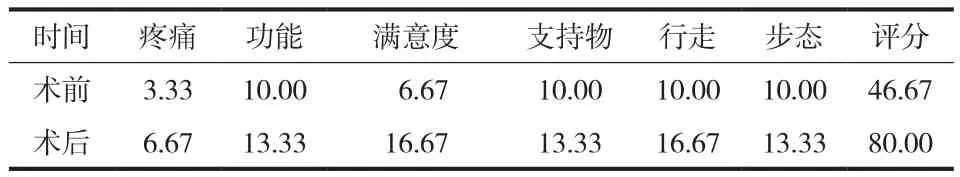
表3 例 2 术前及术后 MSTS( 93 )评分( % )Tab.3 The preoperative and postoperative MSTS 93 scores of the 2nd patient

图1 患者,女,54 岁。左膝关节肿瘤假体翻修术后 a:翻修前 X 线片,见假体松动移位并穿破近端骨皮质;b:术中见大量生物假膜形成,将假体取出;c:取出的假体及尽可能清除掉的生物假膜;d:再次置入的肿瘤型膝关节假体;e:清楚假膜及瘢痕后缺损大,行腓肠肌瓣转移;f:术后 X 线片,见翻修后假体位置可;g:患者超过 5 年的随访,膝关节伸直、屈曲等功能可Fig.1 Prosthetic revision was performed on a 54-year-old female patient with tumors in the left knee joint a: The preoperative X-ray showed prosthetic loosening and migration, and the prosthesis had broken through the proximal cortex; b: A lot of biological pseudomembranes were formed during the operation, and the prosthesis was pulled out; c: The removed prosthesis and the resected biological pseudomembranes; d: The tumor prosthesis of the knee joint was implanted again; e: Muscle fap transplantation was performed due to serious defects after the pseudomembranes and scars were removed; f: The postoperative X-ray showed the prosthetic position was good; g: The extension and fexion of the knee joint were satisfactory during the over-5-year follow up
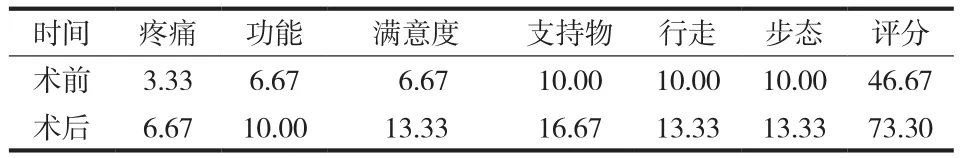
表4 例 3 术前及术后 MSTS( 93 )评分( % )Tab.4 The preoperative and postoperative MSTS 93 scores of the 3rd patient
讨 论
保肢治疗是膝关节周围恶性肿瘤手术的主要方式,保肢治疗的方法有很多,如自体骨移植、灭活再植、异体骨移植、肿瘤型人工关节置换及复合重建等[8],其中人工关节假体置换应用最为广泛。即使人工关节置换有较好的早期效果,并可以长期使用,但却存在诸多并发症。其中股骨远端肿瘤假体翻修可能性 5 年为 17%,10 年为 33%,20 年为58%。同首次人工关节置换一样,肿瘤假体翻修术后存在一系列并发症[9],如神经血管损伤、假体感染、机械性松动、断裂等,但是仍能保留患者的肢体并恢复其部分功能。由于大部分肿瘤假体翻修患者的骨皮质较薄、骨缺损范围的不确定性以及软组织缺乏弹性并且缺损广泛[10],因此术前应有详细的手术计划,并告知患者有肢体不等长及关节功能受限的可能。同第一次的肿瘤假体置换相比,肿瘤假体翻修术有其独特的特点:( 1 )由于远期松动所导致的假体翻修,假体的取出相对容易,有的部件可以直接取出,有的则需要先在骨干钻孔、开槽,去除部分骨水泥再去除假体。( 2 )水泥型膝关节肿瘤假体置换的患者,股骨和胫骨的髓腔内都有大量骨水泥填充,为了安装新的肿瘤假体,必须将其尽可能地取出。一般骨水泥的取出也相对容易,可先用球形髓腔钻磨去除大部分腔内残留的骨水泥,后改用薄鼓捣凿除剩余少量骨水泥,此时要当心不要造成骨折及皮质穿透。( 3 )初次假体置换术后,假体周围会形成大量瘢痕组织甚至生物假膜[11-12],为改善术后功能和控制术后感染,需要尽可能地清楚这些生物假膜及瘢痕组织。生物假膜的清除较假体和骨水泥的取出更为复杂和繁琐,可以用电刀、脑膜剪、咬骨钳等去除。由于翻修时患者解剖结构不清楚,也很容易造成血管神经的损伤,因此术中应格外小心。( 4 )翻修手术难度较大,由于患者软组织缺损较为严重,因此可以进行腓肠肌内侧头等肌皮瓣的转移,以更好地覆盖。另外,较首次假体置换,翻修术所用手术时间及术中出血量也较多。
同普通关节置换假体一样,恶性肿瘤患者或部分侵袭性骨巨细胞瘤患者的肿瘤假体可以长期使用,甚至可达数十年。肿瘤假体远期松动在行翻修术时应注意:术前要有完善的计划,且告知患者有肢体不等长及关节功能受限的可能。手术过程中取出松动的假体以及骨水泥较容易;初次假体置换术后,假体周围会形成大量瘢痕组织甚至生物假膜,生物假膜尽量切除彻底,以改善患者功能及减少术后感染可能,但相对较为繁琐;翻修时患者多有软组织缺损,应准备肌瓣转移术。
[1] Unwin PS, Cannon SR, Grimer RJ, et al. Aseptic loosening in cemented custom-made prosthetic replacements for bone tumours of the lower limb. J Bone Joint Surg Br, 1996, 78(1): 5-13.
[2] Orlic D, Smerdelj M, Kolundzic R, et al. Lower limb salvage surgery: Modular endoprosthesis in bone tumour treatment. Int Orthop, 2006, 30(6):458-464.
[3] Morii T, Morioka H, Ueda T, et al. Deep infection in tumor endoprosthesis around the knee: a multi-institutional study by the Japanese musculoskeletal oncology group. BMC Musculoskelet Disord, 2013, 14:51.
[4] Biau D, Faure F, Katsahian S, et al. Survival of total knee replacement with a megaprosthesis after bone tumor resection. J Bone Joint Surg Am, 2006, 88(6):1285-1293.
[5] Karpik M, Reszeć J, Skowroński J. Custom made tumorprosthesis as a primary treatment for giant cell tumor of femur--case report. Ortop Traumatol Rehabil, 2011, 13(1):73-81.
[6] Khan SA, Kumar A, Inna P, et al. Endoprosthetic replacement for giant cell tumour of the proximal femur. J Orthop Surg (Hong Kong), 2009, 17(3):280-283.
[7] Trieb K, Göggel M, Dürr HR. et al. [Proximal tibial reconstruction with gastrocnemius flap]. Oper Orthop Traumatol, 2012, 24(3):263-269.
[9] Foo LS, Hardes J, Henrichs M, et al. Surgical difficulties encountered with use of modular endoprosthesis for limb preserving salvage of failedallograft reconstruction after malignant tumor resection. J Arthroplasty, 2011, 26(5):744-750.
[10] 汤小东, 郭卫, 杨荣利, 等. 膝关节定制型肿瘤假体的翻修. 中国修复重建外科杂志, 2010, 24(1):5-10.
[11] Mavrogenis AF, Papagelopoulos PJ, Coll-Mesa L, et al. Infected tumor prostheses. Orthopedics, 2011, 34(12):991-998.
[12] Dunne N, Hill J, McAfee P, et al. In vitro study of the effcacy of acrylic bone cement loaded with supplementary amounts of gentamicin: effect onmechanical properties, antibiotic release, and biofilm formation. Acta Orthop, 2007, 78(6): 774-785.
( 本文编辑:李贵存 )
Long-term revision after prosthetic replacement for the patients with tumors in the distal femur: three cases report
YAN Hong-liang, DONG Yang, ZHANG Zhi-chang, MA Huan-zhi, ZHANG Chun-lin, YANG Qing-cheng. Department of Orthopaedics, the sixth People’s Hospital Affliated to Shanghai Jiaotong University, 200233, PRC
ObjectiveTo report revision surgery in 3 patients with tumors in the distal femur who underwent prosthetic replacement 25 years ago and to summarize the experience of revision surgery because of long-time loosening of the tumor prosthesis in the distal femur.MethodsA total of 3 patients underwent prosthetic revision from January 2008 to December 2012, due to loosening in the distal femur after prosthetic replacement 25 years ago. Their clinical data were retrospectively analyzed, including the clinical symptoms( pain around the knee and walking difficulties ), imaging manifestations( prosthetic loosening and migration and prosthetic position after revision surgery based on the X-ray ), operation methods and techniques, postoperative functional recovery and so on. All the 3 patients were followed up for at least 5 years.ResultsThe clinical symptoms of the 3 patients were improved after revision surgery, with pain relief around the knee. The postoperative X-ray showed the joint position was good. No complications such as prosthetic loosening, migration or breakage were noticed during the follow-up. According to the Musculoskeletal Tumor Society( MSTS 1993 )staging system, their postoperative functional scores were 70%, 80% and 73.3%. The postoperative functional recovery of all the patients was satisfactory and no local tumor recurrence or metastasis was noticed.ConclusionsThe tumor prosthesis is durable. However, the complications such as loosening, infection or rejection may occur. It is relatively easy to pull out the prosthesis and the bone cement in revision surgery due to long-term loosening of the tumor prosthesis. After primary prosthetic replacement, a lot of scar tissues and even biological pseudomembranes will be formed around the prosthesis. Biological pseudomembranes should be resected as completely as possible. Muscle fap transplantation should be prepared for the patients with soft tissue defects during the revision.
Femoral neoplasms; Arthroplasty, replacement, hip; Joint prosthesis; Reoperation; Bone neoplasms; Hip joint
10.3969/j.issn.2095-252X.2014.05.016
R738.1, R687.3
200233 上海交通大学附属第六人民医院骨科
董扬,Email: dongyang6405@163.com
2013-10-13 )