Optimal use of fielder XT guidewire enhances the success rate of chronic total occlusion percutaneous coronary intervention
2019-08-14QianChengWangHaiRuoLinYuanHanHaiDongKaiXuShaoYiGuanZhenHuanChenHuiXinHaoJianPingBinYuLinLiaoQuanMinJing
Qian-Cheng Wang, Hai-Ruo Lin, Yuan Han, Hai Dong, Kai Xu, Shao-Yi Guan, Zhen-Huan Chen, Hui-Xin Hao,Jian-Ping Bin, Yu-Lin Liao, Quan-Min Jing
Abstract
Key words: Chronic total occlusion; Percutaneous coronary intervention; Anterograde wire escalation; Parallel wire technique; Fielder XT guidewire; Success rate
INTRODUCTION
Coronary chronic total occlusion (CTO), defined as a lesion with total occlusion exhibiting thrombolysis in myocardial infarction (TIMI) grade 0 flow in a native vessel for more than 3 mo, is found in 18%-31% of patients who undergo invasive coronary angiography[1,2]. Successful recanalization of CTOs has been shown to be associated with reduced risks of death, coronary artery bypass grafting[3], recurrent angina pectoris[4]and increased long-term survival[5,6]. In addition, failure of CTOpercutaneous coronary intervention (CTO-PCI) is reported to be associated with higher subsequent mortality and more frequent major adverse cardiovascular events(MACE)[7]. Although experience and the introduction of new devices have improved the success rate of PCI[8], CTO-PCI is still technically challenging. The most common reason for CTO-PCI failure is the failure of the guidewire to cross the occlusion segment[9]. Recently, the Fielder XT guidewire was specifically designed for CTO lesions. It has a soft, tapered polymer-jacketed tip, and has been introduced and used worldwide.
To validate whether Fielder XT guidewire can increase the success rate of PCI in CTO lesions, we retrospectively compared data from 1230 consecutive patients with CTO who received PCIviathe anterograde approach at our institution from January 2013 to December 2015. We hypothesized that the use of Fielder XT guidewire can increase the success rate of CTO-PCIviathe anterograde approach.
MATERIALS AND METHODS
Study population
Between January 2013 and December 2015, 1230 consecutive patients with CTO who received PCIviathe anterograde approach at the General Hospital of Northern Theater Command. The study protocol was approved by the local ethics committee,and all procedures were performed according to current international guidelines[10,11].All patients provided written informed consent. We conducted a retrospective analysis of these 1230 patients.
Definitions
CTO was defined as a lesion with total occlusion exhibiting TIMI grade 0 flow in a native vessel for more than 3 mo. Estimation of the occlusion duration was based on the first onset of angina symptoms, prior history of myocardial infarction (MI) in the target vessel territory, or comparison with a prior angiogram. Procedural success was defined as angiographic success (final residual diameter stenosis < 20% and TIMI grade 3 flow following recanalization of the CTO). Clinical success was defined as successful PCI with the patient discharged alive.
Criteria for choice of donors
Patients were candidates for interventio n if they had sufficient cardiac function to lie in the supine position for at least 2 h. To minimize confounding factors, only patients undergoing primary anterograde CTO-PCI whose target vessel was ≥ 2.5 mm in diameter were included in this study. Patients were excluded if they had more than one CTO treated during the same PCI procedure, or if there was no clear evidence for CTO duration ≥ 3 mo.
Study design
Based on the use of Fielder XT guidewire, the patients were divided into two groups:the XT group (n =686) and the no-XT group (n =544). Both groups were compared for clinical parameters, lesion-related characteristics, procedural outcomes and inhospital complications.
CTO-PCI procedure
All interventional procedures were performed using standard techniques. The selection of arterial access depends on the characteristics of the target lesions.Generally, puncture of one of the right radial arteries or right femoral arteries was performed. If necessary, puncture of two arteries among the right radial artery, left radial artery, right femoral artery and left femoral artery were performed. We preferred the Amplatz Left guiding catheter when performing CTO-PCI of the right coronary artery, and we preferred the EBU or the Extra Backup guiding catheter when performing CTO-PCI of the left anterior descending (LAD) and left circumflex artery.The anterograde wire escalation (AWE) strategy was employed for anterograde crossing of the CTO. AWE was usually started with a soft (tip load = 0.8 g), tapered polymer-jacketed guidewire (such as Fielder XT, Asahi Intecc, Japan), a tapered polymer-jacketed guidewire (such as Pilot 50, Abbott, United States), a stiff guidewire(such as Miracle 6, Asahi Intecc), or a stiff, tapered guidewire (such as Conquest,Asahi Intecc).
AWE technique was always performed using an over-the-wire system (such as Finecross microcatheter, Terumo, Japan, or Corsair microcatheter, Asahi Intecc) to support the guidewire. A microcatheter allowed rapid exchange of guidewires, while maintaining wire position and improving guidewire torque response. Microcatheters also improve support and enable dynamic alterations of the penetration power of the guidewire by changing the distance between the microcatheter tip and wire tip. Some of the preferred wires are able to cross the CTO lesions either directly or with the support of the over-the-wire system. If the first soft wire entered the subintimal space of the occlusion segment and failed to cross the CTO lesion, we upgraded to a stiff,tapered wire for crossing using the parallel wires technique. If the first wire could not enter the proximal cap of the CTO lesion, we used a higher-tip-load tapered wire to puncture the proximal cap and then downgraded to a softer, tapered polymerjacketed guidewire to cross the occlusion. If the CTO had tortuous vessels or unclear vascular anatomy, the knuckle wire technique was usually attempted with a polymerjacketed guidewire (such as Fielder XT or Pilot 50). Other techniques including the buddy wire technique, multiwire plaque crushing, subintimal tracking and reentry,and balloon jailing were also employed as required. All PCI procedures were performed by experienced interventionists who handled at least 50 cases of CTO-PCI annually.
Statistical analysis
Continuous variables are presented as the mean ± SD, and categorical data are presented as numbers (proportions). The data were statistically analyzed using Pearson’sχ2test for categorical variables, and Students’ttest was used to compare the quantitative data. Significant independent factors and risk ratio with 95% confidence interval (CI) were assessed by multivariate logistic regression analysis. Analyses were performed using SPSS software (version 21.0; SPSS Inc., Chicago, IL, United States),andP <0.05 (2-sided) was considered statistically significant.
RESULTS
Patients
A total of 1230 patients aged from 31 to 88 years were enrolled, with 74.8% (898/1230)of the patients being male and 55.8% (686/1230) of the patients in the XT group. The overall success rate was 83.9% (1032/1230).
Arterial access
The right radial arterial access percentage is 38.4% (472/1230); the right femoral arterial access percentage is 6.3% (77/1230); the right and left radials arterial accesses percentage is 33.1% (407/1230); the right radial arterial and right femoral arterial accesses percentage is 17.1% (210/1230); the right and left femoral arterial accesses percentage is 5.2% (64/1230).
Parameters predicting the success of CTO-PCI
According to backward logistic regression analysis by Wald’s method, the following factors were positively correlated with successful CTO-PCI: Use of Fielder XT guidewire (P =0.005, 95%CI: 1.172-2.380) and systolic blood pressure (P =0.011,95%CI: 1.003-1.022), while factors negatively associated with procedural success were blunt stump (P =0.013, 95%CI: 1.341-11.862), male sex (P =0.016, 95%CI: 0.363-0.902),New York Heart Association (NYHA) class (P =0.035, 95%CI: 0.553-0.979), contrast amount (P =0.018, 95%CI: 0.983-0.998) and occlusion time (P =0.009, 95%CI: 0.994-0.999) (Table 1).
Clinical characteristics in the two groups
Based on the use of Fielder XT guidewire, the patients were divided into two groups:The XT group (n =686; 55.8%) and the no-XT group (n =544; 44.2%). When clinical characteristics from the two groups were compared, we found no significant differences based on male sex (P =0.313), age (P =0.062), height (P =0.064), body weight (P =0.645), body mass index (P =0.112), systolic blood pressure (P =0.146),diastolic blood pressure (P =0.365), hypertension (P =0.782), diabetes mellitus (P =0.988), previous stroke (P =0.521), old MI (P =0.587), previous PCI (P =0.431),previous renal insufficiency (P =0.513), smoking (P =0.325), alcohol drinking (P =0.887), left ventricular ejection fraction (P =0.587), left ventricular end-diastolic diameter (P =0.559), serum creatinine (P =0.577), cardiothoracic ratio (P =0.089),NYHA heart function class (P =0.643) or age ≥ 65 years (P =0.585) (Table 2).
Lesion-related characteristics in the two groups
The groups were further compared for lesion-related characteristics. The two groups did not differ significantly in terms of multivessel coronary artery disease (P =0.609),lesion calcification (P =0.423), tortuosity (P =0.124), bridging collaterals (P =0.665),blunt stump (P =0.787), J-CTO score (P =0.077), Rentrop class (P =0.686), CTO vessel(P =0.570), occlusion length (P =0.876), or occlusion time (P =0.796) (Table 3).
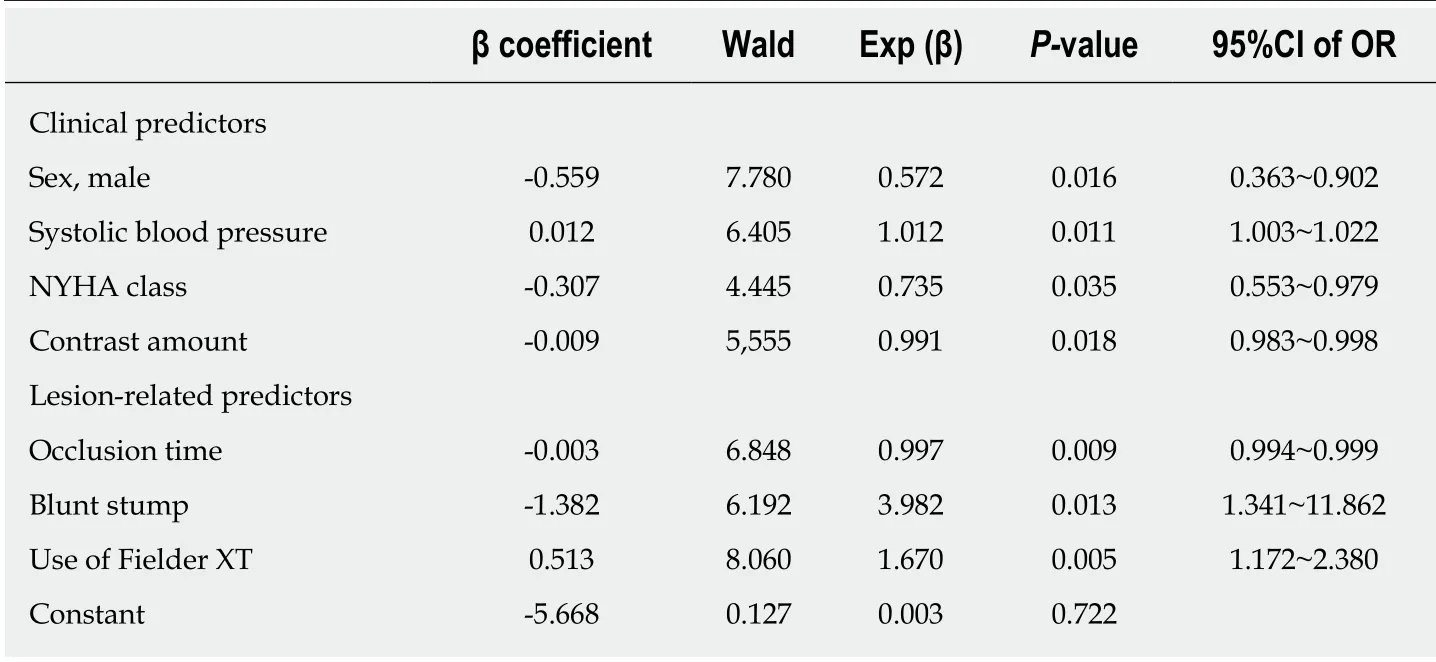
Table 1 Parameters predicting success of chronic total occlusion-percutaneous coronary intervention
Procedural outcomes and in-hospital complications
When the procedural outcomes and in-hospital complications were compared between the two groups, there were no significant differences in coronary artery rupture [3 (0.4%)vs8 (1.5%),P =0.056], in-hospital death [2 (0.3%)vs6 (1.1%),P =0.079] or in-hospital target lesion revascularization (TLR) [3 (0.4%)vs7 (1.3%),P <0.099] (Table 4); however, there were significant differences with regard to success rate [602 (87.8%)vs430 (79.0%),P <0.001], procedure time [(74 ± 23)vs(83 ± 21),P <0.001], stent length [(32.0 ± 15.8)vs(37.3 ± 17.6),P <0.001], contrast amount [(148 ± 46)vs(166 ± 43),P <0.001], post-PCI MI [43 (6.3%)vs59 (10.8%),P =0.004], MACE [44(6.4%)vs57 (10.7%),P =0.007], side branch loss [31 (4.5%)vs44 (8.1%),P =0.009],contrast-induced nephropathy (CIN) [29 (4.2%)vs40 (7.4%),P =0.018] and no reflow[8 (1.2%)vs14 (2.9%),P =0.034] (Table 4).
DISCUSSION
This retrospective study investigated the use of Fielder XT guidewire in CTO-PCIviathe anterograde approach. We focused on the relationship between the use of Fielder XT guidewire and the success rate of CTO-PCI, and evaluated the occurrence of inhospital complications in two groups. The main novel findings of this study are as follows: (1) The use of Fielder XT guidewire contributes to increasing the success rate of CTO-PCIviathe anterograde approach; and (2) The use of Fielder XT guidewire is associated with reduced rates of in-hospital complications and stent implantations.
The AWE technique is the most common strategy for CTO-PCI, and polymerjacketed guidewires are most frequently used to implement this strategy. Although Karatasakiset al[12]recently reported that the use of stiff polymer-jacketed guidewires results in a high CTO crossing rate without increasing the incidence of MACE or perforation[12], we found that a soft, tapered polymer-jacketed Fielder XT (Figure 1)guidewire was also effective in crossing the occlusion. Consistent with our results, the Euro-CTO club has recommended starting with a soft (tip load < 1 g), tapered polymer-jacketed guidewire, not only because of high success rates but also because of the low risk of distal vessel damage if the wire fails to cross the lesion[13]. The existence of microchannels, which partly or completely connect from the proximal cap to the distal end of CTO lesions[14](Figure 2A), has also been reported to predict procedural success[15]. Single wiring displays a high success rate as the initial PCI strategy for CTO of the LAD, and is generally performed with a tapered guidewire such as Fielder XT[16](Figure 2B). The diameter of the Fielder XT guidewire is 230 µm,while the diameters of the microchannels range from 160 to 230 µm[14]. Therefore, it is reasonable to select Fielder XT as the initial guidewire. Additionally, microchannels frequently end at the sidewall of the coronary artery or connect to the side branches far proximal to the distal end of the CTO lesion. Some of these microchannels may run longitudinally through the lesion from the proximal to the distal lumen for up to 85%of the total length of the CTO (Figure 2A). The initial soft, tapered polymer-jacketed guidewire can easily enter the proximal cap through microchannels, but the wirefrequently goes into the sidewall of the coronary artery and results in forming intimal dissection (Figure 2C). It may also go into the side branches of the occlusion segment(Figure 2D). In such situations, the parallel wire technique, which is based on a middle-hard guidewire with a tapered tip, is the best approach to solve the problem.First, the initial guidewire in the false lumen or side branch is left both as a marker and to obstruct the false channel. Second, a second tapered guidewire is used to trace the exact path as the first wire. After the tip of the second guidewire reaches the point where the first guidewire appeared to divert from the true lumen, the tip of the second guidewire is intentionally directed into the true lumen (Figure 2E and F). In this case, the second guidewire usually has a high crossing rate and a low side branch occlusion rate. If the second guidewire fails to enter the true lumen, the AWE strategy for CTO will usually involve switching from a middle-hard guidewire with a tapered tip to a stiff guidewire with a tapered tip. If the initial guidewire had already crossed the occlusion segment and entered the subintimal region of the distal cap (Figure 2G),an anterograde dissection reentry (ADR) strategy can be employed. This is usually attempted to minimize the length of the dissection by reentry into the distal true lumen using a stiff guidewire with a tapered tip immediately after the distal cap of the occlusion segment (Figure 2H). If an initial stiff guidewire has been used to puncture the proximal cap, it is important to downgrade to a soft, tapered polymerjacketed guidewire, such as Fielder XT, to reduce the risk of perforation and increase the chance of tracking the vessel[17].

Table 2 Clinical characteristics in the two groups, n (%)
In the present study, we found that a strategy based on the initial use of Fielder XT guidewire significantly increased the success rate of CTO-PCIviathe anterograde approach. This may have been partially attributable to the existence of microchannels with a diameter of approximately 160-230 µm in the CTO lesions. The number of microchannels has been reported to decrease with CTO maturation[18]. Other studies have reported that these channels can exist in loose tissues extending from the proximal to distal fibrous caps in CTOs of any age[19]. Thus, successful tracking of microchannels in loose tissue may be possible, even in very old CTOs[20]. Consistentwith these data, we found that the use of Fielder XT guidewire significantly increased the success rate of CTO-PCI, although there were no significant differences in occlusion time between the two groups.

Table 3 Lesion-related characteristics in the two groups, n (%)
Nevertheless, factors predicting the success or failure of CTO-PCI are contextdependent. In agreement with previous studies, we noted that blunt stump[21-24]was an independent predictor of the procedural success of CTO-PCI. In recent years,multiple scoring systems have been established to predict the procedural success,efficiency, and complications of CTO-PCI[21-26]. Both the multicenter CTO registry in Japan (J-CTO) and clinical- and lesion-related (CL) scores include blunt stump as the lesion-related predictor[21,23]. CTO with blunt stump is a major obstacle to successful intervention. If the proximal cap has a blunt morphology, the occlusion is often more mature[17]. Older occlusions usually have harder proximal caps and lack microchannels connected to the proximal cap, which prevent the initial soft, tapered polymer-jacketed guidewire from entering the proximal cap. Thus, the blunt stump of proximal cap is an obstacle to the procedural success of CTO-PCI[17]. In accordance with the results of previous studies, we also found that contrast amount, procedure time and cardiac function were independent predictors of procedural success.Algorithms also provide specific guidance, suggesting that operators should consider stopping a CTO procedure if the procedure time is > 3 h, or more than 3.7 mL × the estimated glomerular filtration rate of contrast has been used[17]. Systolic blood pressure is closely related to cardiac function, and systolic blood pressure was thus an independent predictor of procedural success in this study. Furthermore, females have lower J-CTO scores than males. The technical success rate is usually higher in females than in males[27], consistent with our observed outcomes.
In summary, we found in this study that the use of Fielder XT guidewire was associated with a relatively shorter procedure time and lower contrast amount, as Fielder XT guidewire could cross CTO lesions into the distal true lumen by microchannels. The amount of contrast media is closely related to the incidence ofCIN, and several studies have shown that the volume of contrast media is an independent risk factor for the development of contrast-induced acute kidney injury[28-30]. We observed a similar outcome in which the volume of contrast media was positively associated with CIN incidence. We also found that the use of Fielder XT guidewire was associated with lower rates of in-hospital complications and stent implantation. Furthermore, the initial soft, tapered polymer-jacketed guidewire we used could cross the CTO lesion and reach the distal cap, with lower likelihoods of dissection and a smaller degree of hematoma than stiff guidewires. ADR based on the soft guidewire we used above could also ensure true lumen reentry once through the CTO segment, which decreased the length of the implanted stent and reduced side branch loss. Additionally, MI of perioperative caused by the occlusion of side branches after CTO-PCI was avoided.

Table 4 Procedural outcomes and in-hospital complications in the two groups
In conclusion, the use of Fielder XT guidewire shortens the procedure and increases the success rate of CTO-PCI, and is also associated with reduced complication rates.

Figure 1 An illustrative image of the Fielder XT guidewire.
ARTICLE HIGHLIGHTS
Research background
Chronic total occlusion (CTO) is found in 18%-31% of patients who undergo coronary angiography. Successful recanalization of CTOs has been shown to be associated with reduced recurrent angina pectoris rates and increased long-term survival. Although the success rate of CTO percutaneous coronary intervention (CTO-PCI) has improved, CTO-PCI remains technically challenging. The Fielder XT guidewire was designed for CTO lesions. To validate whether the use of the guidewire increases the success rate, we compared the results of CTO-PCI with or without the guidewire. We hypothesized that the use of Fielder XT guidewire can increase the success rate of CTO-PCI.
Research motivation
Although experience and the introduction of new devices have improved the success rates of PCI, CTO-PCI is still technically challenging. We thus wanted to validate whether the use of Fielder XT guidewire increases the success rate of CTO-PCI.
Research objectives
To investigate whether the use of Fielder XT guidewire increases the final procedural success of CTO-PCIviathe anterograde approach.
Research methods
Between January 2013 and December 2015, a retrospective study was conducted on 1230 consecutive patients with CTO who received PCIviathe anterograde approach at the General Hospital of Northern Theater Command. The patients were divided into an XT Group (n =686)and a no-XT Group (n =544) depending on whether Fielder XT guidewire was used. Both groups were compared for clinical parameters, lesion-related characteristics, procedural outcomes and in-hospital complications. The data were statistically analyzed using a Pearson’sχ2test for categorical variables, and a Students’ttest was used to compare the quantitative data.Significant independent factors and risk ratios with a 95% confidence interval (CI) were assessed by multivariate logistic regression analysis.
Research results
In total, 1230 patients were recruited; 75.4% of the patients were male, and 55.8% of the patients were in the XT group. The overall success rate was 83.9%, with 87.8% in the XT group. Based on multivariate logistic regression analysis, factors positively associated with procedural success were the use of Fielder XT guidewire (P =0.005, 95%CI: 1.172-2.380) and systolic blood pressure(P =0.011, 95%CI: 1.003-1.022), while factors negatively associated with procedural success were blunt stump (P =0.013, 95%CI: 1.341-11.862), male sex (P =0.016, 95%CI: 0.363-0.902), NYHA class (P =0.035, 95%CI: 0.553-0.979), contrast amount (P =0.018, 95%CI: 0.983-0.998) and occlusion time (P =0.009, 95%CI: 0.994-0.999). No significant differences were found between the XT group and the no-XT group with respect to clinical parameters, lesion-related characteristics,coronary artery rupture [3 (0.4%)vs8 (1.5%),P =0.056], in-hospital death [2 (0.3%)vs6 (1.1%),P=0.079] or in-hospital target lesion revascularization [3 (0.4%)vs7 (1.3%),P <0.099]. However,there were significant differences between the groups with respect to success rate [602 (87.8%)vs430 (79.0%),P <0.001], procedure time [(74 ± 23)vs(83 ± 21),P <0.001], stent length [(32.0 ± 15.8)vs(37.3 ± 17.6),P <0.001], contrast amount [(148 ± 46)vs(166 ± 43),P <0.001], post-PCI myocardial infarction [43 (6.3%)vs59 (10.8%),P =0.004], major adverse cardiovascular event [44(6.4%)vs57 (10.7%),P =0.007], side branch loss [31 (4.5%)vs44 (8.1%),P =0.009], contrastinduced nephropathy [29 (4.2%)vs40 (7.4%),P =0.018] and no reflow [8 (1.2%)vs14 (2.9%),P =0.034].
Research conclusions
The use of Fielder XT guidewire shortens the procedure and increases the success rate of CTOPCI, and is also associated with reduced complication rates.
Research perspectives
Larger multicenter studies are required to better understand the relationship between the use of Fielder XT series (such as Fielder XT, Fielder XT-R and Fielder XT-A) guidewires and the procedural success of CTO-PCIviaanterograde, retrograde, or hybrid approaches.
杂志排行
World Journal of Clinical Cases的其它文章
- Exosomes in esophageal cancer: A review on tumorigenesis,diagnosis and therapeutic potential
- Food additives can act as triggering factors in celiac disease:Current knowledge based on a critical review of the literature
- Association between ventricular repolarization variables and cardiac diastolic function: A cross-sectional study of a healthy Chinese population
- Non-invasive home lung impedance monitoring in early post-acute heart failure discharge: Three case reports
- Bilateral adrenocortical adenomas causing adrenocorticotropic hormone-independent Cushing’s syndrome: A case report and review of the literature
- Two case reports and literature review for hepatic epithelioid angiomyolipoma: Pitfall of misdiagnosis
