咪达唑仑滴鼻联合酮咯酸氨丁三醇超前镇痛对小儿麻醉效果的影响
2016-10-21王奕皓帅训军程绍波李会范金鑫艾登斌山东省青岛市市立医院本部麻醉科青岛市临床麻醉研究中心青岛市临床麻醉与疼痛质控中心山东青岛266011
王奕皓 帅训军 程绍波 李会 范金鑫 艾登斌山东省青岛市市立医院本部麻醉科青岛市临床麻醉研究中心青岛市临床麻醉与疼痛质控中心,山东青岛266011
咪达唑仑滴鼻联合酮咯酸氨丁三醇超前镇痛对小儿麻醉效果的影响
王奕皓帅训军程绍波李会范金鑫艾登斌▲
山东省青岛市市立医院本部麻醉科青岛市临床麻醉研究中心青岛市临床麻醉与疼痛质控中心,山东青岛266011
目的探讨咪达唑仑滴鼻联合酮咯酸氨丁三醇超前镇痛对小儿麻醉效果的影响。方法选择2014年1~9月于山东省青岛市市立医院择期行扁桃体和腺样体切除术患儿60例,ASA分级Ⅰ级或Ⅱ级。采用随机数字表法将其分为两组:对照组(C组)和试验组(M组),每组各30例。麻醉诱导前30 min,M组给予咪达唑仑0.2 mg/kg滴鼻,C组给予等容量生理盐水。麻醉诱导前10 min,M组静脉注射酮咯酸氨丁三醇0.5 mg/kg(最大剂量不超过15 mg),C组静脉滴注等容量生理盐水。麻醉诱导:两组均静脉注射芬太尼3 μg/kg、丙泊酚2 mg/kg、维库溴铵0.1 mg/kg。气管插管后机械通气,吸入七氟烷维持麻醉。记录患儿入室镇静情绪评分、面罩接受程度、手术时间及苏醒时间;分别于入室时(T0)、拔除管时(T1)、拔管后5 min(T2)、拔管后10 min(T3)、拔管后30 min(T4)和拔管后1 h(T5)记录患者的心率(HR)、平均动脉压(MAP)、血氧饱和度(SpO2)以及T1~T5时FLACC评分、PAED评分和Ramsay评分,并观察恶心呕吐、低氧血症、呼吸抑制等不良反应发生情况。结果与T0比较,C组在T1~T5时MAP升高;与C组比较,M组术前镇静满意率和诱导面罩接受率升高,在T1~T5时HR和FLACC评分降低,在T1~T4时MAP和PAED评分降低,Ramsay评分升高;差异均有统计学意义(P<0.05)。结论小儿麻醉诱导前咪达唑仑0.2 mg/kg滴鼻联合酮咯酸氨丁三醇0.5 mg/kg超前镇痛可获得良好的镇静作用和安全有效的镇痛效果,且能显著减少苏醒期躁动的发生。
咪达唑仑;酮咯酸氨丁三醇;超前镇痛;苏醒期躁动
[Abstract]Objective To evaluate the influence of intranasal Midazolam combined with the preemptive analgesia with Ketorolac Tromethamine on the analgesia effect in pediatric patients.Methods Sixty ASAⅠorⅡpatients scheduled for elective tonsillectomy and adenoidectomy in Qingdao Municipal Hospital from January to September 2014 were randomized into two groups:control group(group C)and the experimental group(group M),with 30 cases in each group.Midazolam 0.2 mg/kg were given intranasally at 30 min before anesthesia induction in group M,while the equal volume of normal saline was given intranasally in group C.10 min before intubation pediatric,patients in group M were given Ketorolac Tromethamine 0.5 mg/kg(maximum dose less than 15 mg)intravenous injection,while patients in group C were received the equal volume of normal saline intravenous injection.Anesthesia was induced with Fentanyl 3 μg/kg,Propofol 2 mg/kg,and Vecuronium 0.1 mg/kg intravenous injection.After the routine anesthesia induction,endotracheal intubation was performed,and patients were mechanically ventilated.Anesthesia was maintained with Sevoflurane.The sedation scores and the mask acceptance rate after admission to operating room,the time of operation and wake-up were recorded.The heart rate(HR),mean arterial pressure(MAP)and pulse oxygen saturation(SpO2)were recorded after admission to operating room(T0),immediately after removing tube(T1),5 min after extubation(T2),10 min after extubation(T3),30 min after extubation(T4)and 60 min after extubation(T5).The FLACC score,PAED score and Ramsay score were recorded from T1to T5.Adverse reactions were evaluated,such as the nausea and vomiting,hypoxemia and respiratory depression.Results Compared with T0,theMAP elevated at T1-T5in group C;compared with group C,the satisfactory rate of preanesthesia sedation and the mask acceptance rate were higher in group M,the HR and the FLACC score reduced significantly at T1-T4,the MAP and PAED score decreased significantly,while the Ramsay score elevated significantly at T1-T4,;the differences were statistically significant(P<0.05).Conclusion The application that Midazolam 0.2 mg/kg intranasally combined with the preemptive analgesia Ketorolac Tromethamine 0.5 mg/kg before the induction of general anesthesia,not only can obtain better sedation and significant analgesic effect,but also significantly reduce the agitation during recovery period.
[Key words]Midazolam;Ketorolac Tromethamine;Preemptive analgesia;Emergence agitation
小儿身心发育尚不成熟,围术期常伴有紧张、焦虑及恐惧感,影响麻醉诱导和手术的顺利进行,部分患儿术后出现不同程度的人格和行为改变[1],因此小儿麻醉前适度镇静具有重要意义。苏醒期躁动是小儿麻醉常见问题,可明显增加小儿麻醉恢复期风险。疼痛是术后躁动的独立危险因素,小儿疼痛管理较为复杂,多数未得到有效控制[2]。阿片类药物镇痛效果充分,但可导致呼吸抑制、恶心呕吐、痛觉超敏等不良反应[3]。有国外研究[4]证实选择不同镇静、镇痛药物组合,可明显缓解患儿术前紧张焦虑和术后疼痛。本研究拟探讨麻醉前咪达唑仑滴鼻联合酮咯酸氨丁三醇超前镇痛对小儿麻醉效果的影响。
1 资料与方法
1.1一般资料
选择2014年1~9月于山东省青岛市市立医院(以下简称“我院”)拟在全麻气管插管下行扁桃体和腺样体切除术患儿60例,男33例,女27例,年龄3~7岁,体重指数在18~24 kg/m2,ASA分级Ⅰ或Ⅱ级,无阿司匹林过敏史、消化道溃疡史、严重血液系统疾病及出血倾向,近期无服用镇静镇痛药物史。采用随机数字表法将患儿分为两组:对照组(C组)和实验组(M组),每组各30例。本研究已获我院医学伦理委员会批准,并与患儿监护人签署知情同意书。
1.2方法
麻醉前访视患儿,禁食6~8 h,禁饮3~4 h。患儿均肌内注射阿托品0.02 mg/kg后由监护人陪同至手术等候区。麻醉诱导前30 min,M组经鼻滴入咪达唑仑(江苏恩华药业有限公司,批号:20100308)0.2 mg/kg,容量1 mL;C组经鼻滴入等容量生理盐水。麻醉医生监护15 min后与监护人分离转入手术室。监测各项生命体征,开放静脉后M组患儿按0.5 mg/kg静脉注射酮咯酸氨丁三醇(山东新时代药业有限公司,批号:0351 11213),最大剂量为15 mg(均稀释至5 mL);C组患儿静脉注射等容量的生理盐水。10 min后行麻醉诱导:静脉注射芬太尼3 μg/kg、丙泊酚2 mg/kg、维库溴铵0.1mg/kg。气管插管后行机械通气,术中吸入七氟烷维持麻醉,连续监测平均动脉压(MAP)、心率(HR)、血氧饱和度(SpO2)、呼气末二氧化碳分压(PetCO2)、最低肺泡有效浓度(MAC)及BIS值。术毕患儿清醒、反射及呼吸恢复后拔除气管导管,观察5 min后送麻醉苏醒室。
1.3观察指标
由同一名对分组不知情的麻醉护士评估并记录各项指标和评分。采用镇静情绪评分[5]评估患儿入室时状态。1分:哭闹,与父母分离时挣扎;2分:清醒,与父母分离时哭泣;3分:嗜睡,与父母分离时安静;4分,入睡。镇静情绪评分≥3分时,患儿镇静状态满意。记录麻醉诱导时面罩接受程度(接受或不接受),记录手术时间、苏醒时间(停药至患儿气管导管拔除)及苏醒室停留时间,记录入室时(T0)、拔除管时(T1)、拔管后5 min(T2)、10 min(T3)、30 min(T4)和1 h(T5)时的心率(HR)、平均动脉压(MAP)、血氧饱和度(SpO2)以及T1-5时改良面部表情评分法(FLACC)评分[6]、躁动评分(PAED评分)[7]和镇静评分(Ramsay评分)[8],并观察恶心呕吐、低氧血症、呼吸抑制、反流误吸、瘙痒等不良反应发生情况。
1.4统计学方法
采用SPSS17.0统计学软件进行分析,计量资料数据用均数±标准差(x±s)表示,组内比较采用重复测量设计的方差分析,组间比较采用成组LSD-t检验,计数资料用率表示,组间比较采用χ2检验;P<0.05为差异有统计学意义。
2 结果
2.1一般资料比较
两组患儿性别构成比、年龄、体重比较差异无统计学(P>0.05);两组患儿麻醉时间、手术时间、苏醒时间及苏醒室停留时间比较差异无统计学(P>0.05)。见表1。
2.2术前镇静满意率和诱导面罩接受率比较
与C组比较,M组术前镇静满意率和诱导面罩接受率升高,差异有统计学意义(P<0.05)。见表2。
2.3生命体征比较
与T0比较,C组在T1~T5时MAP升高,差异有统计学意义(P<0.05);HR、SpO2差异无统计学意义(P>0.05)。与C组比较,M组在T1~T5时HR降低,在T1~T4时MAP降低,差异有统计学意义(P<0.05),SpO2差异无统计学意义(P>0.05)。见表3。

表1 两组患儿一般资料、手术及术后情况的比较(x±s)
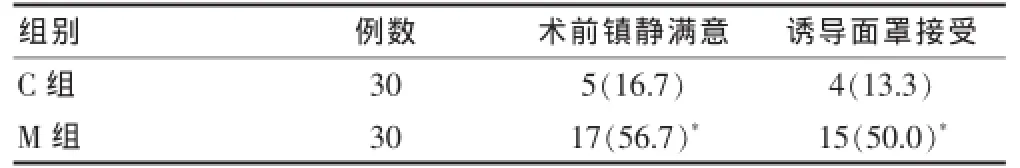
表2 术前镇静满意率和诱导面罩接受率[n(%)]

表3 两组各时点HR、MAP、SPO2比较(x±s)
2.4 FLACC评分、PAED评分和Ramsay评分比较
与C组比较,M组T1~T5时疼痛评分降低,T1~T4时躁动评分降低,镇静评分升高,差异均有统计学意义(P<0.05)。见表4。

表4 两组患儿不同时点FLAACC、PAED、Ramsay评分的比较(分,x±s)
2.5不良反应比较
两组均未发生恶心呕吐、低氧血症(SpO2<90%)、呼吸抑制、反流误吸、瘙痒等不良反应。
3 讨论
咪达唑仑是目前临床广泛应用的麻醉前镇静药,其给药途径有口服、静脉注射、肌内注射和鼻内给药,口服起效快但生物利用度低,肌内注射可产生明显注射痛,可增加患儿恐惧感[9-11]。有研究证实,咪达唑仑经鼻给药后吸收迅速,最大药物浓度和血药浓度-时间曲线下面积同剂量呈正相关,生物利用度可达(60± 23)%[12]。国外有研究显示,咪达唑仑滴鼻后镇静作用起效时间和警觉恢复时间均短于口服[13]。因此本研究选择滴鼻作为咪达唑仑术前用药方式。
本研究中,M组术前镇静满意率和诱导面罩接受率均显著高于C组,提示咪达唑仑0.2 mg/kg滴鼻可明显缓解小儿术前紧张焦虑,产生明显的镇静作用,与国内外研究[14-16]报道的术前鼻内应用咪达唑仑(0.2~0.5 mg/kg)的结果一致。本研究中,M组术前镇静满意率为56.7%,而国外研究[17]显示咪达唑仑滴鼻后患儿与父母分离时镇静满意率达93%,可能与情绪镇静评分的主观性有关,另外增加咪达唑仑滴鼻剂量能否提术前镇静满意率,及其安全性有待于进一步研究。
酮咯酸氨丁三醇是可供临床静脉注射的非选择性环氧化酶(COX-2)抑制剂,无成瘾性和呼吸抑制,应用于2~16岁儿童急性疼痛或术后镇痛的安全性和有效性已得到证实[18-19]。静脉注射或肌内注射30 min内产生镇痛作用,1~2 h血药浓度达峰值,持续4~6 h[20]。本次研究中,M组T1~T5时FLACC评分明显低于C组,表明超前应用酮咯酸氨丁三醇可为行腺样体和扁桃体切除术的患儿提供良好的术后镇痛效果,与国外报道结论一致[21]。本研究在诱导前10 min超前静脉注射酮咯酸氨丁三醇(0.5 mg/kg),经麻醉诱导和手术准备,切皮时已产生镇痛效应,术毕患儿苏醒时镇痛作用正处于峰值,充分发挥其超前镇痛作用。本研究C组MAP在T1~T5时较T0时升高,M组MAP较T0时差异无统计学意义,提示术前应用咪达唑仑和酮咯酸氨丁三醇镇静镇痛可使患儿术后血流动力学更稳定。M组在T1~T5时MAP和HR低于对照组,T1~T4时PAED评分和Ramsay评分高于对照组,提示术前咪达唑仑(0.2 mg/kg)滴鼻联合静脉注射酮咯酸氨丁三醇(0.5 mg/kg)可在术后维持适度的镇静效果和镇痛作用,有效预防苏醒期躁动的发生。
本研究所有患儿术后均未出现鼻咽出血、呼吸抑制及苏醒延迟等不良反应,且围术期血流动力学无明显波动,提示咪达唑仑鼻内给药是安全有效的方式,与国外研究[22]报道的结论相似。本研究M组鼻腔给药后部分患儿出现短暂面色潮红,鼻咽部不适,国外也有类似文献报道[12],考虑咪达唑仑注射液的pH为3.5,呈弱酸性所致,因此适合鼻腔应用的咪达唑仑剂型和用药预处理措施有待进一步研究。
综上所述,对于择期行扁桃体和腺样体切除术患儿,全麻诱导前咪达唑仑滴鼻联合酮咯酸氨丁三醇超前镇痛可产生良好的术前镇静作用,安全有效的术后镇痛效果,显著减少苏醒期躁动的发生,明显提高小儿麻醉舒适度。
[1]Kogan A,Katz J,Efrat R,et al.Premedication with Midazolam in young children:a comparison of four routes of administration[J].Prediatric Anaesth,2002,12(8):685-689.
[2]Patricia D Scherrer.Safe and sound:pediatric procedural sedation and analgesia[J].Minnesota Medicine,2011,94(3):43-47.
[3]Benya min R,Trescot AM,Datta S,et al.Opioid complications and side effects[J].Pain Physician,2008,11(2Suppl):S105-S120.
[4]Doyle L,Colletti JE.Pediatric Procedural Sedation and Analgesia[J].Pediatr Clin North Am,2006,53(2):279-292.
[5]Dalens BJ,Pinard AM,Létourneau DR,et al.Prevention of emergence agitation after sevoflurane anesthesia for pediatric cerebral magnetic resonance imaging by small dose of keta mine or nalbuphine ad ministerd just before discontinuing anesthesia[J].Anesth Analg,2006,102(4):1056-1061.
[6]Merkel SI,Voepel-Lewis T,Shayevitz JR,et al.Extracted from The FLACC:a behavioral scale for scoring postoperative pain in young children[J].Pediatr Nurse,1997,23(3):293-297.
[7]Frederick HJ,Wofford K,De LDG,et al.A Randomized Controlled Trial to Deter mine the Effect of Depth of Anesthesia on Emergence Agitation in Children[J].Anesth Analg,2016,122(4):1141-1146.
[8]Jacobi J,Fraser GL,Coursin DB,et al.Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult[J].Critical Care Medicine,2002,30(1):119-141.
[9]Conway A,Rolley J,Rolley J.Midazolam for sedation before procedures[J].Cochrane Database of Systematic Reviews,2016,5(5):9-12.
[10]Gazal G,Fareed WM,Zafar MS,et al.Pain and anxiety management for pediatric dental procedures using various combinations of sedative drugs:a review[J].Saudi Pharm J,2016,24(4):379-385.
[11]原皓,邹亮,孙莉.全麻术中应用咪达唑仑镇静的安全性及有效性临床分析[J].医学综述,2015,21(7):1337-1339.
[12]Wermeling DP,Record KA,Archer SM,et al.A pharmacokinetic and pharmacodynamic study,in healthy volunteers,of a rapidly absorbed intranasal Midazolam formulation[J].Epilepsy Res,2009,83(2-3):124-132.
[13]Kay L,Reif PS,Belke M,et al.Intranasal Midazolam during presurgical epilepsy monitoring is well tolerated,delays seizure recurrence,and protects from generalized tonicclonic seizures[J].Epilepsia,2015,56(9):1408-1414.
[14]Aynur A,Adnan B,Aliye E,et al.Dexmedetomidine vs Midazolam for premedication of pediatric patients undergoing anesthesia[J].Pediatric Anesthesia,2012,22(9):871-876.
[15]Baldwa NM,Padvi AV,Dave NM,et al.Atomised intranasal Midazolam spray as premediation in pediatric patients:comparison between two doses of 0.2and0.3 mg/kg[J].J Anesth,2012,26(3):346-350.
[16]于威威,季海音,薛航,等.咪达唑仑滴鼻用于小儿术前药的效果观察[J].实用药物与临床,2014,17(7):838-841.
[17]Otsuka Y,Yusa T,Higa M.Intranasal Midazolam for sedation before anesthesia in pediatric patients[J].The Japanese Journal of Anesthesiology,1994,43(1):106-110.
[18]Dsida RM,Wheeler M,Bir mingham PK,et al.Age-stratified pharmacokinetics of Ketorolac Tromethamine in pediatric surgical patients[J].Anesth Analg,2002,94(2):266-270.
[19]VadiveluN,GowdaAM,UrmanRD,etal.Ketorolactrometha mine-routes and clinical implications[J].Pain Pract,2015,15(2):175-193.
[20]Sinha VR,Kumar RV,Singh G.Ketorolac trometha mine formulations:an overview[J].Expert Opin Drug Deliv,2009,6(9):961-975.
[21]Butrón-López FG,Vázquez-Labastida AB,Avila-CastilloA,et al.Preemptive analgesia for postoperative pain with preoperative IM ketorolac trometha mine vs.parecoxib sodium and postoperative oral ketorolac trometha mine vs.valdecoxib[J].Revista Mexicana de Anestesiologia,2005,28(1):27-31.
[22]Stephen MC,Mathew J,Varghese AM,et al.A Randomized controlled trial comparing intranasalmidazolam and chloral hydrate for procedural sedation in children[J]. Otolaryngol Head Neck Surg,2015,153(6):1042-1050.
Influence of intranasal Midazolam combined with the preemptive analgesia with Ketorolac Tromethamine on the analgesia effect in pediatric patients
WANG YihaoSHUAI XunjunCHENG ShaoboLI HuiFAN JinxinAI Dengbin▲
Department of Anesthesiology,Qingdao Municipal Hospital,Shandong Province,Qingdao Municipal Clinical Research Center of Anesthesiology,Qingdao Municipal Clinical Anaesthesia and Pain Quality Control Center,Shandong Province,Qingdao266011,China
R614.2
A
1673-7210(2016)09(a)-0100-04
2016-06-05本文编辑:任念)