The effect of dexmedetomidine on decrease of cough,hemodynamic parameters and Ramsay score versus lidocaine during general anesthesia:a randomized clinical trial
2021-03-03SoheilaSaidieHesameddinModirBijanYazdiEsmailMoshiriGholamrezaNooriAbolfazlMohammadbeigi
Soheila Saidie,Hesameddin Modir ,Bijan YazdiEsmail MoshiriGholamreza Noori,Abolfazl Mohammadbeigi
1 Students Research Committee,Arak University of Medical Sciences,Arak,Iran
2 Departments of Anesthesiology and Critical Care,Arak University of Medical Sciences,Arak,Iran
3 Department of Surgery,Arak University of Medical Sciences,Arak,Iran
4 Department of Epidemiology and Biostatistics,Neuroscience Research Center,Qom University of Medical Sciences,Qom,Iran
Abstract Physiological responses remain common during anesthesia emergence and endotracheal extubation,causing some complications.We aimed to address the effect of dexmedetomidine (DEX) on decrease of cough,hemodynamic parameters and Ramsay score in comparing to lidocaine (LID) during anesthesia.In this double-blinded randomized clinical trial 120 hospitalized patients undergoing general anesthesia were enrolled after obtaining written consent.Block random allocation was used to assign patients into three groups including DEX (intravenous injection; 0.5 μg/kg),LID (1.5 mg/kg),and PBO (10 mL normal saline) at 10 minutes before anesthesia.No statistical significance was uncovered among three groups in blood pressure,oxygen saturation,frequency of laryngospasm and duration of surgery amongst the groups(P > 0.05),but DEX having lower heart rate and cough frequency (P < 0.05).Moreover,the mean of Ramsay score was statistically higher in DEX and LID groups than PBO except at the 50th and 60th minutes after extubation (P < 0.05).Since the mean of Ramsay score was higher in DEX vs.LID groups and reduced heart rate and cough frequency demonstrates in DEX,it seems that DEX could be an appropriate drug on suppressing cough during anesthesia without side effects.The study protocol was approved by the Ethical Committee of Arak University of Medical Sciences by code IR.ARAKMU.REC.1397.140 on August 19,2018,and the protocol was registered at Iranian Registry of Clinical Trials by code IRCT20141209020258N97 on February 22,2019.
Key words:anesthesia; cough; dexmedetomidine; emergency; lidocaine
INTRODUCTION
Physiological responses remain common during anesthesia emergence and endotracheal extubation,causing complications including cough,laryngospasm,bronchospasm,and tachycardia.1,2The frequently cited complaints following anesthesia include postoperative airway complications such as sore throat,cough,and sputum,among which post-extubation cough has been repeatedly reported to be associated to mechanical irritations such as external pressure,the endotracheal intubation method,endotracheal cuff,endotracheal tube (ETT) size,and so forth,3and is though,usually not believed to be a serious complication from anesthesia.It is undesirable and sometimes occurs as an attack,increasing intracranial,intraocular and intra-abdominal pressures.4,5Intravenous lidocaine (LID) affects and reduces the intensity of post-intubation cough owing to various causes,such as the laryngoscope blade type,straining during endotracheal extubation,and smoking.After the intubation,cuff inflation will pack around the ETT and irritate the trachea.4This causes coughing when the depth of general anesthesia is low and causes many problems.ETT and cuff irritation causes the complication and is the underlying mechanism.High-speed receptors in the tube are abundant and play a key role in coughing.6,7These irritations are blocked during general anesthesia.5,6
Cough during emergence from general anesthesia increases blood pressure,heart rate (HR) and myocardial ischemia,bronchospasm,and bleeding,8multiplies the pain caused by surgery,and increases intracranial and intraocular pressure in patients with brain involvement or glaucoma.9,10Range of methods is available,such as local and intravenous injection of topical anesthetics to reduce cough.5,6,11Furthermore,intravenous use of opioids is an alternative to reducing cough at the end of the operation and during endotracheal extubation,and when the patient does not complete awakening.2,6However,this has frequently not been desirable.The use of topical anesthetics before endotracheal intubation covers a limited time during surgery owing to absorption from the ETT mucus,and subsequently,a further alternative should be employed to achieve a more long-time effect.The intracuffmethod appears to arrive at the goal.12LID reduces goblet cell secretion by controlling the neural pathway,though water absorption is besides reduced by LID effect on ion transport.The use of LID appears to influence the consequences in different ways.7,10,13
Dexmedetomidine (DEX) is an α2-adrenoceptor agonist with antinociceptive,sedative and hypotensive actions and,if infused,it reduces HR,systemic vascular resistance and blood pressure (BP).11,14This,as an adjuvant to induce general anesthesia with a central sympathetic effect,helps to maintain the patient’s hemodynamic status,and has a potent anesthetic effect reducing the need for opioids,complications,and stress response,as well as improving recovery.The DEX’s ability to provide adequate sedation and amnesia seems to remain matchless and causes a mild cognitive impairment that facilitates easy communication between the medical team and the patient in the intensive care unit and those in need of monitoring.2,14
Different studies found a lower HR and mean blood pressure(MBP) in patients receiving DEX,suggesting that the drug be used to reduce the amount of bleeding.11,14As reported by Lee et al.,15DEX alone reduced cough more effectively than remifentanil alone,while no decrease in respiratory rate was observed in patients.Furthermore,other studies suggested that DEX and LID,respectively,reduces cough.6,15,16Given that the effects of both DEX and LID have been so far studied alone,but not compared,we decided to conduct a study to address the compared efficacy of DEX and LID on reducing cough severity.
SUBJECTS AND METHODS
Study setting
The double-blinded study enrolled 102 patients undergoing general anesthesia who were hospitalized at Valiasr Hospital(Arak,Iran),after obtaining written consent and verification of inclusion/exclusion criteria.inclusion criteria were patients who were 20-60 years of age,American Society of Anesthesiologists status I-II,17Mallampati class I-II,18both genders,non-addiction,non-smoking,no active airway infection or history of surgery and pathology of larynx and trachea,absence of lower esophageal sphincter incompetence (absence of reflux),absence of body mass index greater than 30 kg/m2,lack of intracranial and intraocular pressure,surgery time ranged between 60-120 minutes,no pulmonary and heart disease,and no use of drugs causing cough.Exclusion criteria were including lack of patient’s cooperation and satisfaction,and death.

Figure1:CONsolidated Standards of Reporting Trials (CONSORT) diagram showing the flow of participants through each stage of a randomized trial.
The written informed consent was obtained from all subjects and the study protocol was approved by Ethical Committee of Arak University of Medical Sciences by code IR.ARAKMU.REC.1397.140 on August 19,2018.Moreover,the protocol was registered at Iranian Registry of Clinical Trials by code IRCT20141209020258N97 on February 22,2019.The writing and editing of the article was performed in accordance with the CONsolidated Standards of Reporting Trials (CONSORT)Statement (Figure1).
All patients were hospitalized at least one day before surgery,kept nil per os for 8 hours,and afterward randomly split into three groups.All patients underwent the same anesthesia protocol,receiving 5 mL/kg intravenous injection crystalloid Ringer’s solution (Samen Co.,Mashhad,Iran) before induction of anesthesia,followed by 1 µg/kg fentanyl (Aboreyhan Co.,Tehran,Iran) and 2 mg intravenous injection midazolam(Oxir Co.,Tehran,Iran),subsequently,anesthesia was induced with 5 mg/kg thiopental sodium (Kavosh-Gostar Daru,Tehran,Iran) and 0.5 mg/kg intravenous injection atracurium(Caspian Tamin Co.,Rasht,Iran) after pre-oxygenation.This was followed by a direct laryngoscopy via Macintosh blade and endotracheal intubation by cuffed ETT (Flexicare Medical Ltd.,UK) with appropriate size for each patient.We inflated the cuff with a cuff gauge providing a pressure of 2.45 kPa to keep ETT cuff pressure the same for all patients.Thus,all subjects were in the same condition for irritation of the ETT cuff.Anesthesia was continued through 75-150 μg/kg propofol(Aram-Kimia-Caspian Co.,Ghazvin,Iran) infusion per minute and repeated muscle relaxant and opioid.
Intervention
Eligible subjects were assigned into three groups including DEX,LID and normal saline (PBO) by block random allocation method around 10 minutes before surgery:the DEX,LID,and PBO,intravenous injection being slowly infused 0.5 μg/kg DEX(Hospira Co.,IL,USA),1.5 mg/kg LID (Caspian Tamin Co.),and PBO,respectively,in a 10-mL volume (for each) over 10 minutes.At the end of the operation,the ETT was removed after clearing any secretions from the upper airway when following adequate spontaneous respiration and complete awakening of the patient (obeying verbal commands.such as opening the eyes,raising the head for 5 seconds).Subsequently,we assessed and recorded Laryngospasm and cough at 0 and 10 minutes,and during recovery up to 40 minutes after endotracheal extubation,whereas one did their prevalence in all patients.A cough is considered real when the patient spontaneously and quickly exhales,whereas the sound of a cough is heard.Oxygen saturation by pulse oximetry was evaluated and recorded all the time before induction of anesthesia and throughout surgery and during endotracheal extubation at 0,5 minutes,and every 5 minutes up to 40 minutes after extubation,recovery time,and finally when transferring to the ward.
Measurements
We assessed and recorded the changes in mean artery pressure by a non-invasive BP monitor (Williamson Ct.,Louisville,KY,USA) attached to the patient and HR changes by electrocardiogram (Williamson Ct.) throughout the surgery,as well as 5 to 40 minutes after endotracheal extubation.Ramsay score (RS)was assessed at the time of recovery and 10,20,30,40,50,and 60 minutes postoperatively.It should be noted that the data was measured and recorded to conduct a double-blind study by an intern,without any awareness of the patient groupings,when for each group,preparation and administration of adjuvants were done by an anesthesiologist,whereas the patients were not aware of grouping information.
Statistical analysis
Sample size calculation was estimated by considering study power = 80%,and type one error = 0.05 using Medcal software (MedCalc Software,Ostend,Belgium).Data were analyzed using descriptive statistics,one-way analysis of variance,Tukey’spost hoctest,Chi-square and repeated measures analysis of variance by SPSS software version 20.0(IBM Corp,Armonk,NY,USA).
RESULTS
The age of patients in study was 38.08 ± 7.49 years and the minimum and maximum of age were 24 and 51 years,respectively.The mean age (P= 0.900) and sex distribution (P= 0.941) of patients were not statistically significant among three groups(Table1).In addition,there was a statistically significant difference in duration of surgery among the groups (P< 0.05).
According to Figure2A,no statistically significant difference was found in MBP among the three groups at different time after extubation (P> 0.05).However,based on repeated measure test,there was a significant difference in trend of MBP during study among three groups and the MBP was higher in DEX group (P= 0.038).Moreover,as shown in Figure2B,no statistically significant difference was found in mean of oxygen saturation among the groups at different time after extubation (P> 0.05) except at the 5thminute (P=0.23).Repeated measure test did not show significant difference in trend of oxygen saturation during study among three groups (P= 0.468).
Based on the results in Table2,a significant difference was seen in HR among the groups at different times after extubation (P< 0.05).Based on repeated measure test,lower HR observed in the DEX and LID groups than that in the PBO group,and based on Tukeypost hoctest,the HR was lowerin DEX than LID group (P= 0.001).The results revealed that a statistically significant difference was observed in mean of cough frequency (CF) among three groups at all times after extubation (P< 0.05),except at 35-40 minutes (P= 0.072).Based on post hoc test,lower CF was observed in DEX group and was lower than PBO group.Moreover,DEX group had lower CF than the LID up to 20-25 minutes (P< 0.05).A statistically significant difference was seen in RS among the groups except at the 50thand 60thminutes after extubation (P< 0.05).However,in other times,RS was lower in the LID and DEX than in the PBO,but did not observe any difference between two intervention groups.Comparison of laryngospasm among three groups showed that no significant difference was observed among groups at different time after extubation (P> 0.05).
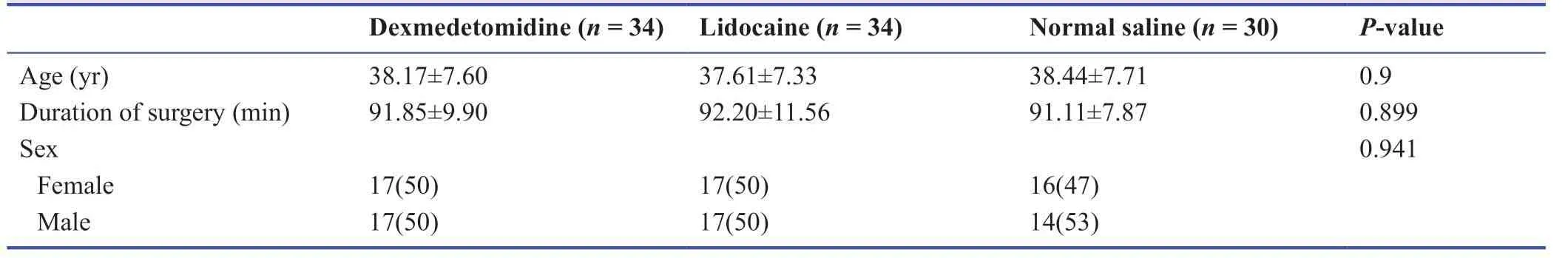
Table1:Comparison of age,surgery duration and sex distribution in dexmedetomidine,lidocaine,and normal saline groups

Figure2:Trend of MBP (A) and SaO2 (B) in the general anesthesia patients of DEX,LlD,and PBO groups.

Table2:Comparison of heart rate,cough frequency and Ramsay score in general anesthesia patients of dexmedetomidine,lidocaine,and normal saline groups
DISCUSSION
A randomized,double-blind randomized clinical trial conducted on 102 patients undergoing general anesthesia in three assigned groups which no statistically significant difference was observed among them regarding to age,gender,BP,SaO2,frequency of laryngospasm,and duration of surgery.Based on our results,HR and CF were lower in the DEX than the others.The DEX group had a lower HR and lower CF for 20-25 minutes,compared to the LID,but a significant statistical difference was seen in RS among the groups at the 50thand 60thminutes and RS was lower in LID and DEX than in the PBO.However,LID and DEX groups were same regarding to RS.Overall,the DEX caused a reduce in HR and CF,compared to the LID and PBO,but RS in the group was not different from that in the LID.
DEX is an adjuvant to induce general anesthesia with a central sympathetic effect has a potent anesthetic effect reducing the need for opioids,complications,and stress response,as well as improving recovery.2,7,11,15DEX is an α2-adrenoceptor agonist with antinociceptive,sedative and hypotensive actions and helps to maintain the patient's hemodynamic status.2,16,19In this study,the DEX was more effective than LID in suppressing cough in patients undergoing anesthesia.
Hancı et al.20study assessed the effects of fentanyl or DEX when used in combination with propofol and LID for tracheal intubation and showed that endotracheal intubation was better with the DEX-LID-propofol combination than with the fentanyl-LID-propofol combination,whereas our results showed that DEX reduces HR and CF,while RS in the DEX was not different from that in the LID.Lee et al.15conducted a study aimed at assessing the efficacy of single dose of DEX to reduce cough during anesthesia in which the DEX group had a lower frequency of cough and mean cough grade during endotracheal extubation,while MBP and HR did not significantly differ.DEX though decreased cough effectively,compared with remifentanil,no decrease was found in respiratory rate in their patients.15Their results were in line with ours.
A systematic review showed that intravenous LID injection from 0.5-2 mg/kg,dose dependently prevents intubation-,extubation-,and opioid-induced cough in adults and children with number needed to treat ranging from 8 to 3.6Nevertheless,our results suggested that LID as well as DEX reduces HR and CF,but RS in the DEX was not different from that in the LID.Guler et al.21performed a study to prescribe a single dose of DEX to reduce agitation and smooth extubation after surgery,reporting that CF was significantly lower in the DEX,while nausea and vomiting were similar,and that DEX reduced cough and agitation in patients,whose results were consistent with ours.
In conclusion,DEX decreased HR and CF compared with the LID and PBO,whereas RS in the DEX did not significantly differ from that in the LID.DEX,like LID,seems to be a promising drug to suppress cough during anesthesia emergence,given the lack of side effects,and to be used as an option and drug choice to achieve the goal.
Acknowledgements
We would like to express their gratitude towards the Clinical Research Council at Valiasr Hospital for its guidance and the research deputy of the Arak University of Medical Sciences for his assistance and support.
Author contributions
Study conception:HM,SS,EM,AM; data collection:GN,AM;data acquisition and analysis:BY,GN; data interpretation:HM,SS;manuscript writing:BY.All authors approved the final version of the manuscript for publication.
Conflicts of interest
There is no conflict of interest.
Financial support
The study was supported by a grant from Arak University of Medical Sciences,Arak,Iran.
Institutional review board statement
The protocol of study was approved by the Ethical Committee of Arak University of Medical Sciences with IR.ARAKMU.REC.1397.140 on August 19,2018.In addition,it was registered in Iranian Registry of Clinical Trials with IRCT20141209020258N97 on February 22,2019.
Declaration of patient consent
The authors certify that they have obtained patients consent forms.In the form,patients have given their consent for the images and other clinical information to be reported in the journal.The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Reporting statement
The writing and editing of the article was performed in accordance with the CONsolidated Standards of Reporting Trials (CONSORT)Statement.
Biostatistics statement
The statistical methods of this study were reviewed by the biostatistician of Qom University of Medical Sciences,Iran.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement
Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access journal,and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License,which allows others to remix,tweak,and build upon the work non-commercially,as long as appropriate credit is given and the new creations are licensed under the identical terms.
杂志排行
Medical Gas Research的其它文章
- High-flow hydrogen inhalation might suppresses the immune function of middle-aged participants:a selfcontrolled study
- Evaluation of audible leak versus pressure volume loop closure for polyvinyl chloride cuff and polyurethane microcuff in endotracheal tube inflated with air:a prospective randomized study
- The role of nitric oxide in peptic ulcer:a narrative review
- Therapeutic effects of hyperbaric oxygen:integrated review
- A new mechanistic approach for the treatment of chronic neuropathic pain with nitrous oxide integrated from a systems biology narrative review
- Hyperbaric oxygen therapy decreases mortality due to Fournier’s gangrene:a retrospective comparative study
