Lacrimal sac lymphoma: a case series and literature review
2022-10-24FengXiMengHanYueYiQunYuanRuiZhangYiFeiYuanYingWenBiJiangQian
Feng-Xi Meng, Han Yue, Yi-Qun Yuan, Rui Zhang, Yi-Fei Yuan, Ying-Wen Bi,Jiang Qian
1Department of Ophthalmology, Eye & ENT Hospital of Fudan University, Shanghai 200031, China
2Laboratory of Myopia, Chinese Academy of Medical Sciences, Shanghai 200031, China
3NHC Key Laboratory of Myopia, Fudan University, Shanghai 200031, China
4Department of Pathology, Eye & ENT Hospital of Fudan University, Shanghai 200031, China
Abstract
● KEYWORDS: lacrimal sac tumor; lacrimal drainage apparatus; non-epithelial lacrimal sac tumor; lymphoma;mucosal-associated lymphoid tissue lymphoma
INTRODUCTION
Tumors that originate from the lacrimal sac are rare, but without early diagnosis and proper intervention, they can be life-threatening. As many as 55% of the lacrimal sac tumors (LSTs) are malignant and those of epithelial origin account for the majority[1-6]. Non-epithelial malignant tumors of the lacrimal sac are exceedingly rare[7], and most have been reported as solitary cases rather than case series.
Non-epithelial LSTs are roughly divided into four histopathological categories: mesenchymal tumors, hemopoietic tumors, melanoma,and granulocytic sarcoma[8-9]. In previous literature, lymphoma has been reported as the most common pathological type among the non-epithelial malignant tumors of the lacrimal sac[7,10]. Similar to systemic lymphomas, lacrimal sac lymphomas (LSLs) also present diverse subtypes according to the World Health Organization (WHO) classification of lymphoid tumors[11], indicating different clinical outcomes.
To identify the clinical features of LSLs and to review our experience in the management, we retrospectively investigated eight cases of LSL and analyzed the clinical and histopathological data, with the hope of aiding oncologists in diagnosing this rare disease.
SUBJECTS AND METHODS
Ethical ApprovalThis study adheres to the tenets of the Declaration of Helsinki, and all the conducts of this study were reviewed and approved by the Institutional Review Board of Eye and ENT Hospital of Fudan University, Shanghai, China.
SubjectsThis retrospective study included 64 cases of lacrimal sac malignant tumors obtained from all inpatients at our hospital from 1986 to 2020. Clinical data regarding sex, age, and diagnosis were analyzed. Among the 64 cases,there were 8 cases of primary LSLs, in whom all remained as primary lymphomas until the conclusion of the study.Further detailed information about these 8 cases was carefully examined, including clinical symptoms, imaging features,preoperative treatments, therapeutic conductions, pathological reports, and long-term follow-up.
Histopathological ExaminationIn all the 8 LSL patients, the histopathological specimens were stained with hematoxylin and eosin. The immunohistochemical markers of CD3, CD5,CD10, CD20, CD23, CD43, CD79α, cyclin D-1, and MIB-1 were also applied to determine the exact subtypes of lymphoma.Diagnoses were made according to the WHO lymphoma classification system[11]. All the diagnoses of the 8 LSLs patients were confirmed by three experienced pathologists. For pending cases, gene rearrangement was conducted.
RESULTS
Pathological Classifications of 64 Primary MalignantLacrimal Sac LymphomasSixty-four cases of malignant LSTs were diagnosed and treated in our hospital over 25y (January 1986 to December 2020). Among them, 51 (80%, 31 males, and 20 females) were found to be epithelial. The mean age of these patients was 54±13y. The remaining 13 cases (20%, 8 males and 5 females) were of non-epithelial origin, with a mean age of 48±15y. Of the 13 non-epithelial neoplasms, lymphoma was the major pathological type (8 cases). The rest included 3 melanomas, 1 malignant neurinoma, and 1 soft tissue sarcoma.
Lymphoma was the Most Common Type of Non-epithelial Lacrimal Sac LymphomasThere were altogether 8 cases of primary LSLs in the 13 non-epithelial neoplasms. The detailed clinical information was carefully examined as follows (Table 1).
Age and sexThere were 4 males and 4 females among the 8 LSLs, with a mean age of 44±16y. Five neoplasms occurred on the left side and 3 on the right side.
Clinical symptomsAll 8 patients had epiphora in the lacrimal sac for a certain period of time (from 1mo to 5y). Only 1 patient developed the symptom of dacryocystitis. All 8 patients showed no signs of systemic involvement at the first time of clinical visits
History prior to referralOne patient had been prescribed intermittent antibiotic eye drops for 3y. One patient had received dacryocystorhinostomy (DCR), followed by 2“granulation tissue resection” surgeries within 40d before she was referred to our hospital. The other 6 patients had received no medical treatment before visiting our hospital.
Imaging featuresComputed tomography (CT) scans were applied to all the patients. Each patient had a soft tissue mass arising from the lacrimal sac with no bony erosion in the scan images (Figure 1A, 1B). Enhanced CT scans showed slight enhancement of the tumors (Figure 1C). One patient was diagnosed with NK/T cell lymphoma and underwent DCR before being referred to our hospital. The CT images were taken in the initial medical center. According to the electronic medical record, the CT scans showed an irregular soft tissue mass in the lacrimal sac region with orbital medial wall discontinuity.

Figure 1 CT scan images of LSL Axial (A) and coronal (B) orbit CT scan soft tissue window showed a soft. Tissue mass on the left side of lacrimal sac region. CT scan of a patient with LSL (A, B);image of another patient with LSL, slight enhancement of the tumor could be observed in the enhanced CT scan (C). LSL: Lacrimal sac lymphoma.

Figure 2 Haematoxylin and eosin staining of LSLs (×200) showed different histopathological types A: Mucosal-associated lymphoid tissue (MALT) lymphoma; B: Diffused large B-cell lymphoma(DLBCL); C: NK/T cell lymphoma; D: Mantle cell lymphoma(MCL). LSL: Lacrimal sac lymphoma.
Pathological subtypeOf all the 8 patients, 5 were diagnosed with mucosal-associated lymphoid tissue (MALT) lymphoma,1 with NK/T cell lymphoma, 1 with mantle cell lymphoma(MCL), and 1 with diffused large B-cell lymphoma (DLBCL;Figure 2). Among the 5 MALT lymphoma cases, there were 2 males and 3 females, with a mean age of 43y.
Operative and further treatmentAll the patients received either incisional biopsy or dacryocystectomy to remove the tumor completely. According to the pathological examination,the patients received further chemotherapy or radiotherapy or both. The detailed information was listed in Table 1.
ProgressionExcept 1 patient with MALT lymphoma died for unknown reasons 104mo after surgery, the other 7 patients showed no signs of local recurrence or in other organs. The follow-up periods ranged from 38 to 220mo, with an average of 101±66mo.
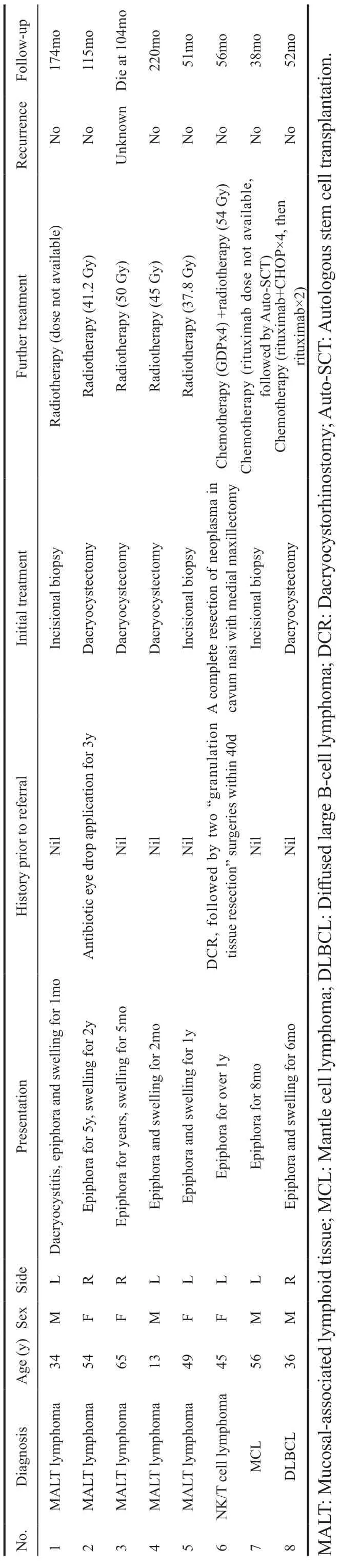
Table 1 Clinical characteristics, treatment, and follow-up information for 8 patients with lacrimal sac lymphoma
DISCUSSION
Malignant LSTs are infrequent, and few reports have been done with large samples. In Stefanyszynet al’s[2]study of 59 malignant LSTs, 44 were of epithelial origin (74.6%). Other reports also demonstrated that non-epithelial malignancies are less common in lacrimal sac[2-4,12]. Lymphoma is the major type of non-epithelial malignant LSTs, accounting for about 6%-13% of all lacrimal sac malignancies[2,7,10,13-14].
LSL may be primary and solitary without systemic involvement[14-16]or secondary to leukemia[17]. Older patients who develop symptoms of dacryocystitis with a known course of systemic lymphoma should be highly suspected for lymphoproliferative infiltration in the lacrimal drainage system[18]. Secondary LSLs tended to be bilateral, and the time interval between the diagnosis of systemic lymphoma and LSL averaged 5.8y[18]. Since lymphoma lesions may exhibit local or distinct recurrence[7]or change to a more aggressive type[19],long-term monitoring is needed.
Akin to lymphoma in ocular adnexal, our study showed that MALT lymphoma was undoubtedly the major subtype of all the LSLs. Kajitaet al[20]summarized all the published LSL cases in Japan, showing 2 DLBCLs, 1 MALT lymphoma,1 peripheral T cell lymphoma, 1 NK cell lymphoma, and 2 medium cell type lymphomas with B-cell markers. In the EORTC study of 15 primary LSLs, there were 5 MALT lymphomas (33.3%), 5 DLBCLs (33.3%), 3 “transitional MALT lymphomas” (being in transition from MALT lymphoma to DLBCL, 20%), and 2 unclassified B-cell lymphomas (13.3%)[19]. In another report from Japan in 2019 which included 5 cases of LSL, there were 3 DLBCL,1 MALT and 1 MCL[21]. Literature based on the western population shows that DLBCL and MALT lymphomas occur with approximately equal frequency[19]. Conclusions from more previous studies vary since the lymphoma classification system has changed considerably over the past few decades.Therefore, issues such as which lymphoma subtype is more likely to occur in the lacrimal sac and differences among races still need to be addressed in greater detail.
The most common initial symptoms of LSLs were epiphora and painless swelling in the area. Only 1 patient had the symptom of dacryocystitis, although previous studies have indicated that chronic dacryocystitis[22-24]may cause LSL.Other signs such as bleeding tears and ulcers in the adjacent skin, which were reported to be common in some epithelial and more aggressive non-epithelial malignancies[2], were not observed in our study.
Imaging examinations such as CT scans or magnetic resonance imaging (MRI) are essential for diagnosing LSL. Both our study and the previous reports showed solid masses in the lacrimal sacs with homogeneous density. Enlargement of the lacrimal ducts and surrounding bone compression could also be observed. Though not as commonly as in epithelial malignancies, bony destruction could be observed in LSLs[25].MRI is more helpful in the differential diagnosis of LSTs since MRI could provide better tumor definition and determination of the cystic or solid nature of the masses. The dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) pattern,as well as its parameters were valuable for the diagnosis of non-typical cases[26]. However, in our retrospective study, we failed to collect the electronic MR images of this rare disease.Future work is needed for a better conclusion on LSL imaging features.
Because of the rarity of LSL, the optimal therapy is not well established. Surgery, radiotherapy, and chemotherapy could all be applied to LSL patients. It is indicated that radiotherapy alone could be considered as an option with curative potential for primary NHL of the lacrimal sac, especially for those who could not tolerate chemotherapy or surgery[3].All MALT patients in our study received radiotherapy with good response, but the dose varies because of the change of practice concept over decades. LSL prognosis seems to be optimistic, as indicated in previous reports[12,19]and in our study.
DCR is the gold standard treatment for nasolacrimal duct obstruction. It could avoid skin scars; however, it is more challenging to detect LSTs. Although rare, there are cases reporting patients diagnosed with malignant lacrimal sac tumor after DCR. Such clinical situations are challenging. Leeet al[27]reported two cases of malignant LSTs discovered in patients with persistent epiphora after receiving DCR. Wide resection of lacrimal sac together with nasolacrimal duct and medial maxillectomy was performed, after which adjuvant radiotherapy was applied. Both patients were under observation at the time of the report. Kanget al[28]have reported ten cases of LSTs. Six patients had a history of DCR for dacryostenosis,and the average number of DCR was 3.5. Five of the 6 patients were diagnosed with malignant epithelial tumors. One patient underwent 10 times DCR, and the tumor involved the orbit, so orbital exenteration was performed with total maxillectomy.No recurrence was detected at the follow-up of 204mo. One patient refused further treatment after dacryocystectomy with wide excision and died 18mo after surgery. The rest 3 patients received medial maxillectomy and radiotherapy and were all alive by the end of the follow-up (from 12 to 143mo). In our case series, only 1 patient diagnosed with NK/T lymphoma had prior DCR history. After complete resection of neoplasm in cavum nasi with medial maxillectomy, both chemotherapy and radiotherapy were applied. Despite the progressiveness of NK/T lymphoma, the patient was free of recurrence after 56mo of the surgery. Therefore, for the malignant lacrimal sac tumor patients with prior DCR history, complete resection of the neoplasm with medial maxillectomy and adjuvant radiotherapy is recommended. Depending on the pathological diagnosis,chemotherapy may also be beneficial.
There is a common limitation of small sample size and weak follow-up in LSL studies. Our study contributes a relatively large sample to this topic, especially on behalf of the Asian population. However, research with larger samples is expected to better understand LSL.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Natural Science Foundation of China (No.81970835); the Science and Technology Commission of Shanghai Municipality, China(No.20Y11911200).
Conflicts of Interest: Meng FX,None;Yue H, None;Yuan YQ,None;Zhang R,None;Yuan YF,None;Bi YW,None;Qian J,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Age-related changes of lens thickness and density in different age phases
- Therapeutic potential of pupilloplasty combined with phacomulsification and intraocular lens implantation against uveitis-induced cataract
- Prophylaxis with intraocular pressure lowering medication and glaucomatous progression in patients receiving intravitreal anti-VEGF therapy
- Optimal timing of preoperative intravitreal anti-VEGF injection for proliferative diabetic retinopathy patients
- Prognosis value of Chinese Ocular Fundus Diseases Society classification for proliferative diabetic retinopathy on postoperative visual acuity after pars plana vitrectomy in type 2 diabetes
- Visual field defects and retinal nerve fiber layer damage in buried optic disc drusen: a new insight
