简化肺栓塞严重度指数对老年肺栓塞预后判断价值的探讨
2015-04-23张运剑王晓芳施举红
张运剑,王晓芳,罗 凌,施举红
简化肺栓塞严重度指数对老年肺栓塞预后判断价值的探讨
张运剑1*,王晓芳1,罗 凌1,施举红2
(1北京积水潭医院,北京大学第四临床医学院,呼吸与危重症医学科,北京100035;2中国医学科学院北京协和医院呼吸科,北京,100730)
探讨简化肺栓塞严重度指数(sPESI)对老年肺栓塞(PTE)患者危险分层的价值。采取回顾性病例对照研究,将233例于2002年4月至2015年5月在北京积水潭医院确诊的PTE患者分为老年组(≥65岁,=132)和非老年组(<65岁,=101),对老年和非老年PTE患者的合并症、临床特征、sPESI以及30d病死率进行分析。老年组年龄(76.32±6.77)岁,非老年组年龄(51.93±10.39)岁;30d病死率分别为22.73%和11.88%,两组差异具有统计学意义(=0.033)。老年组合并心功能不全、心律失常、脑血管病、肾功能不全、高血压病、糖尿病及肺炎者较非老年组高,两组差异均有统计学意义(均<0.05)。14.39%的老年患者和13.86%的非老年患者合并肿瘤,差异无统计学意义(=0.908),但两组合并肿瘤的构成不同,老年组以肺癌为主,而非老年组以骨肿瘤占多数。老年组动脉血氧分压低于非老年组[(59.39±11.00)(66.44±13.77)mmHg,=0.002],而肺动脉收缩压、脑钠肽及心肌肌钙蛋白I水平均高于非老年组,两组之间差异有统计学意义(=0.000,=0.003和=0.041)。老年组和非老年组sPESI≥1者分别占73.48%和48.51%,两组差异有统计学意义(=0.000)。老年组内死亡者与存活者比较,sPESI≥1的比例分别为90.00%和68.63%,两者差异有统计学意义(=0.020);死亡老年患者的sPESI均值也高于存活老年患者[(2.23±1.52)(1.18±1.11),=0.001]。sPESI评估老年组和非老年组30d预后的ROC曲线下面积(AUC)分别为0.704(95%CI 0.596~0.812)和0.723(95%CI 0.551~0.896)。sPESI有助于老年PTE患者的危险分层。
老年人;肺栓塞;简化肺栓塞严重度指数;危险分层
急性肺栓塞(pulmonary thromboembolism,PTE)发病率随年龄增长而升高。老年PTE患者合并症多,临床表现不典型,预后影响因素更复杂。简化肺栓塞严重度指数(simplified pulmonary embolism severity index,sPESI)作为一种简单的临床评估量表用于非高危PTE患者的初步危险分层,能简化PTE诊治流程,并得到2014年欧洲心脏病学协会(European Society of Cardiology,ESC)急性肺栓塞诊断和管理指南的推荐[1]。但sPESI是基于整体PTE患者而建立的危险分层方法,其对老年PTE患者预后判断的研究并不多。本文针对老年PTE患者的主要特征以及sPESI与预后的关系进行分析,以期对老年PTE患者进行更合理的危险分层,改善其预后。
1 对象与方法
1.1 研究对象
选取2002年4月至2015年5月北京积水潭医院确诊的PTE患者233例。根据国内外部分研究年龄分组标准[3,4],本研究分为老年组(≥65岁组,=132)和非老年组(<65岁组,=101)。
1.2 诊断标准
根据中华医学会呼吸病学分会制定的《肺血栓栓塞症的诊断与治疗指南(草案)》诊断标准[2],并至少符合以下3项中1项:(1)CT肺动脉造影(computed tomographic pulmonary angiography,CTPA)发现肺动脉内血栓直接证据;(2)肺动脉造影结果阳性;(3)肺核素通气/灌注扫描结果呈高度可能者。233例中CTPA确诊192例,肺动脉造影确诊16例,肺核素通气/灌注扫描诊断19例;另外6例患者因发病时病情危重不能进行以上检查,根据PTE危险因素、临床表现并结合超声心动检查发现右室壁运动幅度降低而室壁不厚或右心室/右心房扩大或发现血栓而诊断。
1.3 临床及检查指标
包括年龄、合并症(肿瘤、心功能不全、心律失常、慢性阻塞性肺病、肺炎、肾功能不全、脑血管病、高血压病、糖尿病、高脂血症、低蛋白血症)、动脉血氧分压(PaO2)、超声心动图估测肺动脉收缩压、心肌肌钙蛋白I(cardiac troponin-I,cTnI)、脑钠肽(brain natriuretic peptide,BNP)、血尿酸(serum uric acid,SUA)。
1.4 预后指标
以sPESI及30d病死率为预后指标。sPESI纳入指标包括以下6项:年龄≥80岁、合并慢性心肺疾病或心功能不全、合并肿瘤、血压<100mmHg(1mmHg=0.133kPa)、脉搏≥110次/min、动脉血氧饱和度<90%,每项计1分。
1.5 统计学处理
应用SPSS19.0软件进行统计学分析。符合正态分布的计量资料以均数±标准差表示,统计方法采用独立样本检验;计数资料以百分率表示,组间比较采用2检验或Fisher精确检验;以sPESI评分作为判断30d内死亡与否的临界值,以敏感度为纵座标,(1−特异度)为横坐标绘制患者30d的受试者工作特征(receiver operating characteristic,ROC)曲线,用ROC曲线下面积(area under curve,AUC)衡量sPESI评分系统判断预后的能力。根据Youden指数(灵敏度+特异度−1)的最大值确定PTE患者30d生存与否的最佳临界值。以<0.05为差异有统计学意义。
2 结 果
2.1 两组患者一般资料比较
老年组132例,男66例,女66例,年龄65~96(76.32±6.77)岁,溶栓治疗3例,死亡30例,30d病死率22.73%。非老年组101例,男59例,女42例,年龄18~64(51.93±10.39)岁,溶栓治疗9例,死亡12例,30d病死率为11.88%。老年组30d病死率较非老年组高,且差异有统计学意义(2=4.555,=0.033)。
2.2 两组患者合并症情况比较
老年组患者合并心功能不全、心律失常(心房颤动)、脑血管病、肾功能不全、高血压病、糖尿病及肺炎的发生率较非老年组高,且差异有统计学意义(均<0.05;表1)。老年组和非老年组分别有19例(14.39%)和14例(13.86%)肿瘤患者,两组差别无统计学意义(=0.908),但两组肿瘤构成不同。老年组以肺癌为主,共8例(非小细胞肺癌7例、小细胞肺癌1例),乳腺癌、肾癌各2例,其余食管癌、肝癌、结肠癌、胆管癌、口腔癌、鼻咽癌及子宫内膜癌各1例;而非老年组以骨肿瘤占多数,共6例(肉瘤4例、恶性间叶肿瘤1例、未分型低度恶性肿瘤1例),子宫内膜癌2例,其余乳腺癌、肾癌、胃间充质瘤、腹膜后恶性梭形细胞瘤、慢性淋巴细胞白血病、多发性骨髓瘤各1例。
2.3 老年组与非老年组辅助检查比较
老年组PaO2低于非老年组,而肺动脉收缩压、BNP及cTnI均高于非老年组,两组之间差异有统计学意义(均<0.05);两组之间D−二聚体、血白蛋白和SUA差异无统计学意义(表2)。
2.4 老年组与非老年组sPESI比较
老年组sPESI≥1分者比例高于非老年组(2=15.248,=0.000;表3)。
2.5 老年组内死亡者与存活者sPESI比较
死亡的老年PTE患者中sPESI≥1分者占90.00%(27/30),而存活的老年PTE患者sPESI≥1分者占68.63%(70/102),两者差异有统计学意义(=0.020)。死亡患者的sPESI均值也高于存活患者(=0.001,95%CI:0.44~1.65;表4)。

表1 老年组与非老年组合并症情况比较

表2 老年组与非老年组主要检查指标比较
SUA: serum uric acid; BNP: brain natriuretic peptide; cTnI: cardiac troponin-I. 1mmHg=0.133kPa

表3 老年组与非老年组sPESI比较
sPESI: simplified pulmonary embolism severity index

表4 老年组内死亡与存活患者sPESI比较
sPESI: simplified pulmonary embolism severity index
2.6 sPESI预测两组患者预后的ROC曲线
sPESI评估老年组和非老年组30d预后的AUC分别为0.704[标准误(standard error,SE)0.055,95%CI 0.596~0.812]和0.723(SE 0.088,95%CI 0.551~0.896;图1,2),两组均有较大AUC,且老年组AUC略小于非老年组。老年组和非老年组的最佳临界值均为1.5,其敏感度、特异度分别为0.633、0.657和0.500、0.865;此临界值时,老年组特异度略低于非老年组。
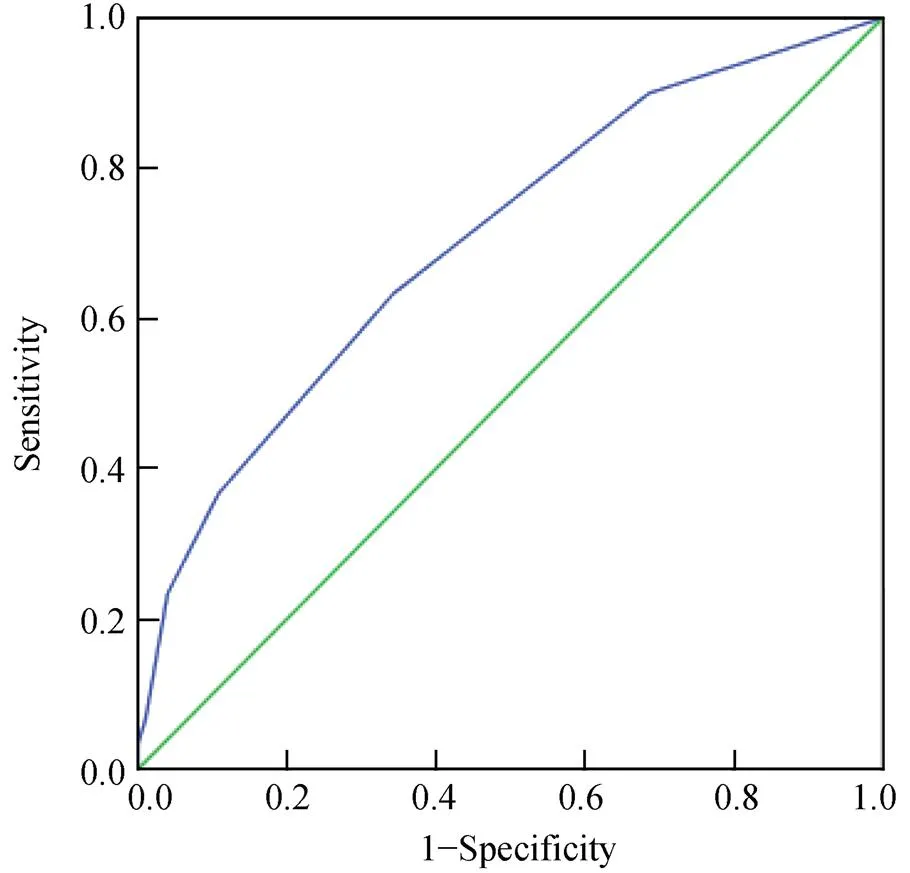
图1 sPESI判断老年患者30d预后的ROC曲线
Figure 1 ROC curve for 30-day mortality in the elderly patients by sPESI ROC: receiver operating characteristic; sPESI: simplified pulmonary embolism severity index
3 讨 论
PTE的发病率随年龄增长而增加,临床表现不典型,病死率高[5]。国外资料显示≥65岁PTE患者30d病死率为14.2%~39.4%[6,7]。老年PTE患者合并症多,既造成诊断困难,又加剧其心肺功能障碍。我们的研究结果显示老年组肺动脉收缩压、BNP及cTnI均较高,而PaO2低于非老年组。老年组PTE患者30d病死率为22.73%,明显高于非老年组的11.88%,主要与老年组有1/3病例合并心功能不全以及脑血管病、肾功能不全、糖尿病、肺炎等因素有关。另外,老年高危PTE患者能溶栓的机会较少,本研究中老年组仅有3例溶栓(2.27%),而非老年组溶栓者9例(8.91%),治疗措施的受限也会增加老年PTE患者的病死率。

图2 sPESI判断非老年患者30d预后的ROC曲线
Figure 2 ROC curve for 30-day mortality in the non-elderly patients by sPESI ROC: receiver operating characteristic; sPESI: simplified pulmonary embolism severity index
对老年PTE患者进行准确危险分层并采取相应治疗措施是改善其预后的关键。目前对PTE的危险分层主要基于临床状况评估、右心功能评价及是否有心肌损伤。sPESI作为一种临床评估量表用于血流动力学稳定的急性PTE患者初步危险分层可以简化诊断流程。国外研究显示sPESI对PTE预后具有较好的预测价值,能节约检查成本并缩短住院时间[8−10]。因此,2014年ESC推荐低危患者(sPESI=0分)可早期出院,而中危患者(sPESI≥1分)需根据右心功能和心肌损伤标志物进一步分层[1]。由于评估sPESI预测价值的资料绝大多数基于整个PTE群体,目前仅有极少数研究显示sPESI可较好地预测≥65岁老年PTE患者的30d病死率[11],因此,有必要进一步研究sPESI对老年PTE患者预后的判断价值。我们研究显示老年PTE患者sPESI≥1分者比例明显高于非老年组,而且老年组内死亡者sPESI评分高于存活者;sPESI对评估老年组和非老年组30d病死率的AUC分别为0.704和0.723,说明sPESI评分系统无论对于老年还是非老年PTE患者均能较好地区分可能死亡和可能存活的患者,有助于老年PTE患者的危险分层。
老年PTE患者合并症多而复杂,在应用sPESI评估预后时应区别对待。本研究中两组sPESI预测30d死亡的最佳临界值均为1.5,但老年组的特异度为0.657,低于非老年组的0.865,这提示判断老年PTE患者预后时还应考虑一些未包括在sPESI评分系统中的因素,如合并脑血管病、肾功能不全、糖尿病、肺炎等疾病。另一方面,sPESI评分系统中只是依据合并症的有或无评分,并未考虑合并症的种类和严重程度。虽然本研究中两组合并肿瘤的比例并无差异,但老年组以肺癌为主。许小毛等[12]研究发现肺癌合并静脉血栓栓塞症者30d病死率高达20.8%。早期国外资料显示子宫内膜癌、淋巴瘤合并静脉血栓栓塞症的死亡风险明显高于乳腺癌和前列腺癌[13]。另外,我们资料显示老年患者合并心房颤动比例明显高于非老年组,有研究者发现PTE合并心房颤动的患者30d病死率高达35.1%[14]。因此,对合并肺癌、心房颤动的老年PTE患者更应重视。基于以上原因,有研究者认为采用疾病累计评分表(Cumulative Illness Rating Scale,CIRS)可能更有利于老年PTE患者预后的判断[15]。
老年PTE患者的预后影响因素多,虽然sPESI未能涵盖某些预后影响因素,但因其简单易于操作,可用于判断血流动力学稳定的老年PTE患者30d病死率。
[1] Konstantinides SV, Torbicki A, Agnelli G,. 2014 ESC Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism[J]. Eur Heart J, 2014, 35(43): 3033−3069.
[2] Society of Respiratory Disease, Chinese Medical Association. Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism(draft)[J]. Chin J Tuberc Respir Dis, 2001, 24(5): 259−264. [中华医学会呼吸病学分会.肺血栓栓塞症的诊断与治疗指南](草案)[J]. 中华结核和呼吸杂志, 2001, 24(5): 259−264.]
[3] Guo DJ, Zhao C, Zou YD,. Values of the Wells and revised Geneva scores combined with D-dimer in diagnosing elderly pulmonary embolism patients[J]. Chin Med J (Engl), 2015, 128(8): 1052−1057.
[4] Minges KE, Bikdeli B, Wang Y,. National trends in pulmonary embolism hospitalization rates and outcomes for adults aged ≥65 years in the United States (1999 to 2010)[J]. Am J Cardiol, 2015, 116(9): 1436−1442.
[5] Spencer FA, Gurwitz JH, Schulman S,. Venous thromboembolism in older adults: a community-based study[J]. Am J Med, 2014, 127(6): 530−537.
[6] Polo Friz H, Molteni M, Del Sorbo D,. Mortality at 30 and 90 days in elderly patients with pulmonary embolism: a retrospective cohort study[J]. Intern Emerg Med, 2015, 10(4): 431−436.
[7] Weberova D, Weber P, Meluzinova H,. Deceased elderly in-patients with pulmonary embolism[J]. Bratisl Lek Listy, 2014, 115(12): 786−790.
[8] Fermann GJ, Erkens PM, Prins MH,. Treatment of pulmonary embolism with rivaroxaban: outcomes by simplified pulmonary embolism severity index score from a post hoc analysis of the EINSTEIN PE study[J]. Acad Emerg Med, 2015, 22(3): 299−307.
[9] Mizuno A, Yamamoto T, Tanabe Y,. Pulmonary embolism severity index and simplified pulmonary embolism severity index risk scores are useful to predict mortality in Japanese patients with pulmonary embolism[J]. Circ J, 2015, 79(4): 889−891.
[10] Barra SN, Paiva L, Providência R,. A review on state-of-the-art data regarding safe early discharge following admission for pulmonary embolism: what do we know[J]? Clin Cardiol, 2013, 36(9): 507−515.
[11] Zwierzina D, Limacher A, Méan M,. Prospective comparison of clinical prognostic scores in elder patients with a pulmonary embolism[J]. J Thromb Haemost, 2012, 10(11): 2270−2276.
[12] Xu XM, Yang H, Qiao LS,. Clinical characteristics and outcomes of lung cancer patients with venous thromboembolism[J]. Chin Med J, 2014, 94(26): 2045−2049. [许小毛, 杨 鹤, 乔立松, 等. 肺癌合并静脉血栓栓塞症患者的临床特点及预后分析[J]. 中华医学杂志, 2014, 94(26): 2045−2049.
[13] Gross CP, Galusha DH, Krumhoiz HM. The impact of venous thromboembolism on risk of death or hemorrhage in older patients[J]. J Gen Intern Med, 2007, 22(3): 321−326.
[14] Barra SN, Paiva LV, Providência R,. Atrial fibrillation in acute pulmonary embolism: prognostic considerations[J]. Emerg Med J, 2014, 31(4): 308−312.
[15] Castelli R, Bucciarelli P, Porro F,. Pulmonary embolism in elderly patients: prognostic impact of Cumulative Illness Rating Scale(CIRS) on short-term mortality[J]. Thromb Res, 2014, 134(2): 326−330.
(编辑: 周宇红)
Predictive value of simplified pulmonary embolism severity index for pulmonary thromboembolism in the elderly
ZHANG Yun-Jian1*, WANG Xiao-Fang1, LUO Ling1, SHI Ju-Hong2
(1Department of Respiratory and Critical Care Medicine, Beijing Jishuitan Hospital, the Fourth Clinical Medical College of Peking University, Beijing 100035, China;2Department of Respiratory Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing 100730, China)
Simplified pulmonary embolism severity index (sPESI) is a practical validated tool aiming to stratify 30-day mortality risk in acute pulmonary thromboembolism (PTE). However, guidelines for PTE risk stratification are not concerning on age. The aim of our study was to determine the prognostic value of sPESI in the elderly patients with PTE.s A retrospective case-control study was carried out on 233 consecutive patients with identified PTE admitted in our hospital from April 2002 to May 2015. They were divided into the elderly group (≥65 years old,=132) and the non-elderly group (<65 years old,=101). Their complications, clinical features, sPESI score, and 30-day mortality were compared and analyzed.The patients of the elderly group were at age of (76.32±6.77) years, and those of the non-elderly group were (51.93±10.39) years. The former group had a 30-day mortality of 22.73%, and the latter of 11.88%, with significant difference between the two groups (=0.033). The incidences of cardiac insufficiency, arrhythmia, cerebrovascular diseases, renal insufficiency, hypertension, diabetes and pneumonia were significantly higher in the elderly patients than in the non-elderly ones (all<0.05). There was no significant difference in the incidence of malignant tumors between the elderly and non-elderly groups (14.39%13.86%,=0.908). But, the most common tumor was lung cancer in the elderly group, and bone tumor in the non-elderly group. The arterial partial pressure of oxygen was significantly lower in the elderly group than in the non-elderly group [(59.39±11.00)(66.44±13.77)mmHg,=0.002], but the pulmonary arterial pressure, serum levels of brain natriuretic peptide and cardiac troponin-I were obviously higher in the former than in the latter (=0.000,=0.003 and=0.041). Significant difference was observed in the percentage of patients with sPESI score ≥1 between the two groups (73.48%48.51%,=0.000). In the elderly group, sPESI score ≥1 was found among 90.00% of the dead patients and 68.63% of the survival ones (=0.020). The mean sPESI score was 2.23±1.52 in the dead patients of the elderly group, significantly higher than those survived (1.18±1.11,=0.001). The area under the receiver-operating characteristic (ROC) curves was 0.704 [95% confidence interval (CI): 0.596−0.812] for the elderly patients and 0.723 (95%CI: 0.551−0.896) for the non-elderly ones.sPESI is helpful for risk stratification in the elderly patients with acute PTE.
aged; pulmonary embolism; simplified pulmonary embolism severity index; risk stratification
(Z141107002514153).
R592; R563.5
A
10.11915/j.issn.1671-5403.2015.12.207
2015−09−01;
2015−10−18
北京市科学技术委员会资助课题(Z141107002514153)
张运剑, E-mail: zhangyjian@126.com
