Extranodal natural killer/T-cell lymphoma (nasal type) presenting as a perianal abscess: A case report
2019-08-14YanNiLiuYongZhuJiaJunTanGuangShuShenShuLiangHuangChunGenZhouShaoHuaHuangfuRuiZhangXiaoBoHuangLingWangQiZhangBinJiang
Yan-Ni Liu, Yong Zhu, Jia-Jun Tan, Guang-Shu Shen, Shu-Liang Huang, Chun-Gen Zhou, Shao-Hua Huangfu,Rui Zhang, Xiao-Bo Huang, Ling Wang, Qi Zhang, Bin Jiang
Abstract
Key words: Extranodal natural killer T-cell lymphoma; Perianal abscess; Lymphoma;Rectal involvement; Case report
INTRODUCTION
Extranodal nasal type NK/T-cell lymphoma (ENKTL), according to the 2016 revision of the World Health Organization classification of lymphoid neoplasms, is a type of invasive non-Hodgkin's lymphoma expressing NK cell (or less frequently T cell)markers. It is a rare disease that accounts for 2%-10% of malignant lymphomas and is most prevalent in Asia and South America[1]. It is most commonly observed in young and middle-aged males and the male to female ratio is about 2-4:1[2]. The nasal cavity is the most common primary site of ENKTL and adjacent tissues are often involved including the skin. Twenty-five percent of cases originate from extranasal tissues,including the gastrointestinal tract, lungs, skin, and testes. There have been only a few reports of ENKTL originating in the anorectal region.
Although the pathogenesis of ENKTL is not fully understood, it has been shown to be closely related to EBV infection[3,4]. The lesions are characterized by vascular invasion and destruction, significant necrosis, expression of cytotoxic molecules (i.e.,granzyme B, perforin, and T cell-restricted intracellular antigen-1 [TIA-1]), and Epstein-Barr virus (EBV) infection[5-8]. Typically, the cells are CD2 and CD56 positive,and surface CD3 negative[9-12]. Moreover, they are usually positive for cytotoxic molecules (such as granzyme B, TIA-1, and perforin), and negative for other T and NK cell-associated antigens, including CD4, CD5, CD8, CD16, and CD57[13-15].
While sinonasal ENKTL has a better prognosis than extranasal disease, its course is usually aggressive with rapid progression, and the prognosis is usually poor with a 5-year survival rate of approximately 30%[16]or even lower in more advanced stages[8,17,18]. Due to the non-specific symptoms, the disease is difficult to diagnose.Here we present a case of ENKTL in the rectum initially diagnosed and treated as a perianal abscess.
CASE PRESENTATION
Chief complaints
Anal discomfort for 22 d after surgery and fever for two days.
History of present illness
A 24-year-old female patient was admitted to our hospital for routine perianal abscess incision and drainage surgery. The surgery was performed in January 2016. Thirteen days after the surgery, she was discharged in good condition. Twenty-two days after the discharge, the patient was readmitted to the hospital because of anal discomfort that started just after the discharge. Two days before readmission, the patient developed a fever.
History of past illness
The patient reported no past illnesses.
Personal and family history
The patient was previously healthy and her family history was unremarkable.
Physical examination upon admission
After admission, the doctor found that apart from a 2 cm surgical wound localized at the 6 o’clock position, a digital rectal examination revealed a prominent 3-4 cm lesion localized laterally from the surgical wound at the 7 o’clock position and extending upwards to the 11 o’clock position. Blood was present in the stool.
Laboratory examinations
Routine laboratory analysis showed leukocytosis with neutrophilia (white blood cells 16.12 × 109/L, 81.91% neutrophils); increased levels of inflammatory markers (Creactive protein: 15.2 mg/L; prealbumin: 106.00 mg/L; albumin: 30.60 g/L; total protein: 48.20 g/L), cholinesterase (111.00 U/L), and creatine kinase (21.00 U/L).
Imaging examinations
Endorectal ultrasonography showed a hypoechoic area under the mucosa located 5 cm laterally from the 8-12 o’clock position of the anal margin in the anal canal. The mass was diagnosed as a submucosal infection. Enteroscopy showed hyperplasia and adhesions on the rectal mucosa at the margin of the perianal incision, which was diagnosed as proctitis. Biopsy samples were taken during endoscopy (Figure 1).Pathological examination revealed moderate to severe acute and chronic mucositis,inflammatory necrosis, and granulation tissue hyperplasia (Figure 2).
On days 3, 10, 16, and 23 of hospitalization, the patient underwent several anal exploration and hemostasis surgeries due to recurrent anal hemorrhage. The source of bleeding remained unidentified. Twenty-two days later, the patient was transferred to a secondary reference hospital for a laparoscopic assisted pelvic exploration and ileostomy. Excessive purulent secretions and necrotic tissue around the anus were observed in colonoscopy. In magnetic resonance imaging (MRI), thickening and edema of the rectum and external genital organs were observed along with multiple exudations and small lymph nodes around the rectum (Figure 3). After the surgery,continuous irrigations and drainageviaan anal double cannula was performed. The patient was still feverish and suffered from very extensive, bloody discharge from the anus resulting in hypovolemic shock. Sigmoid colostomy with rectal and anal resection was suggested, but the patient did not consent to surgery and so after symptomatic treatment, she was discharged on request.
For the next 4 mo, the patient was treated conservatively in an outpatient clinic,however, the symptoms returned and the patient was readmitted to hospital. In addition to the perianal abscess, rectal vaginal fistula and inflammation of perianal tissue were diagnosed. On the seventh day of admission, the anorectal abscess was resected and the pelvic abscess was drained. A biopsy of the left inguinal lymph nodes was performed. Histopathological and immunohistochemical examinations showed the presence of CK (-), LCA (+), CD2 (+), CD3 (+), CD4 (-), CD5(-), CD8(partial), CD56 (+), CD10 (-), CD20 (-), CD30 (partial), CD15 (-), CD79a (-), CD138 (-),CylinD1 (-), TIA (-), EMA (-), CD7 (-), granzyme B (+), perforin (+), and CD57 (-) cells that suggested a diagnosis of ENKTL (Figure 4). The Ki67 index was 65%.
Two weeks later, before the histopathological results were available, the patient was transferred to a tertiary reference hospital. The results of lymphocyte immunoassay are shown in Table 1.
FINAL DIAGNOSIS

Figure 1 Colonoscopy images showing necrotic tissue and erosion at the edge of the anal margin (black arrows).
A PET-CT scan performed after the transfer showed a thickened rectal wall,pathological mass in the perianal area with multiple exudations and gas in the peripheral fat space, enlarged spleen, pathological mass in the right nasal cavity, and thickened posterior wall of the trachea. In the scan range, the skin was irregularly thickened and high-density, subcutaneous shadows were visible (left neck, chest,abdomen, and left hip). Generalized lymphadenopathy (bilateral axillary, abdominal,pelvic cavity, and left inguinal) was observed, in line with the diagnosis of lymphoma. In addition, signs of sinusitis and nodular foci of increased metabolism in left margin of L3 vertebral body and left iliac crest were visible (Figure 5). The images of nasopharyngeal biopsy were typical for ENKTL (Figure 6). Immunohistochemistry showed CD20 (-), CD3 (+), CD2 (+), CD56 (+), and TIA (+) cells with a Ki67 index of 90%. Fluorescentin situhybridization showed the presence of EBV-encoded small RNAs (EBERs). A final diagnosis of stage IV ENKTL was made.
TREATMENT
Two weeks after the admission, COP chemotherapy was initiated (cyclophosphamide 1.3 g on day 1, vincristine 4 mg on day 1, and prednisone 50 mg b.i.d on days 1-5).However, on day 1, a massive anal hemorrhage resulting in hypovolemic shock occurred. As a result, chemotherapy was stopped and shock management including intravascular fluid therapy and blood transfusions were implemented. The patient’s condition continued to deteriorate despite the treatment.
OUTCOME AND FOLLOW-UP
Three weeks later, the patient was transferred to Jiangbei People's Hospital for conservative maintenance therapy. Three days after the admission, continuous blood oozing from the anus was noted. Intravenous administration of a hemostatic agent(etamsylate and P-aminomethylbenzoic acid) was ineffective in stopping the bleeding.Coagulation panel showed activated partial thromboplastin time 58.40 s (reference value 20-40 s), fibrinogen 1.62 g/L (reference value 2-4 g/L), and D-dimer 2.94 µg/mL(reference value < 0.2 µg/mL). Because of suspected coagulopathy, daily infusions of red blood cells, cryoprecipitate, platelets, and plasma were introduced. Despite shock management, the patient's condition gradually deteriorated and she died 9 mo after presentation.
DISCUSSION
What could raise suspicion of ENKTL in a patient with typical symptoms of a common perianal abscess? The complicated postoperative course of the disease,including persistent fever and recurrent, massive anal hemorrhage resulting in hypovolemic shock not relieved after re-operation and antibiotic treatment, is not a typical course of perianal abscess and should prompt further diagnostic procedures[19].However, as nasopharyngeal symptoms were not evident at the first admission and no abnormalities in imaging and routine laboratory analysis suggested a suspicion of systemic disease, malignancy was not included in the differential diagnosis at an early stage.
Pathological and immunohistochemical examinations of colonoscopy biopsies showed local inflammatory necrosis and inflammatory granulation tissue hyperplasia.This misleading result might be caused by the fact that routine colonoscopic biopsies are superficial and do not reach submucosal tissues potentially containing lymphoma cells. Therefore, one could not suggest changing the primary diagnosis. In such cases,a deep tissue biopsy may improve the accuracy of the diagnosis.
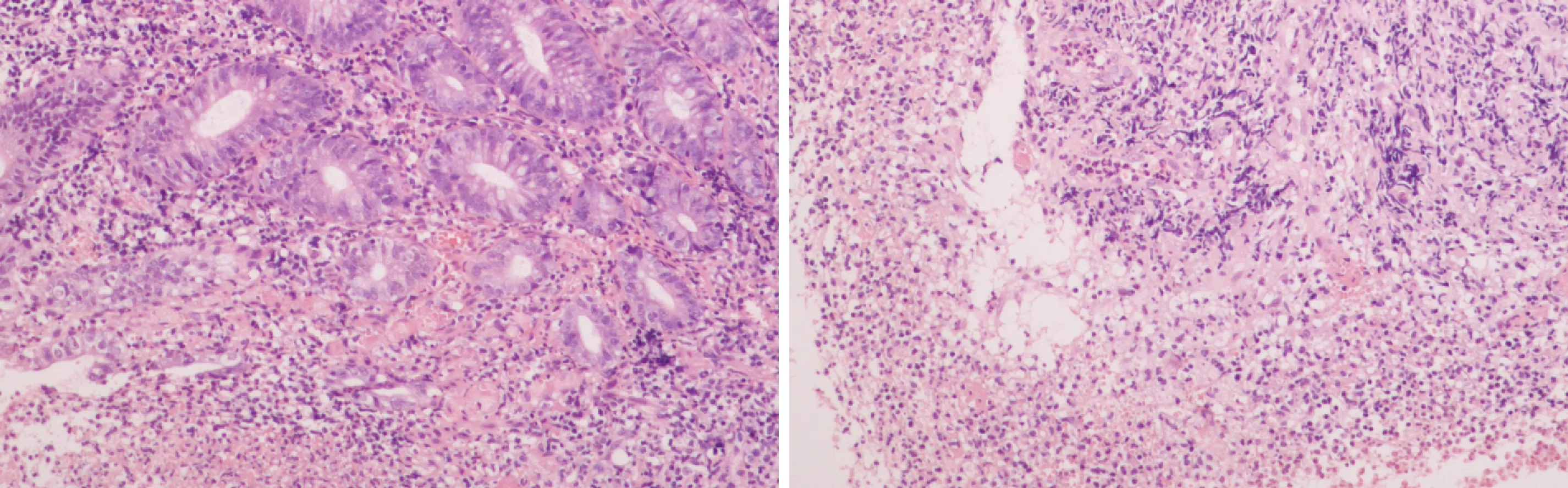
Figure 2 Histopathological examination showing moderate-severe acute and chronic inflammation with inflammatory necrosis and hyperplastic granulation tissue.
In the anal canal, lymphoid tissue is accumulated around the anus where lymphoma cells may block the internal glands of the anus and cause perianal abscess formation. Therefore, in the cases of perianal disease with unexplained blood in the stool, fever, anemia, weight loss, and other systemic symptoms, timely biopsy may facilitate accurate diagnosis and allow initiation of adequate treatment[20,21]. In addition, full-body imaging can further reduce the risk of misdiagnosis.
Lymphoma cases presenting with a perianal abscess are very rare. Ninety percent of the anorectal abscesses are caused by acute infection of the anal glands. In the remaining cases, the abscess is formed as a result of other diseases such as inflammatory bowel disease, tuberculosis, or tumors. Gastrointestinal lymphoma is usually secondary to a wide range of lymph node diseases, and primary gastrointestinal lymphoma is relatively rare[22-24]. There are a few reports on lymphomas in the anorectal area, including ENKTL originating from the rectum. Kakimotoet al[25]reported a case of refractory ulcerative colitis presenting with colonic submucosal tumors histopathologically diagnosed as ENKTL. Valbuenaet al[26]reported a case of a male who underwent rectal resection for clinical suspicion of carcinoma. After histopathologic examination, it was diagnosed as classical Hodgkin lymphoma(nodular sclerosis type) involving the rectum.
CONCLUSION
We present a rare case of fatal, disseminated ENKTL with rectal involvement in which a perianal abscess was initially suggested. Non-specific symptoms and results of imaging, laboratory analysis, and colonoscopic biopsy did not suggest systemic disease and consequently the final diagnosis was delayed. Therefore, a complicated course of surgical treatment, recurrent hemorrhages, and rapid deterioration of patient’s condition should prompt further investigation, and systemic and neoplastic diseases should be included in the differential diagnosis of any potentially benign perianal abscess.

Table 1 Lymphocyte immunoassay results

Figure 3 T2 liposuction magnetic resonance imaging demonstrated edema (A, yellow arrow) and enlarged lymph nodes (B, arrow) around the rectum on diffusion weighted imaging.

Figure 4 Histopathological and immunohistochemical examinations. A-C: Hematoxylin-eosin staining of tumor cells (A, 100× magnification, C, 400×magnification) and tumor-associated necrotic tissue (B, 100× magnification); D-J: immunohistochemical staining for CD2 (D), CD3 (E), CD56 (F), perforin (G),granzyme B (H), TIA-1 (I), and Ki-67 (J).

Figure 5 Positron emission tomography-computed tomography showing increased marker uptake in the kidneys (A) and nasopharyngeal area (B).
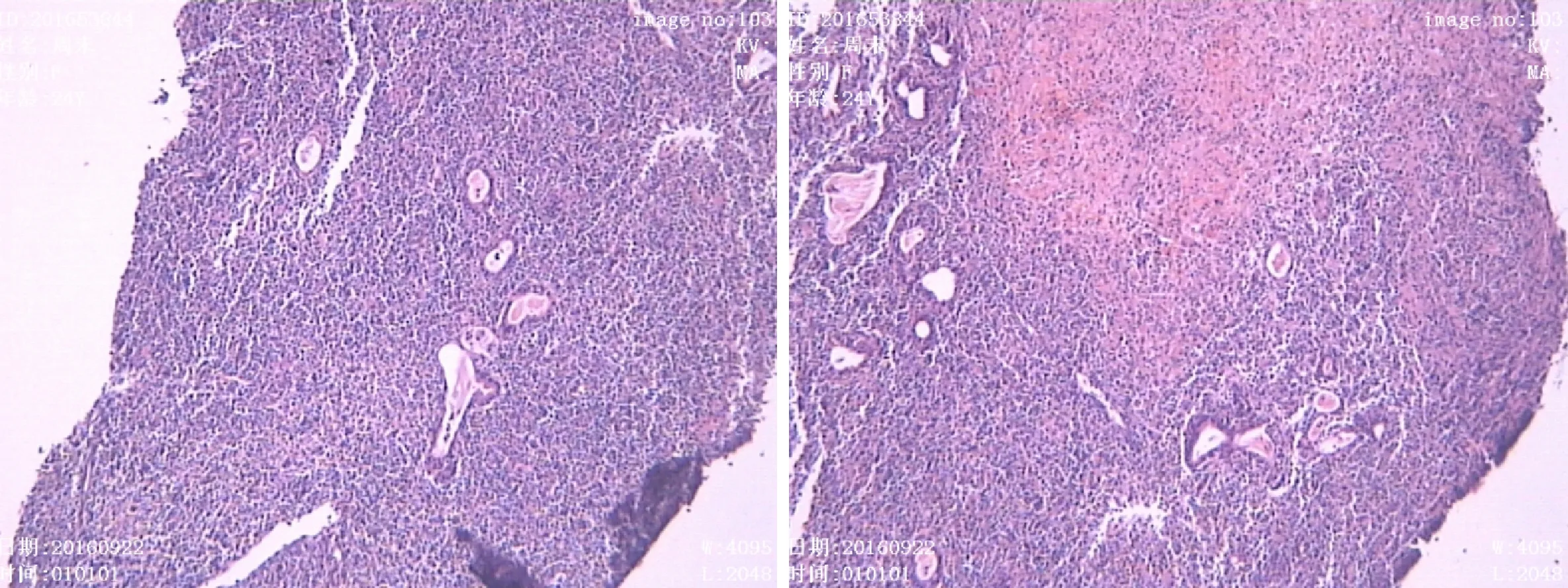
Figure 6 Small-to-moderate size lymphoid tissue hyperplasia with necrosis and apoptosis in nasal endoscopy biopsy.
杂志排行
World Journal of Clinical Cases的其它文章
- Exosomes in esophageal cancer: A review on tumorigenesis,diagnosis and therapeutic potential
- Food additives can act as triggering factors in celiac disease:Current knowledge based on a critical review of the literature
- Optimal use of fielder XT guidewire enhances the success rate of chronic total occlusion percutaneous coronary intervention
- Association between ventricular repolarization variables and cardiac diastolic function: A cross-sectional study of a healthy Chinese population
- Non-invasive home lung impedance monitoring in early post-acute heart failure discharge: Three case reports
- Bilateral adrenocortical adenomas causing adrenocorticotropic hormone-independent Cushing’s syndrome: A case report and review of the literature
