核苷和核苷酸类药物治疗慢性乙型肝炎的长期性
2015-08-12参加慢性乙型肝炎长期治疗讨论会专家
参加慢性乙型肝炎长期治疗讨论会专家
核苷和核苷酸类药物治疗慢性乙型肝炎的长期性
参加慢性乙型肝炎长期治疗讨论会专家
【摘要】核苷和核苷酸类药物(NAs)已成功用于慢性乙型肝炎(CHB)治疗。目前一致认为,乙型肝炎病毒(HBV)复制是肝损伤和疾病进展的关键因素,因此CHB治疗的主要目的是最大限度地持续抑制HBV复制。现已证明,应用NAs长期治疗CHB可明显改善肝脏组织学、逆转肝纤维化或肝硬化,以及减少肝细胞癌的发生。本文对CHB长期治疗的必要性、临床获益及管理进行了综述。
【关键词】肝炎,乙型,慢性;核苷和核苷酸类药物;长期治疗;管理
近20年来,临床和流行病学研究表明,持续、活跃的乙型肝炎病毒(HBV)复制是慢性乙型肝炎(CHB)疾病进展的最重要因素,只有长期抑制HBV复制,才有可能防止疾病进展。但HBV在复制过程中,在肝细胞核内形成共价闭合环状DNA(cccDNA)并可持续存在[1];核苷(酸)类药物(NAs)主要抑制HBV复制的逆转录环节,对cccDNA无直接抑制或清除作用;CHB患者存在特异性免疫功能障碍[2-5],而NAs无直接的免疫调节作用[5]。因此,现有NAs抗病毒治疗很难彻底清除HBV,仅部分HBV e抗原(HBeAg)阳性并伴有明显丙氨酸氨基转移酶(ALT)升高的患者可实现HBeAg血清学转换,甚至HBV表面抗原(HBsAg)消失或HBsAg血清学转换,而大部分CHB患者,尤其是HBeAg阴性CHB和肝硬化患者,需要长期抗病毒治疗[6]。因此,目前国内外CHB管理指南或共识均将治疗目标确定为:最大限度地长期抑制HBV复制,减轻肝细胞炎症坏死和纤维化,延缓和减少肝脏失代偿、肝硬化、肝细胞癌(HCC)及其并发症的发生,从而改善生活质量和延长存活时间[7-10]。为帮助临床医生正确认识NAs治疗的长期性,合理选择抗病毒药物、系统监测其疗效和不良事件并长期随访其临床转归,国内部分肝脏病学和感染病学专家根据国内外最新研究证据,经过认真讨论和反复修改,最终形成本文。
1 NAs长期治疗的必要性
1.1病毒因素HBV复制过程可分6个环节:(1)病毒进入肝细胞浆,其核衣壳被裂解而形成松弛型环状DNA(rcDNA),后者进入肝细胞核,并在病毒DNA聚合酶和宿主酶的作用下,修复rcDNA成为cccDNA;(2)以cccDNA为模板,在宿主细胞RNA聚合酶作用下,转录成4种不同长度的病毒信使RNA(mRNA)和前基因组RNA(pgRNA),翻译HBV的各种蛋白;(3)病毒聚合酶和衣壳化信号共同作用于pgRNA,启动逆转录和核衣壳组装;(4)通过逆转录,合成病毒负链DNA,同时病毒聚合酶消化病毒RNA模板;(5)病毒负链DNA合成后,剩余的RNA作为引物,启动正链DNA合成;(6)完成正链DNA合成,形成rcDNA,同时核衣壳被包被上外膜并作为感染性病毒体分泌至细胞外;或再回到同一个肝细胞核内,扩增或维持cccDNA库[11-14](图1)。
现有的NAs只作用于HBV复制的(3)、(4)、(5)环节,对病毒复制的其他环节无明显作用。因此,cccDNA可在肝细胞内持续存在并作为HBV的复制模板,持续产生子代HBV,感染其他肝细胞。
cccDNA一旦在肝细胞核内形成,即具有高度稳定性,可持续产生子代病毒而不受细胞分裂的影响。据数学模型推算,应用阿德福韦酯(ADV)治疗的患者,需要14.5年才能完全清除其肝细胞核中的cccDNA[1,15]。因此,尽管NAs治疗可有效抑制HBV复制,少数患者可达到HBeAg血清学转换甚至HBsAg消失,但肝细胞核内仍可能残存cccDNA,停药后仍有可能复发[16-18]。
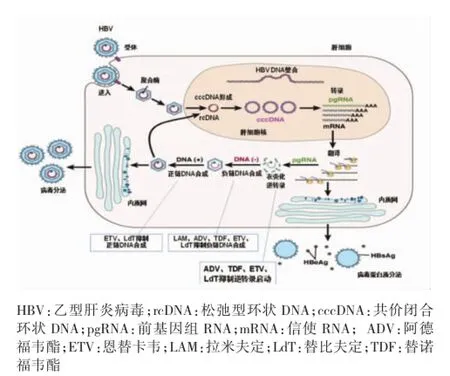
图1 乙型肝炎病毒复制过程及NAs作用靶点
1.2药物因素NAs在细胞内经磷酸化后,生成三磷酸核苷活性产物,通过竞争抑制作用,阻止内源性核苷酸参与HBV DNA的复制,快速有效地减少HBV DNA的合成[19]。有研究表明,ADV、替诺福韦酯(TDF)、恩替卡韦(ETV)和替比夫定(LdT)可抑制逆转录启动;拉米夫定(LAM)、ADV、TDF、ETV 和LdT可抑制病毒负链DNA合成;ETV和LdT可抑制正链DNA合成(图1)[20]。但对HBV复制的中间产物cccDNA不起作用,因此,NAs不能清除在治疗前已存在的,或在治疗过程中因未完全抑制HBV复制而新产生的cccDNA。
此外,cccDNA、HBeAg和HBsAg的减少或清除主要依赖于宿主免疫系统的作用[1,13]。NAs可暂时改善机体对HBV的免疫应答[21-27],但无直接免疫调节作用[5]。尽管NAs可有效降低肝细胞和血清中HBV DNA水平,但对血清中HBeAg和HBsAg水平无明显降低作用[16,18-20]。因此,NAs有限疗程治疗难以达到停药后持久的免疫应答。
1.3宿主因素慢性HBV感染是一个长期的发展过程[7]。在我国,接受NAs治疗的CHB患者中,大部分是在婴幼儿时期感染HBV,其病程较长,一般肝组织学均表现有不同程度的坏死炎症和肝纤维化,甚至肝硬化。但肝脏组织学改善尤其是纤维化改善需要较长的期限。Chang等[22]随访57例经ETV治疗的HBeAg阳性或阴性患者,发现治疗48周时Ishak纤维化评分下降(1者仅为32%(18/57),但治疗至中位时间6年(范围3~7年)时Ishak纤维化评分下降(1者升至88%(50/57)。
1.4临床实践临床实践表明,即使按照国内外现行CHB管理指南或共识建议的标准停药,复发率仍较高(表1)[28-31]。
停药后复发率的高低与巩固治疗时间、判断复发的标准和停药后随访时间有关[38-43]。巩固治疗时间越长,复发率越低[35-36]。Jiang等[35]报道,巩固治疗≥18个月者的复发率(15.4%)明显低于巩固治疗<18个月者(47.5%)。
关于判断复发的标准,各家报道不一。多数报道以病毒学复发为标准,但其标准也不一致,有的以停药后血清中又检测到HBV DNA为复发;有的以停药后血清HBV DNA升高(1000拷贝/ml为复发;也有以停药后血清HBV DNA升高(2000 IU/ml为复发。少数报道以临床复发为标准,但其标准也各异,有的以停药后血清HBV DNA升高(10000拷贝/ml及ALT(2倍正常值上限为临床复发;有的以停药后血清HBV DNA(2000 IU/ml,ALT升高(2倍正常值上限为临床复发。在停药标准、巩固治疗时间和随访时间相同的情况下,一般病毒学复发率高于临床复发率。
停药后随访时间越长,复发率越高。Liu等[43]报道,停药后随访至6、12、24、36、48和60个月,累计病毒学复发率(血清HBV DNA(10 000拷贝/ml)分别为26.2%、43.6%、49.7%、52.1%、56.1%和56.1%,随随访时间延长,复发率升高。
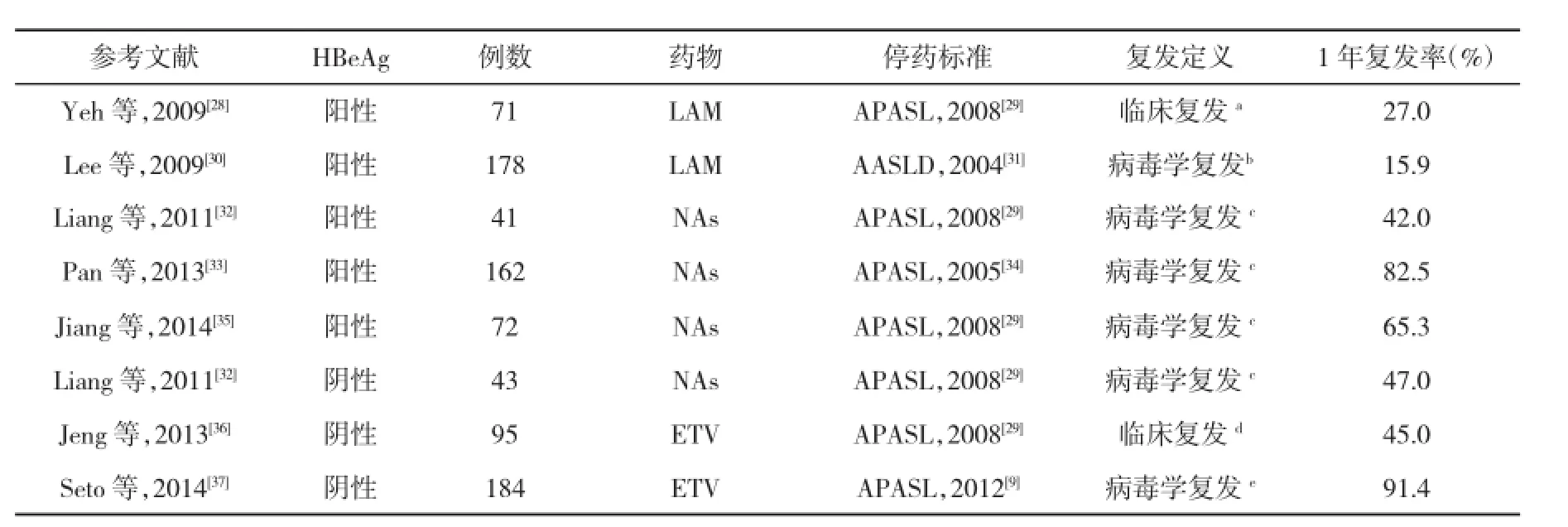
表1 CHB患者NAs治疗停药后复发率
2 NAs长期治疗的临床获益
2.1改善肝脏组织坏死炎症及逆转纤维化和肝硬化应用NAs长期治疗可改善CHB患者的肝组织坏死炎症和纤维化逆转。Dienstag等[44]用LAM治疗CHB患者,随访至中位治疗时间3.5年,56%患者肝组织坏死炎症改善,33%无改变。Xu等[45]应用LAM治疗CHB至10年,19例患者有基线和10年时配对的肝活检标本,结果21%(4/19)肝纤维化/肝硬化完全逆转,47%(9/19)Ishak评分改善,32%(6/19)肝纤维化无改善。Hadziyannis等[46]用ADV治疗70例HBeAg阴性CHB患者,治疗至192周或240周时,分别有86%和83%患者肝组织坏死炎症改善,73%和75%患者纤维化改善。Marcellin等[47]用ADV治疗171例HBeAg阳性CHB患者,其中15例有基线和随访5年的配对肝活检资料,67%患者肝组织坏死炎症改善,60%患者纤维化改善。Liaw[48]报道,641例接受TDF治疗的患者中,489例(76%)完成240周治疗,348例(54%)有基线和240周时肝活检结果,该348例患者中,304例(87%)肝组织学改善,176例(51%)240周时发生肝纤维化逆转(P<0.0001);96例(28%)基线为肝硬化(Ishak评分为5或 6)患者中,71例(74%)患者于240周时肝活检 Ishak评分下降1,表示肝硬化逆转。Schiff等[49]报道,10例进展性肝纤维化或肝硬化患者(基线Ishak评分(4),经ETV累计治疗6年(范围267~297周),所有10例患者的肝脏组织学均改善,Ishak肝纤维化评分和Knodell肝组织坏死炎症评分较基线分别平均下降2.2和7.6分,4例基线为肝硬化患者的Ishak评分均降至4或以下。
2.2逆转或缓解失代偿一项随机非盲研究[50]报道,195例失代偿肝硬化患者应用ETV 1mg/d或ADV 10mg/d治疗,48周时病毒抑制率分别为57%和20%,MELD评分下降为2.6 和1.7。一项双盲研究入组112例CHB失代偿患者,随机分为TDF组(45例)、TDF和恩曲他滨(Truvada)联合治疗组(45例)及ETV组(22例),治疗48周后,3组应答率相同,病毒学应答率(HBV DNA<400拷贝/ml)分别为71%、88%和73%;ALT复常率分别为57%、76%和55%;3组MELD中位评分和CTP评分下降2分及以上者的比例相同[51]。
2.3延缓或阻止肝病进展LAM长期治疗(中位治疗时间89.9个月) 142例HBeAg阳性但无肝硬化患者,其累计肝硬化发生率明显低于124例未治疗的HBeAg阳性对照组[52]。一项双盲随机对照研究[53]表明,用LAM长期治疗(中位治疗时间32.4个月)436例肝硬化患者,与未治疗的215例对照组比较,治疗组和对照组的肝病进展分别为7.8%(34/436)和 17.7% (38/215)(P=0.001)。VIRGIL研究报道[54],ETV中位治疗时间20个月(范围11~32个月)且出现病毒学应答(血清HBV DNA<80IU/ml)的CHB患者,发生失代偿的概率下降71%。
2.4预防和减少HCC的发生多项研究报道,应用LAM长期治疗CHB患者可明显降低HCC发生率[55-58]。Su等[59]报道,666例接受ETV单药治疗肝硬化患者为ETV组,621例未接受治疗患者为对照组,在随访2.7年中,ETV组的HCC发生率为2.4%,对照组为5.2%(P=0.009),降低59%。Wu等[60]对中国台湾健康保险研究数据库(NHIRD)中1997年1月至2010年12月间CHB患者数据进行回顾性分析,纳入21 595 例CHB患者,接受NAs治疗至少3个月,为抗病毒治疗组;另21 595例采用保肝药物治疗的患者作为对照组,结果抗病毒治疗组7年HCC发生率显著低于对照组(7.32%vs 22.7%,P<0.001)。
但也有一些研究报道,NAs长期治疗对CHB患者的HCC发生率无影响[61-70],这可能与研究对象不同(如患者的种族、遗传、年龄、性别、病期、基线HBVDNA和HBsAg水平、HBV基因型、CHB和肝癌家族史等构成不同)、样本量小、随访时间短等因素有关。如TDF治疗6年的注册研究报道,治疗组的HCC年发生率为0.4%,与按REACH-B评分获得的预期HCC发生率比较,最初5年TDF有效治疗对HCC发生率并无影响,但5年后两组的差异有统计学意义[71](图2)。
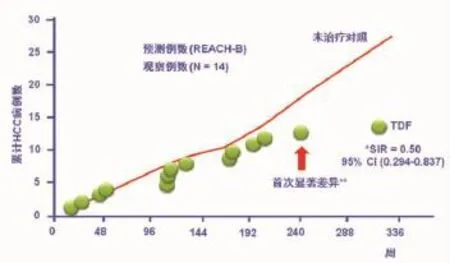
图2 应用TDF单药治疗初治的有或无代偿期肝硬化患者7年观察和预测的累计HCC发生率*SIR=标化发病率比值;**0.05?水平显著差异
3 NAs长期治疗应注意的问题
3.1初治药物选择应用低耐药基因屏障的NAs如LAM长期治疗,可产生较高的HBV耐药突变率。发生耐药突变的患者,特别是肝硬化患者更易发生疾病进展,甚至死亡[53,55]。因此,亚太、欧洲和美国肝病学会的CHB管理共识或指南均推荐,NAs初治患者应选择强效、高耐药基因屏障的药物,即ETV和TDF作为优选或一线单药治疗[8-10]。我国CHB防治指南也建议:“如条件允许,初始治疗时宜选用抗病毒作用强和耐药发生率低的药物”[7]。
3.2依从性患者对长期治疗的依从性不仅与耐药发生有关,还与抗病毒治疗的疗效有关。Hilleret等[72]报道,用ADV治疗至2年时,依从性差的患者血清HBV DNA检测不到的患者比例明显低于依从性好的患者(21%vs42%,P<0.01)。与依从性好的患者比较,依从性差的患者的HBeAg阳性率、血清HBV DNA载量和病毒学突破率均较高[73-75]。
据调查,欧美一些国家CHB患者对NAs治疗的依从性约50%[74-77]。据对我国110个城市741家医院的684名肝病相关临床医师其诊治的LAM经治CHB患者调查结果表明,自行停药换药者为47%~49%,其中治疗1年内自行停药换药者占19%~24%[78]。叶丽华等[79]报道,未遵医嘱用药的患者占16.7%。因此,加强对患者抗病毒治疗依从性的教育刻不容缓。
3.3耐药监测耐药是NAs长期治疗CHB所面临的主要问题之一。耐药可引发病毒学突破、生化学突破、病毒学反弹及肝炎发作,少数患者可出现肝脏失代偿、急性肝衰竭,甚至死亡[80]。临床试验数据表明,LAM、ADV和ETV治疗1年耐药突变率分别为20.0%、0和0;治疗4年耐药突变率分别为64.7%、25.7%和0.9%[79]。ADV治疗HBeAg阳性CHB患者5年累计耐药突变率为14.6%[81]。LdT单药治疗104周耐药突变率为25.8%[82]。根据已发表的数据,TDF治疗5年尚未发现对其耐药的CHB病例。
关于耐药监测,请见参考文献[83]。
3.4安全性由于NAs主要从肾脏排泄,因此,在应用NAs前,应检测患者血清肌酐水平、计算肌酐清除率和估算肾小球滤过率 (eGFR),如肌酐清除率或eGFR<50 ml/min,则应调整NAs治疗剂量。此外,还应对失代偿期肝病、肝硬化、肌酐清除率<60 ml/min、同时合并高血压、蛋白尿、糖尿病、活动性肾小球肾炎、实体器官移植等患者进行肾脏损害的风险评估。
NAs有可能导致肾功能下降[84]。ADV连续使用4~5年,3%的患者出现肾毒性[10]。有研究报道,ADV和TDF治疗可导致Fanconi综合征、肾功能不全、低磷性骨病和骨密度下降等[85-88]。因此,对用ADV或TDF治疗的患者,应定期监测血肌酐并计算肌酐清除率、血磷和骨密度等。
GLOBE研究[89]表明,接受LdT治疗2年的患者中,有3或4级肌酸激酶(CK)升高(7倍正常值上限)者的比例为12.9%,并有2例出现有症状的肌病,如肌疼、肌无力等。Lai等[90]报道,LdT治疗52周时CK升高率为7.5%(51/680),1例于LdT治疗11个月后发生肌病。我国任江波等[91]报道,患者的CK升高率与其LdT治疗时间长短有关,治疗1年者为61.2%,治疗5年者为95.9%;CK升高的严重程度也与治疗时间长短有关,治疗1年时CK 3~4级升高率为4.1%,5年升至14.3%。因此,对接受LdT治疗的患者,应监测血清CK变化和横纹肌疾病的发生。
4 存在问题与未来研究课题
4.1提高抗病毒药物的可及性由于受药物价格、报销政策、认知水平及支付能力等因素的制约,我国仍有许多CHB患者未接受抗病毒治疗;已接受抗病毒治疗的患者,也有许多未采用国内外CHB管理共识或指南所推荐的高效低耐药抗病毒药物治疗。因此,应通过政府部门、学术界、企业界和民间团体之间的良性互动,建立和完善药物审批及价格形成机制,充分发挥政府带量采购和报销政策对降低价格和优先选择药物的强大杠杆作用,以公共卫生策略来推动CHB的临床治疗,尽早实现政府、企业、患方和医方均受益的多赢结局。
4.2制订行业规范,进一步提高我国CHB诊治水平我国目前有相当一部分患者未按现行CHB管理共识或指南的建议进行规范的抗病毒治疗和定期随访。因此,应该充分发挥专业团体的学术引领作用和有关政府部门的规范管理功能,进一步加大对CHB管理共识或指南的宣传推广力度,并制订具有可操作性且有一定强制性的行业规范,提高我国CHB的诊治水平和整体卫生经济效益。
4.3研究更可靠的NAs长期治疗CHB的停药标准和监测指标国内外研究报道,即使按照现行的CHB管理共识或指南建议的标准停药[7-10],停药后的复发率仍高达50%~70%[21]。因此,有必要研究NAs长期治疗CHB更可靠的停药标准和判断停药后复发与否的监测指标,如定量HBsAg水平和特异性免疫学指标等[21,92],将停药后复发率降至更低水平。
4.4研究现有NAs更有效的长期治疗策略有部分肝硬化患者经过长期治疗后发生了逆转,他们有可能停药;但还有相当一部分患者虽经长期治疗有所逆转,仍有严重的肝纤维化,可能需要终身治疗。对肝硬化患者的治疗策略值得进一步研究。
Ning等[93]报道,应用ETV治疗达到病毒学抑制的CHB患者,改用聚乙二醇干扰素(-2a(PegIFN(-2a)治疗,可明显提高HBeAg血清学转换率和HBsAg消失率。但也有不同报道[94]。至今关于NAs与PegIFN(联合或序贯治疗的研究还较少,尚需进行多中心随机对照研究证实。
4.5研究NAs长期治疗的安全性目前用于CHB治疗的NAs中,LAM已有16年历史,最后被批准上市的TDF也有7年临床应用历史。国内外临床研究表明,NAs是安全的。但更长时期的NAs单药或2种NAs联合治疗,以及特殊人群,如肝硬化失代偿、长期服用他汀类药物的患者等应用NAs长期治疗的安全性问题,有待进一步观察和评价。
【参考文献】
[1]Werle-Lapostolle B,Bowden S,Locarnini S,et al.Persistence of cccDNA during the natural history of chronic hepatitis B and declineduringadefovirdipivoxiltherapy.Gastroenterology,2004,126(7):1750-1758.
[2] Busca A,Kumar A.Innate immune responses in hepatitis B virus(HBV)infection.Virol J,2014,11:22.
[3]Glebe D.Recent advances in hepatitis B virus research:a German point of view.World J Gastroenterol,2007,13(1):8-13.
[4]Chan C,Abu-Raddad E,Golor G,et al.Clinical phamacokinetics of alamifovir and its metabolites.Antimicrob Agents Chemother,2005,49(5):1813-1822.
[5]Bertoletti A,Ferrari C.Innate and adaptive immune responses in chronic hepatitis B virus infections:towards restoration of immune control of viral infection.Gut,2012,61(12):1754-1764.
[6]Marcellin P,Asselah T.Long-term therapy for chronic hepatitis B:hepatitis B virus DNA suppression leading to cirrhosis reversal.J Gastroenterol Hepatol,2013,28(6):912-923.
[7]中华医学会肝病学分会,中华医学会感染病学分会.慢性乙型肝炎防治指南(2010年版).中国病毒病杂志,2011,1(1):9-23.
[8]European Association for the Study of the Liver.EASL clinical practice guidelines:management of chronic hepatitis B virus infection.J Hepatol,2012,57(1):167-185.
[9] Liaw YF,Kao JH,Piratvisuth T,et al.Asian-Pacific consensusstatement on the management of chronic hepatitis B:a 2012 update.Hepatol Int,2012,6(3):531-561.
[10]Lok AS,McMahon BJ.Chronic hepatitis B:update 2009.Hepatology,2009,50(3):661-662.
[11]Locarnini S.Molecular virology of hepatitis B virus.Semin Liver Dis,2004,24 Suppl 1:3-10.
[12]Levrero M,Pollicino T,Petersen J,et al.Control of cccDNA function in hepatitis B virus infection.J Hepatol,2009,51(3): 581-592.
[13]Wei Y,Neuveut C,Tiollais P,et al.Molecular biology of the hepatitis B virus and role of the X gene.Pathol Biol(Paris),2010,58(4):267-272.
[14]Abu-Amara M,Feld JJ.Does antiviral therapy for chronic hepatitis B reduce the risk of hepatocellular carcinoma Semin Liver Dis,2013,33(2):157-166.
[15]Wursthorn K,Lutgehetmann M,Dandri M,et al.Peginterferon alpha-2b plus adefovir induce strong cccDNA decline and HBsAg reduction in patients with chronic hepatitis B.Hepatology,2006,44(3):675-684.
[16]Zoulim F.Mechanism of viral persistence and resistance to nucleoside and nucleotide analogs in chronic hepatitis B virus infection.Antiviral Res,2004,64(1):1-15.
[17]Balsano C,Alisi A.Viral hepatitis B:established and emerging therapies.Curr Med Chem,2008,15(9):930-939.
[18]Fung J,Lai CL,Seto WK,et al.Nucleoside/nucleotide analogues inthetreatmentofchronichepatitisB.JAntimicrob Chemother,2011,66(12):2715-2725.
[19]Kamiya N.The mechanisms of action of antivials against hepatitis B virus infection.J Antimicrob Chemother,2003,51(5): 1085-1089.
[20]Gish R,Jia JD,Locarnini S,et al.Selection of chronic hepatitis B therapy with high barrier to resistance.Lancet Infect Dis,2012,12(4):341-353.
[21]Reijnders JG,Janssen HL.Relapse of chronic hepatitis B after discontinuation of nucleos(t)ide analogs:is the glass half full or half empty Hepatology,2013,58(6):1885-1887.
[22]Chang TT,Liaw YF,Wu SS,et al.Long-term entecavir therapy results in the reversal of fibrosis/cirrhosis and continued histological improvement in patients with chronic hepatitis B.Hepatology,2010,52(3):886-893.
[23]Marinos G,Naoumov NV,Williams R.Impact of complete inhibition of viral replication on the cellular immune response in chronic hepatitis B virus infection.Hepatology,1996,24(5): 991-995.
[24]Boni C,Bertolatti A,Penna A,et al.Lamivudine treatment can restore T cell responsiveness in chronic hepatitis B.J Clin Invest,1998,102(5):968-975.
[25]Boni C,Penna A,Ogg GS,et al.Lamivudine treatment can overcome cytotoxic T-cell hyporesponsiveness in chronic hepatitisB:newperspectivesforimmunetherapy.Hepatology,2001,33(4):963-971.
[26]Evans A,Riva A,Cooksley H,et al.Programmed death 1 expression during antiviral treatment of chronic hepatitis B:impact of hepatitis B e-antigen seroconversion.Hepatology,2008,48 (3):759-769.
[27]Zhang JY,Song CH,Shi F,et al.Decreased ratio of Treg cells to Th17 cells correlates with HBV DNA suppression in chronic hepatitis B patients undergoing entecavir treatment.PLoS One,2010,5(11):e13869.
[28]Yeh CT,Hsu CW,Chen YC,et al.你Withdrawal of lamivudine in HBeAgpositivechronic hepatitis B patients afterachieving effective maintained virologicalsuppression.J Clin Virol,2009,45 (2):114-118.
[29]Liaw YF,Leung N,KaoJH,etal.Asian-Pacificconsensus statement on the management of chronic hepatitis B:a 2008 update.Hepatol Int,2008,2(3):263-283.
[30]Lee HW,Lee HJ,Hwang JS,et al.Lamivudinemaintenance beyond one yearafter HBeAg seroconversion is a majorfactor for sustained virologic response inHBeAg-positive chronic hepatitis B.Hepatology,2010,51(2):415-421.
[31]Lok AS,McMahon BJ.Chronic hepatitis B:update of recommendations.Hepatology,2004,39(3):857-861.
[32]Liang Y,Jiang J,Su M,et al.Predictors of relapse in chronic hepatitis B after discontinuation of anti-viral therapy.Aliment Pharmacol Ther,2011,34(3):344-352.
[33]Pan XF,Zhang K,Yang XA,et al.Relapse rate and associated-factor of recurrence after stopping NUCs therapy with different prolonged consolidation therapy in HBeAg positive CHB patients.PLoS One,2013,8(7):e68568.
[34]LiawYF,Leung N,Guan R,et al.Asian-Pacific consensus statement on the management of chronic hepatitis B:a 2005 update .Liver Int,2005,25(3):472-489.
[35]Jiang JN,Huang ZL,He LX,et al.Residual amount of HBV DNA in serum is related to relapse in chronic hepatitis B patients after cessation of nucleos(t)ide analogs.J Clin Gastroenterol,2014.[Epub ahead of print]
[36]Jeng WJ,Sheen IS,Chen YC,et al.Off-therapy durability of response to entecavir therapy in hepatitis B e antigen-negative chronic hepatitis B patients.Hepatology,2013,58(6):1888-1896.
[37]Seto WK,Hui AJ,Wong WS,et al.Treatment cessation of entecavirinAsianpatientswithhepatitisBeantigennegative chronic hepatitis B:a multicentre prospective study.Gut,2014. [Epub ahead of print]
[38]Song BC,Suh DJ,Lee HC,et al.Hepatitis B e antigen seroconversion after lamivudine therapy is not durable in patients with chronic hepatitis B in Korea.Hepatology,2000,32(4 Pt 1):803-806.
[39]Reijnders JG,Perquin MJ,Zhang NP,et al.Nucleos(t)ide analogues only induce temporary hepatitis B e antigenseroconversion in most patients with chronic hepatitis B.Gastroenterology,2010,139(2):491-498.
[40]Fung SK,Wong F,Hussain M,et al.Sustained response after a 2-year course of lamivudine treatment of hepatitis B e antigen-negative chronic hepatitis B.J Viral Hepat,2004,11(5):432-438.
[41]Chan HL,Wang H,Niu J,et al.Two-year lamivudine treatment for hepatitis B e antigen-negative chronic hepatitis B:a double-blind,placebo-controlled trial.Antivir Ther,2007,12(3): 345-353.
[42]Hadziyannis SJ,Sevastianos V,Rapti I,et al.Sustained responses and loss of HBsAg in HBeAg-negative patients with chronic hepatitis B who stop long-term treatment with adefovir. Gastroenterology,2012,143(3):629-636.
[43]Liu F,Wang L,Li XY,et al.Poor durability of lamivudine effectivenessdespitestringentcessationcriteria:aprospective clinical study in hepatitis B e antigen-negative chronic hepatitis B patients.J Gastroenterol Hepatol,2011,26(3):456-460.
[44]Dienstag JL,Goldin RD,Heathcote EJ,et al.Histological outcome during long-term lamivudine therapy.Gastroenterology,2003,124(1):105-117.
[45]Xu B,Lin LY,Xu GG,et al.Long-term lamivudine treatment achieves regression ofadvanced liver fibrosis/cirrhosis in patientswithchronichepatitisB.JGastroenterHepatol,2014. [Epub ahead of print]
[46]Hadziyannis SJ,Tassopoulos NC,Heathcote EJ,et al.Long-term therapy with adefovir dipivoxil for HBeAg negative chronic hepatitis B for up to 5 years.Gastroenterology,2006,131(6): 1743-1751.
[47]Marcellin P,Chang TT,Lim SG,et al.Long-term efficacy and safety of adefovir dipivoxil for the treatment of hepatitis B e antigen-positive chronic hepatitis B.Hepatology,2008,48(3): 750-758.
[48]Liaw YF.Reversal of cirrhosis:an achievable goal of hepatitis B antiviral therapy.J Hepatol,2013,59(4):880-881.
[49]Schiff ER,Lee SS,Chao YC,et al.Long-term treatment with entecavir induces reversal of advanced fibrosis or cirrhosis in patients with chronic hepatitis B.Clin Gastroenterol Hepatol,2011,9(3):274-276
[50]Liaw YF,Raptopoulou-Gigi M,Cheinquer H,et al.Efficacy and safety of entecavir versus adefovir in chronic hepatitis B patientswithhepaticdecompesation:arandomized,open-label study.Hepatology,2011,54(1):91-100.
[51]Liaw YF,Sheen IS,Lee CM,et al.Tenofovir disoproxil fumarate (TDF),emtricitabine/TDF,and entecavir in patients with decompesated chronic hepatitis B liver disease.Hepatology,2011,53(1):62-72.
[52]Yuen MF,Seto WK,Chow DH,et al.Long-term lamivudinetherapy reduces the risk oflong-termcomplicationsofchronic hepatitis B infection even in patients without advanced disease.Antivir Ther,2007,12(8):1295-1303.
[53]Liaw YF,Sung JJ,Chow WC,et al.TheCALM Study Group. Lamivudine for patients with chronichepatitis B and advanced liver disease.N Engl J Med,2004,351(15):1521-1531.
[54]Matsumoto A,Tanaka E,Rokuhara A,et al.The Inuyama Hepatitis Study Group.Efficacy of lamivudine for preventing hepatocellular carcinoma in chronic hepatitis B:a multicenter retrospective study of 2795 patients.Hepatol Res,2005,32(3):173-184.
[55]Di Marco V,Marzano A,Lampertico P,et al.Italian Association for the Study of the Liver(AISF)Lamivudine Study Group,I-taly.Clinical outcome of HBeAg-negative chronic hepatitis B in relation to virological response to lamivudine.Hepatology,2004,40(4):883-891.
[56]Sung JJ,Tsoi KK,Wong VW,et al.Meta-analysis:treatment of hepatitis B infection reduces risk of hepatocellular carcinoma. Aliment Pharmacol Ther,2008,28(9):1067-1077.
[57]Papatheodoridis GV,Lampertico P,Manolakopoulos S,et al.Incidence of hepatocellular carcinoma in chronic hepatitis B patients receiving nucleos(t)ide therapy:a systematic review.J Hepatol,2010,53(2):348-356.
[58]Eun JR,Lee HJ,Kim TN,et al.Risk assessment for thedevelopment of hepatocellular carcinoma:according toon-treatment viral response during long-term lamivudinetherapy in hepatitis B virus-related liver disease.J Hepatol,2010,53(1):118-125.
[59]Su TH,Hu TH,Lin CC,et al.Reduction of hepatocellular carcinoma in hepatitis B related cirrhosis patients with long-term entecavir therapy-an interim report of C-TEAM study.Hepatology,2013,58Suppl 1:301A.
[60]Wu CY,Lin JT,Ho HJ,et al.Association of nucleos(t)ide analogue therapy with reduced risk of hepatocellular carcinoma in patients with chronic hepatitis B-a nationwide cohort study. Gastroenterology,2014,147(1):143-151.
[61]Kumada T,Toyoda H,Tada T,et al.Effect of nucleos(t)ide analogue therapy on hepatocarcinogenesis in chronic hepatitis B patients:a propensity score analysis.J Hepatology,2013,58 (3):427-433.
[62]Papatheodoridis GV,Manolakopoulos S,Touloumi G,et al.Virological suppression does not prevent the developmentof hepatocellular carcinoma in HBeAg-negative chronic hepatitis B patients with cirrhosis receiving oral antiviral(s)starting with lamivudinemonotherapy:resultsofthenationwideHEPNET. Greece cohort study.Gut,2011,60(8):1109-1116.
[63]Fattovich G,Bortolotti F,Donato F.Natural history of chronic hepatitis B:special emphasis on disease progression and prognostic factors.J Hepatology,2008,48(2):335-352.
[64]Papatheodoridis G,Manolakopoulos S,Touloumi G,et al.Hepatocellularcarcinoma(HCC) risk in HBeAg-negative chronic hepatitis B(CHBe-)with or without cirrhosis treated with entecavir:results of the nationwide HepNet Greece Cohort Study. J Hepatol,2013,58Suppl 1:S312.
[65]Lampertico P,Soffredini R,Yurdaydin C,et al.Four years of tenofovir monotherapy for NUC naive field practice European patients suppress HBV replication in most patients with a favourable renal safety profile but do not prevent HCC in patients with or without cirrhosis.Hepatology,2013,58Suppl 1:653A.
[66]Papatheodoridis GV,Dalekos GN,Yurdaydin C,et al.Risk and risk factors of hepatocellular carcinoma(HCC) in Caucasian chronic hepatitis B(CHB)patients with or without cirrhosis treated with entecavir(ETV)or tenofovir(TDF).Hepatology,2013,58Suppl 1:302A.
[67]Cho JY,Paik YH,Sohn W,et al.Patients with chronic hepatitis B treated with oral antiviral therapy retain a higher risk for HCC compared with patients with inactive stage disease. Gut,2014.
[68]Lampertico P,Soffredini R,Vigano M,et al.5-year entecavir treatment in NUC-naive,field-practice patients with chronic hepatitis B showed excellent viral suppression and safety profile but no prevention of HCC in cirrhosis.J Hepatol,2013,58Suppl 1:S306.
[69]Hosaka T,Suzuki F,Kobayashi M,et al.Long-term entecavir treatment reduces hepatocellular carcinoma incidence in patients with hepatitis B virusinfection.Hepatology,2013,58 (1):98-107.
[70]Wong GL,Chan HL,Chan HY,et al.Accuracy of risk scores for patients with chronic hepatitis B receiving entecavir treatment.Gastroenterology,2013,144(5):933-944.
[71]Kim WR,BergT,Loomb R,et al.Long-term tenofovir disoproxil fumarate therapy and the risk of hepatocellular carcinoma.J Hepatol,2013,58Suppl 1:S19.
[72]Hilleret MN,Larrat S,Stanke-Labesque F,et al.Does adherence to hepatitis B antiviral treatment correlate with virological responseandriskofbreakthroughJHepatol,2011,55(6): 1468-1469.
[73]BergT,MarcellinP,ZoulimF,etal.Tenofoviriseffective alone or with emtricitabine in adefovir-treated patients with chronic hepatitis B virus infection.Gastroenterology,2010,139 (4):1207-1217.
[74]World Health Organization.Adherence to long-term therapies: evidence for action[EB/OL].[2014-08-12].http://www.who.int/ chp/knowledge/publications/adherencefull_report.pdf.
[75]Chotiyaputta W,Peterson C,Ditah FA,et al.Persistence and adherence to nucleos(t)ide analogue treatment for chronic hepatitis B.J Hepatol,2011,54(1):12-18.
[76]Lee M,Keeffe EB.Study of adherence comes to the treatment of chronic hepatitis B.J Hepatol,2011,54(1):6-8.
[77]Giang L,Sellinger CP,Lee AU.Evaluation of adherence to oral antiviral hepatitis B treatment using structured questionnaires. World J Hepatol,2012,4(2):43-49.
[78]孙秘书,王贵强,张伟,等.拉米夫定经治慢性乙型肝炎患者治疗现状调查分析.中国预防医学杂志,2012,13(1):18-22.
[79]叶丽华,胡兆琴,李正莲.慢性乙型肝炎患者诊断治疗依从性行为调查.实用肝脏病杂志,2013,16(2):155-156.
[80]An P,Bian L,Yin B,et al.Risk factors of gene-resistantmutations in different nucleosides.Hepato-Gastroenterology,2012,59 (113):228-230.
[81]Zeng MD,Mao YM,Yao GB,et al.Five years of treatment with adefovirdipivoxilinChinesepatientswithHBeAg-positive chronic hepatitis B.Liv Int,2012,32(1):137-146.
[82]Sun J,Xie Q,Tan DM,et al.The 104-week efficacy and safety of telbivudine-based optimization strategy in chronichepatitis B patients:a randomized,controlled study.Hepatology,2014,59(4): 1283-1292.
[83]参加乙型肝炎耐药讨论会专家.核苷和核苷酸类药物治疗慢性乙型肝炎的耐药及其管理.中国病毒病杂志,2013,3(1):1-11.
[84]Pipili C,Cholongitas E,Papatheodoridis G.Review article: nucleos(t)ide analogues in patients with chronichepatitis B virus infection and chronic kidney disease.Aliment Pharmacol Ther,2014,39(1):35-46.
[85]Jung YK,Yeon JE,Choi JH,et al.Fanconi’ssyndrome associated with prolonged adefovir dipivoxil therapy in a hepatitis B virus patient.Gut Liver,2010,4(3):389-393.
[86]Verhelst D,Monge M,Meynard JL,et al.Fanconi syndrome and renalfailure induced by tenofovir:a first case report.Am J Kidney Dis,2002,40(6):1331-1333.
[87]Gaspar G,Monereo A,García-Reyne A,et al.Fanconi syndrome and acute renal failure in a patient treated with tenofovir:a call for caution.AIDS,2004,18(2):351-352.
[88]Pol1 S,Lampertico P.First-line treatment of chronic hepatitis B with entecavir ortenofovir in real-life settings:from clinical trials to clinicalpractice.J Viral Hepat,2012,19(6):377-386.
[89]Liaw YF,Gane E,Leung N,et al.2-Year GLOBE trial results: telbivudine is superior to lamivudine in patients with chronic hepatitis B.Gastroenterology,2009,136(2):486-495.
[90]Lai CL,Gane E,Liaw YF,et al.Telbivudine versus lamivudine in patients with chronic hepatitis B.N Engl J Med,2007,357(25):2576-2588.
[91]任江波,王宇,李红艺,等.替比夫定治疗慢性乙型肝炎期间肌酸激酶升高的观察与分析.中华肝脏病杂志,2012,20(9):641-643.
[92]Chan HL,Wong VW,Tse AM,et al.Serum hepatitis B surfaceantigen quantitation can reflect hepatitis Bvirus in the liver andpredicttreatmentresponse.ClinGastroenterolHepatol,2007,5(12):1462-1468.
[93]Ning Q,Han M,Sun Y,et al.Switching from entecavir to PegIFN alfa-2a in patients with HBeAg-positive chronic hepatitis B:a randomised open-label trial(OSST trial).J Hepatol,2014.
[94]Xie Q,Zhou HJ,Bai XF,et al.A Randomized,open-label clinical study of combined peginterferon alfa-2a(40KD)and entecavir treatment for HBeAg-positive chronic hepatitis B.Clin Infect Dis,2014.参与讨论的专家(按姓氏拼音排序):陈成伟、陈士俊、陈永平、成军、程明亮、窦晓光、段钟平、高志良、侯金林、贾继东、江家骥、李杰、李兰娟、李彤、鲁凤民、茅益民、缪晓辉、宁琴、牛俊奇、任红、孙永涛、谭德明、唐红、唐小平、万谟彬、王贵强、王豪、王慧芬、王宇明、魏来、翁心华、谢青、尤红、张文宏、张欣欣、庄辉
(收稿:2014-10-29)
(本文编辑:陈从新)
DOI:10.3969/j.issn.1672-5069.2015.01.032
通讯作者:100191北京大学医学部病原生物学系和感染病中心(庄辉),E-mail:zhuangbmu@126.com;200040上海复旦大学附属华山医院感染科(翁心华),E-mail:xinhua_weng@fudan.edu.cn
Long-termtreatment of chronic hepatitis B Experts attending the discussion on long-treatment of chronichepatitisBCorrespondingauthors:ZhuangHui,E-mail:zhuangbmu@126.com;WengXinhua,xinhua_weng@fudan.edu.cn
【Abstract】Nucleos(t)ide analogs(NAs)have been successfully used for treatment of chronic hepatitis B. Hepatitis B virus(HBV)replication is now recognized as the key driverof liver injury and disease progression,so the primaryaim of treatment forchronic HBV infection is to maximize sustained suppression of HBV replication to undetectablelevels.The long-term treatment has also beenshown to achieve substantial histological improvement and regression of liver fibrosis orcirrhosis,and reduction of hepatocellular carcinoma.This paper has reviewed the necessity,clinical benefits,and the management of long-term treatment for chronic hepatitis B.
【Key words】Hepatitis B,chronic;Nucleoside and nucleotide analogs;Long-term treatment;Management
