血浆D−二聚体水平与肺动脉血栓负荷相关性研究
2015-04-23方春晓季颖群李智勇张中和
方春晓,安 俊,季颖群*,孙 博,李智勇,张中和
血浆D−二聚体水平与肺动脉血栓负荷相关性研究
方春晓1,安 俊1,季颖群1*,孙 博2,李智勇2,张中和1
(大连医科大学附属第一医院:1呼吸科,2放射科,大连 116011)
分析血浆D−二聚体(DD)水平与肺动脉血栓负荷的相关性。顺次选取 2009年1月至2011年8月间大连医科大学附属第一医院采用CT肺动脉造影(CTPA)首次确诊急性肺血栓栓塞症(PTE)患者69例。采用Mastora评分系统获得肺动脉阻塞指数(PAOI;PAOI>21.3%提示预后不良风险增加);CT影像测得右(RV)及左(LV)心室短轴直径,计算两者比值(RV/LV>0.9提示右心功能不全)。采用免疫比浊法测定血浆DD。血浆DD浓度中位值为765µg/L(95%CI:750~1205µg/L),PAOI中位值为16.77%(95%CI:16.49%~23.26%)。血浆DD水平与整体肺动脉PAOI呈正相关(=0.417,=0.000)。PAOI>21.3%患者的血浆DD浓度(993μg/L)高于PAOI≤21.3%的患者(663μg/L),差异有统计学意义(=-2.991,=0.003)。血浆DD水平与RV/LV之间呈正相关性(=0.272,=0.024)。RV/LV>0.9患者的血浆DD浓度(880μg/L)高于RV/LV≤0.9的患者(634μg/L),两者之间差异有统计学意义(=-2.070,=0.038)。整体肺动脉PAOI与RV/LV之间呈正相关(=0.390,=0.001)。血浆DD水平与PTE发病时间呈负相关(=-0.407,=0.000);PAOI与发病时间无相关性(=-0.140,=0.245)。老年组(年龄>60岁)患者,其DD水平(727µg/L)和PAOI(14.84%)与非老年组(年龄≤60岁;792.5µg/L,20.97%)比较,差异均无统计学意义(=-0.180,=0.857;=-1.382,=0.167)。规范抗凝3个月后,DD和PAOI水平均显著下降(=-6.976,=0.000;=-7.009,=0.000),二者具有相关性(=0.609,=0.000)。(1)DD水平与CTPA肺动脉新鲜血栓负荷和RV/LV呈正相关,有助于急性PTE患者临床评估病情、指导治疗和判断预后。(2)老年组与非老年组急性PTE患者的DD和PAOI水平差异无统计学意义。
D−二聚体;肺栓塞;肺动脉阻塞指数;CT肺动脉造影
肺血栓栓塞症(pulmonary thromboembolism,PTE)是一种常见并具有潜在致死性的疾病,占心血管系统死亡原因第3位,仅次于心肌缺血及脑血管疾病[1]。由于血浆D−二聚体(D-dimer,DD)水平检测具有快速、定量、价格低、重复性好等优点,其对PTE的阴性预测价值现已得到公认。近年有研究表明血浆DD水平与PTE严重程度呈正相关,也可作为PTE短期及中期死亡率的预测指标[2,3]。另外,CT肺动脉造影(computed tomographic pulmonary angiography,CTPA)已成为确定PTE诊断的一线检查方法,不仅可直接观察是否存在血栓及血栓位置、形态,还可量化血栓负荷[肺动脉阻塞指数(pulmonary artery obstruction index,PAOI)],并测量心血管参数,从而评估PTE严重程度[4,5]。本文研究血浆DD水平与CTPA肺动脉血栓负荷相关性。
Galle等[6]首次提出急性PTE患者DD水平(Asserachrom D-dimer)与通气/灌注(V/Q)扫描的肺灌注缺损程度相关。随后,Kucher等[7]研究表明PTE患者采用校正的Mille指数方法,血栓负荷与DD水平(法国生物梅里埃公司全自动免疫分析系统测定)呈正比。另外,Ghanima等[8]报道了采用Qanadli评分法,DD水平与CTPA的血栓负荷相关。Jeebun等[9]也通过Qanadli评分法证实DD水平与CTPA的血栓负荷和右室功能不全相关。
然而,Qanadli评分法仅仅将肺动脉阻塞程度分为完全阻塞或部分阻塞予以评分[8−10]。Mastora评分系统则对Qanadli评分法进行补充,其优势在于通过五分制法对每支肺动脉进行阻塞程度评估,进一步提供了肺动脉远端血栓的肺灌注状态。Mastora评分是最佳的肺动脉阻塞严重程度的评估方法,因为不是通过近端血管阻塞程度来推测远端血管情况。上述二者的不同之处非常重要,因为近端血管阻塞并不是影响远端血管血流的必要条件,所以,每一支中心肺动脉进行各自评分。而且,Mastora评分系统采用血流动力学“敏感”的五分制方法对每一支动脉分支进行阻塞等级评估[11−13]。
目前尚无采用Mastora评分法探讨PTE严重程度与血浆DD水平相关性的报道。本研究目的是应用Mastora评分法探索CTPA影像严重程度与血浆DD水平是否相关。
1 对象与方法
1.1 研究对象
顺次选取2009年1月至2011年8月大连医科大学附属第一医院采用CTPA首次确诊为急性PTE,并在确诊前后24h内测定血浆DD水平的患者。排除标准:明确诊断慢性血栓栓塞性肺动脉高压、既往明确静脉血栓栓塞症病史、血液系统疾病和妊娠。入选患者共69例,男性34例(49.3%),女性35例(50.7%),年龄22~85(58±15)岁。并将入选病例分为老年组(>60岁)和非老年组(≤60岁),老年组31例,男性16例,女性15例;非老年组38例,男性18例,女性20例。记录性别、年龄、基础疾病、诱发因素、发病时间(从出现PTE症状至CTPA确诊时间)、临床表现等。
1.2 血浆DD检测
应用高敏免疫比浊法测定血浆DD水平,正常人血浆DD<300μg/L。
1.3 CTPA成像
所有患者行CT胸部平扫和肺动脉增强扫描,应用GE light-speed 16排螺旋CT。扫描参数:管电压120kV,管电流260mA,准直器宽度16×0.625mm,层厚1.25mm,螺距0.938∶1,扫描范围为肺部,转数:0.6s/r。增强扫描:肘静脉以4ml/s注入碘普罗胺(优维显,碘浓度为370g/L)进行增强扫描,注射造影剂与显像的延迟时间为14s。CTPA影像阅读由至少>2名肺血管专业影像学医师进行双盲阅片。
1.4 PAOI
采用Mastora[11]评分系统量化血栓负荷(PAOI),PAOI>21.3%提示早期预后不良风险增加[12]。
1.5 右心室及左心室短轴直径比值
CTPA影像四腔心层面测定右心室(right ventricule,RV)及左心室(left ventricule,LV)短轴直径,计算两者比值(right/left ventricular short axis diameter ratio,RV/LV),RV/LV>0.9提示右心室功能不全(right ventricular dysfunction,RVD)[13,14]。
1.6 随访
3个月后随访,复查血浆DD水平和CTPA。
1.7 统计学处理
应用SPSS19.0统计软件进行统计分析。应用Spearman相关系数及检验、2检验、Mann-Whitney检验或Wilcoxon带符号秩检验。以<0.05为差异有统计学意义。
2 结 果
2.1 两组患者临床资料比较
两组患者在性别以及有无诱发因素、基础疾病、晕厥、下肢深静脉血栓形成的临床资料方面比较,差异均无统计学意义(>0.05;表1)。

表1 两组患者临床资料比较
Precipitating factors include trauma, surgery, immobility, and oestrogen use. Underlying disesases include chronic heart disease, chronic lung disease, cancer, cerebrovascular disease, varicosity, diabetes mellitus, and connective tissue disease. The diagnosis of deep vein thrombosis is confirmed by computed tomographic venography or compression ultrasound
2.2 血浆DD水平与PAOI、RV/LV的相关性
69例患者血浆DD浓度中位值为765μg/L(95%CI:752~1207μg/L),PAOI中位值为16.77%(95%CI:16.49%~23.26%)。血浆DD水平与整体肺动脉PAOI呈正相关(=0.417,=0.000;图1)。血浆DD水平与RV/LV呈正相关(=0.268,=0.027;图2A)。PAOI与RV/LV呈正相关(=0.390,=0.001;图2B)。

图1 D−二聚体与肺动脉阻塞指数的关系
Figure 1 Correlation between D-dimer and pulmonary artery obstruction index
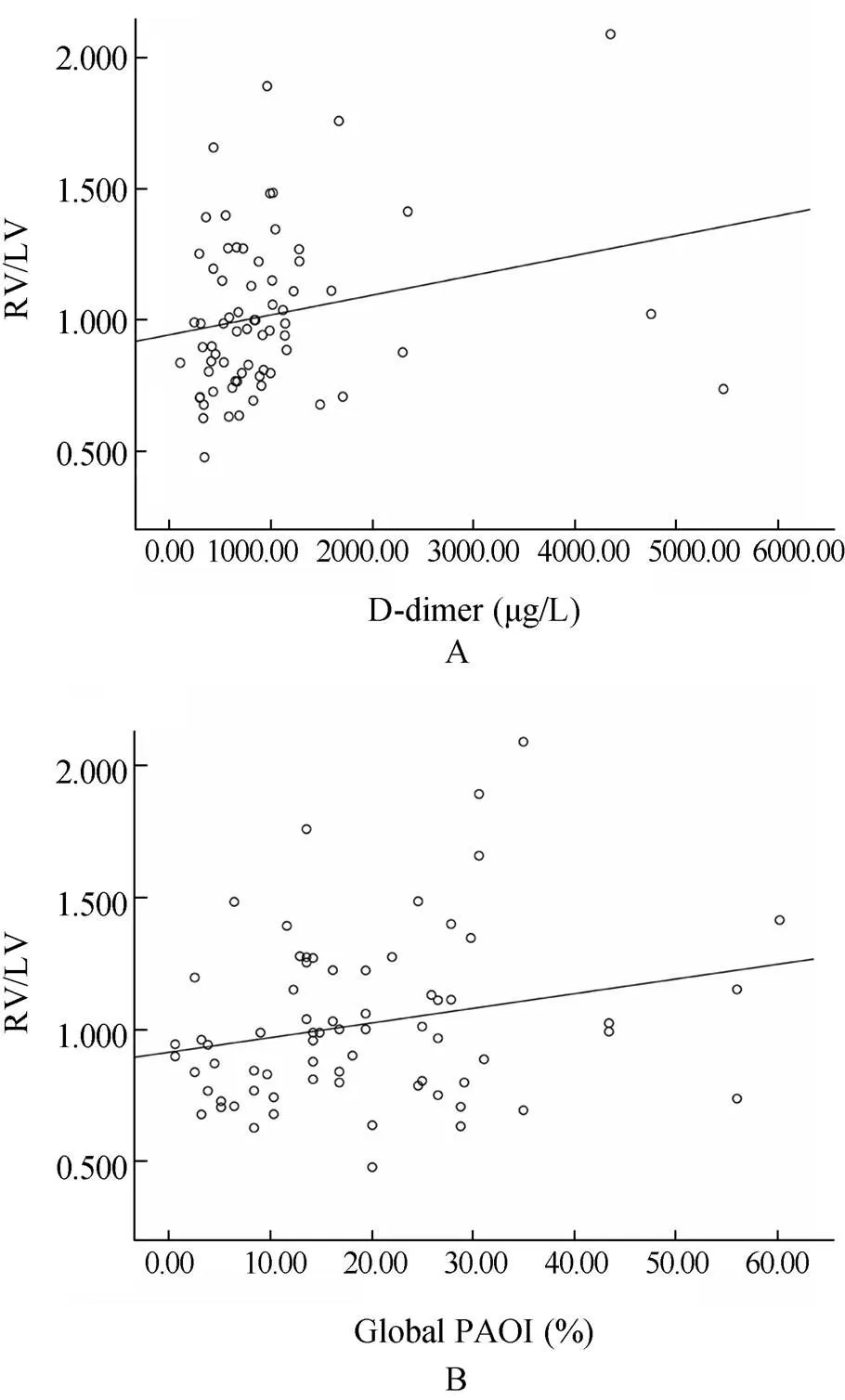
图2 右心室与左心室短轴直径比值与D−二聚体、肺动脉阻塞指数的关系
Figure 2 Correlations among RV/LV, D-dimer and PAOI RV/LV: right/left ventricular short axis diameter ratio; PAOI: pulmonary artery obstruction index. A: correlation between RV/LV and D-dimer; B: correlation between RV/LV and PAOI
PAOI>21.3%的患者29例(42.03%),其血浆DD中位值为993μg/L(95%CI:856~1841μg/L),PAOI≤21.3%患者40例(57.97%),其血浆DD中位值663μg/L(95%CI:572~846μg/L),两者差异有统计学意义(=−2.991,=0.003;图3A)。根据受试者工作特征(receiver operating characteristic,ROC)曲线可得血浆DD浓度为746μg/L时,预测PAOI>21.3%的敏感度为36.6%,特异度为28.6%(曲线下面积为0.287;图4);其中血浆DD>746μg/L的患者35例,PAOI均值为24.99%±15.65%;而DD≤746μg/L的患者34例,PAOI均值为14.29%±9.49%,两者差异有统计学意义(=3.447,=0.031)。
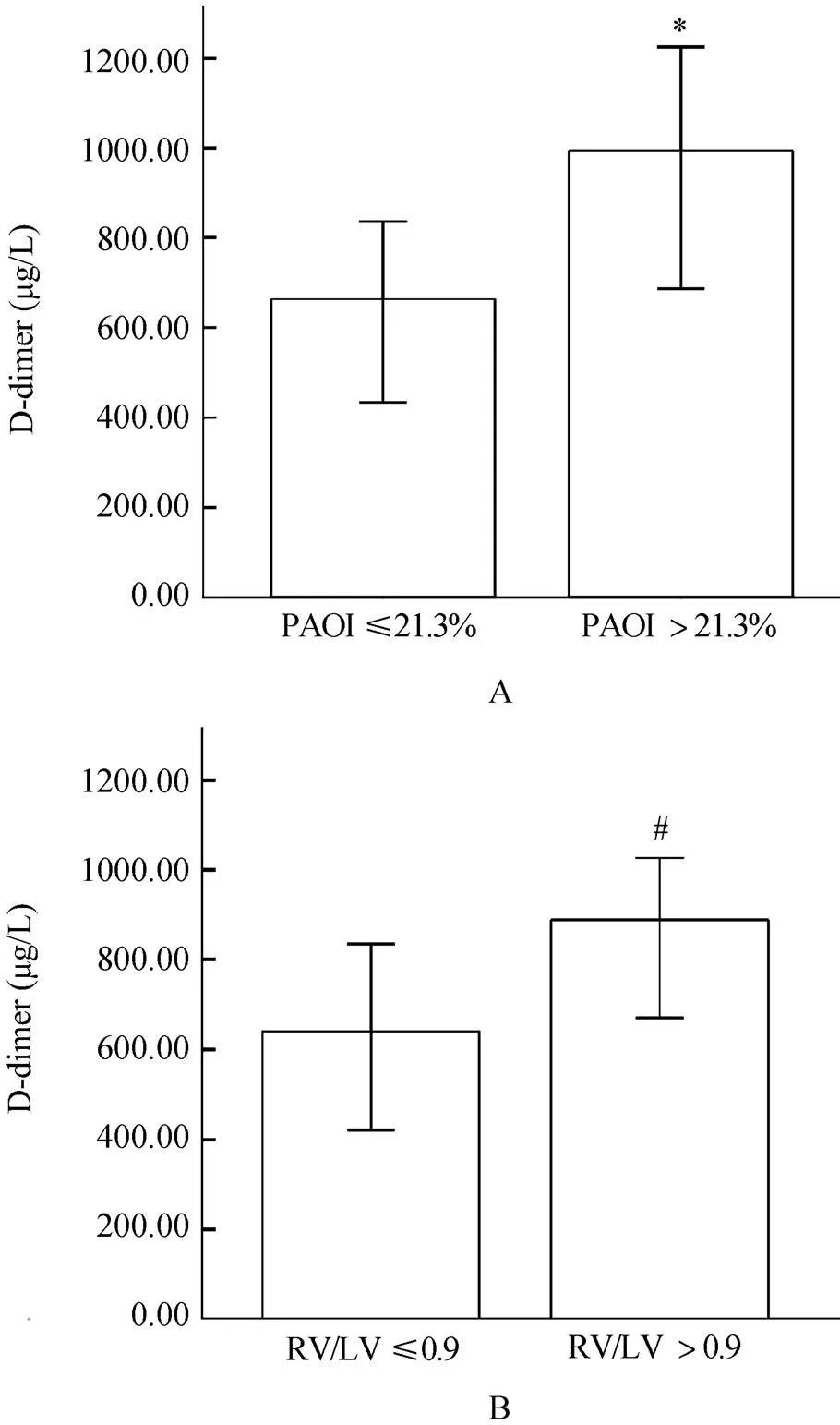
图3 不同组别患者D−二聚体浓度比较
Figure 3 Comparison of D-dimer level in different groups RV/LV: the ratio of end-diastolic right ventricular diameter to leftventricular diameter; PAOI: pulmonary artery obstruction index. A: comparison of D-dimer level between the groups with PAOI>21.3% and PAOI≤21.3%; compared with PAOI≤21.3%,*=0.003. B: comparison of D-dimer level between the groups with RV/LV>0.9 and RV/LV≤0.9; compared with RV/LV≤0.9,#=0.038
RV/LV>0.9的患者37例(53.6%),其血浆DD中位值为880μg/L(95%CI:767~1392μg/L),RV/LV≤0.9的患者32例(46.4%),其血浆DD中位值为634μg/L(95%CI:519~1211μg/L),两者差异有统计学意义(=−2.070,=0.038;图3B)。根据ROC曲线可得血浆DD浓度为721μg/L时,预测RVD的敏感度为64.9%,特异度为62.5%(曲线下面积为0.645;图5);其中血浆DD>721μg/L的患者36例,RV/LV均值为1.095±0.334,而DD≤721μg/L的患者33例,RV/LV均值为0.934±2.267,两者差异有统计学意义(=2.206,=0.001)。
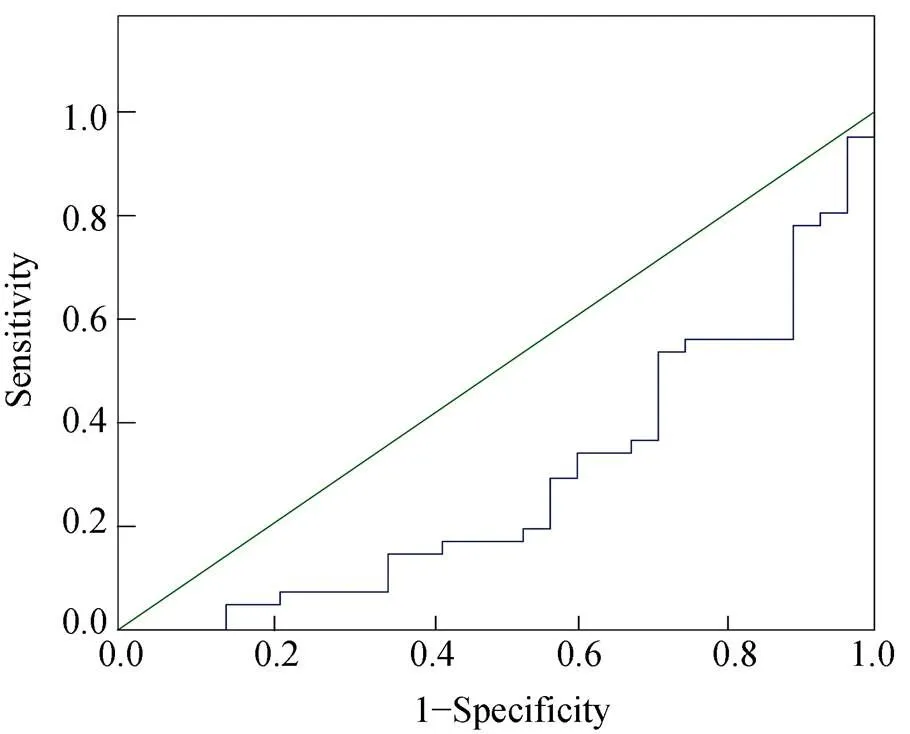
图4 D−二聚体用于预测PAOI>21.3%的ROC曲线
Figure 4 ROC curve for prediction of PAOI>21.3% by D-dimer PAOI: pulmonary artery obstruction index

图5 D−二聚体用于预测RVD的ROC曲线
Figure 5 ROC curve for prediction of RVD by D-dimer RVD: right ventricular dysfunction
2.3 血浆DD水平、PAOI与发病时间的相关性
69例患者发病时间中位数为2d(1h~15d)。血浆DD水平与发病时间之间呈负相关(=-0.407,=0.001;图6)。整体肺动脉PAOI与发病时间不存在相关性(=-0.140,=0.252;图7)。
2.4 血浆DD水平与PTE和(或)深静脉血栓(deep vein thrombosis,DVT)的关系
单纯PTE(无DVT)者18例,DD中位值611.5μg/L(95%CI:458.93~1426.62μg/L);PTE伴DVT者51例,血浆DD水平807μg/L(95%CI:726.66~1259.40μg/L),两者差异无统计学意义(=-0.806,=0.420)。
2.5 年龄与血浆DD水平、PAOI的关系
老年组和非老年组血浆DD水平中位值分别为727μg/L(95%CI:638.43~1203.23μg/L)、792.5μg/L(95%CI:670.31~1397.86μg/L),两者差异无统计学意义(=-0.180,=0.857)。两组PAOI中位值分别为14.84%(95%CI:12.79%~21.11%)、20.97%(95%CI:17.02%~27.50%),两者差异无统计学意义(=-01.382,=0.167)。
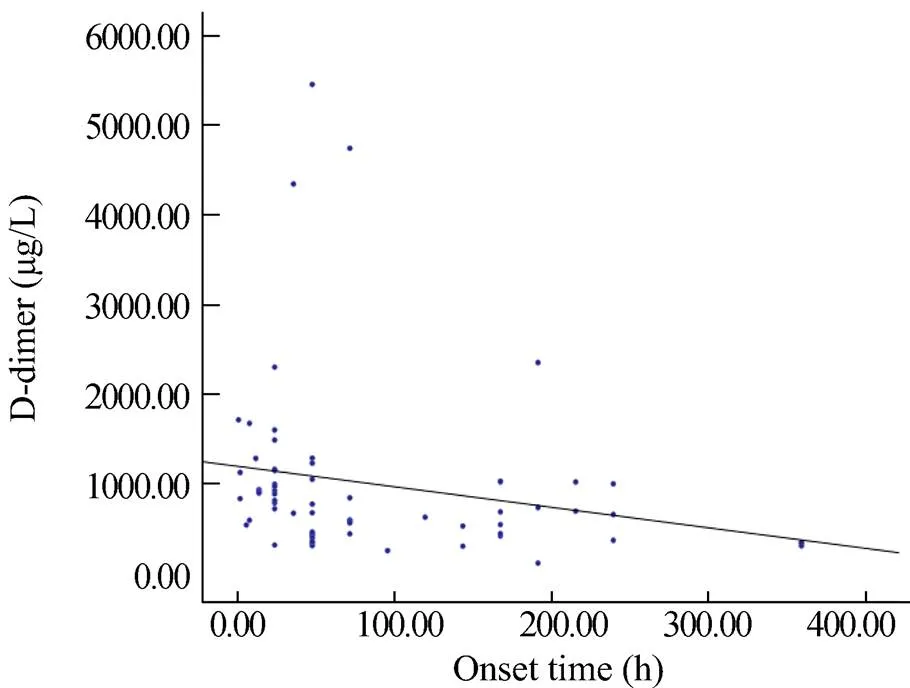
图6 D−二聚体水平与发病时间的关系
Figure 6 Correlations between D-dimer level and pulmonary thromboembolism onset time
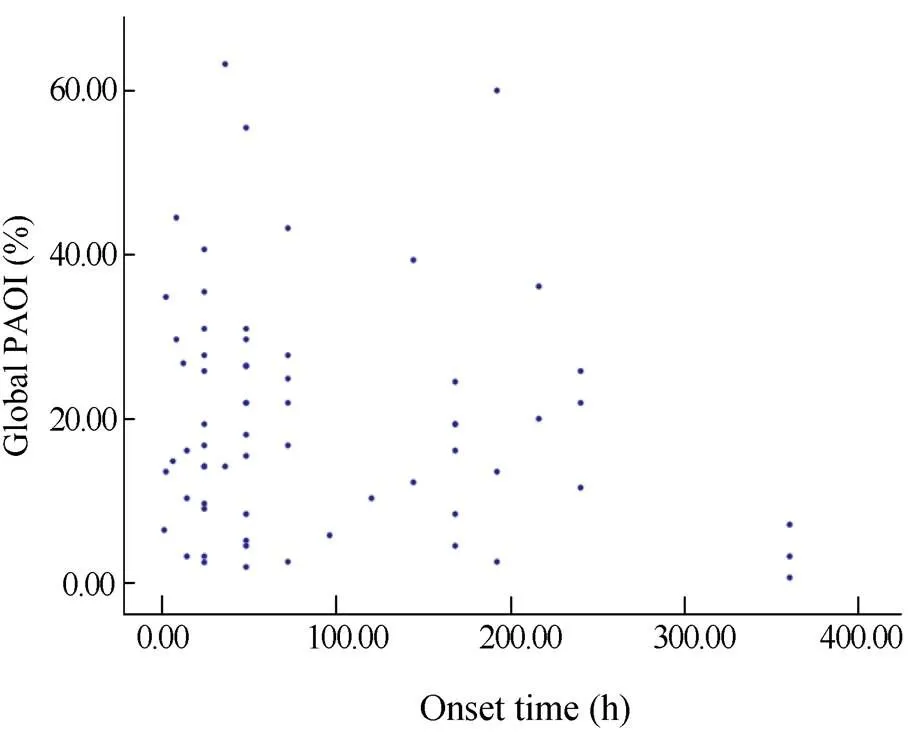
图7 PAOI与发病时间的关系
Figure 7 Correlations between PAOI and PTE onset time PAOI: pulmonary artery obstruction index; PTE: pulmonary thromboembolism
2.6 治疗和随访
69例PTE患者中,2例溶栓治疗,67例抗凝治疗。3个月后随访,其中65例(失访4例)患者规范抗凝并复查血浆DD水平和CTPA,DD水平和PAOI均显著下降(=-6.976,=0.000;=-7.009,=0.000;图8),两者具有相关性(=0.609,=0.000),其中44例患者(67.69%)复查CTPA提示血栓完全吸收,余21例患者PAOI值波动于0.65%~5.16%;血浆DD水平中位值下降至190μg/L(95%CI:179.69~238.61μg/L),恢复到正常值范围内。
3 讨 论
本研究结果证实,血浆DD水平与整体肺动脉PAOI呈正相关,表明DD水平(765μg/L)与CTPA影像所示血栓负荷(16.77%)程度呈正比,即血栓或栓子负荷越多,血浆DD水平越高,与较低血栓负荷相比,较高栓子负荷能产生较多的纤维蛋白降解产物,上述结果与Galle等[6]、Kucher等[7]、Ghanima等[8]及Jeebun等[9]研究结果相似。并且,我们创新性地同时随访CTPA和DD,结果表明,规范抗凝3个月后大部分患者(67.69%)血栓完全吸收,部分(32.31%)残留血栓患者PAOI水平也明显下降(0.65%~5.16%);而血浆DD水平中位值(190μg/L)则恢复到正常值范围内,两者仍具有相关性。因此,我们可通过定期监测DD水平评估急性PTE患者的血栓负荷,进一步指导治疗和判断预后。
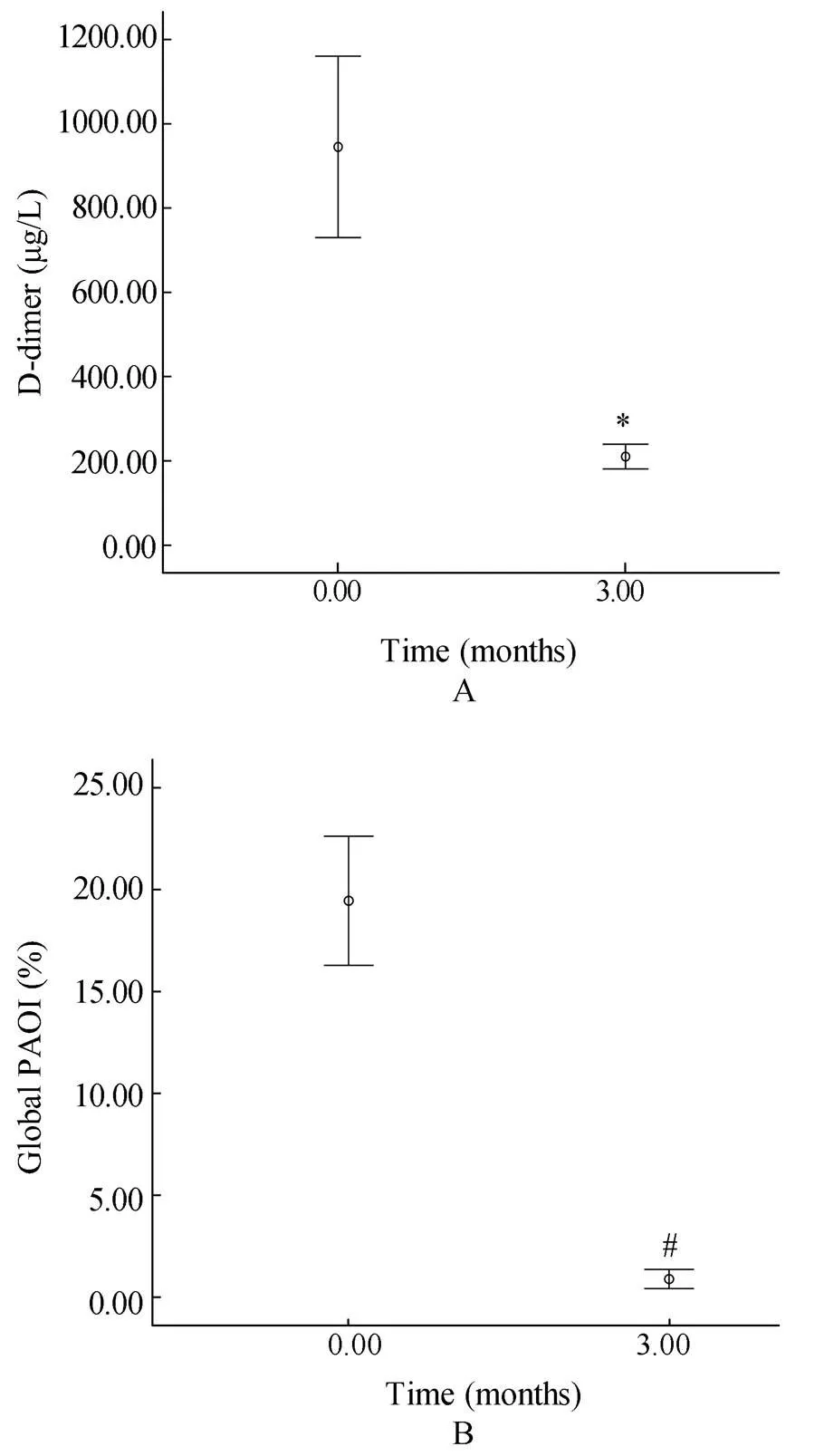
图8 治疗前后D−二聚体浓度和PAOI变化
Figure 8 Comparison of D-dimer level and PAOI before and after treatment PAOI: pulmonary artery obstruction index. A: comparison of D-dimer level before and after treatment; compared with before treatment,*=0.000. B: comparison of PAOI before and after treatment; compared with before treatment,#=0.000
Engelke等[12]研究证实,PAOI>21.3%是PTE患者早期死亡的重要预测因子,其风险可增加约6.7倍(=0.017);而PAOI≤21.3%的患者经规范抗凝后可获得较长期生存率。多项研究[13−15]证实CTPA影像提示右室功能不全(RV/LV>0.9)的PTE患者预后不良。本研究结果证实,血浆DD水平和PAOI均与RV/LV呈正相关;PAOI>21.3%的患者血浆DD中位值高于PAOI≤21.3%的患者;RV/LV>0.9的患者血浆DD中位值高于RV/LV比值≤0.9的患者。因此,我们可通过定期监测DD水平评估急性PTE患者病情严重程度和危险分层。
另外,本研究创新性地探索了DD和PAOI水平与发病时间的相关性。结果证实,血浆DD水平与发病时间之间呈负相关;而整体肺动脉床的PAOI与发病时间不存在相关性。从而进一步表明,血浆DD水平是与“新鲜”血栓负荷呈正相关的。
近年来,多项回顾性研究[16−19]证实DD的阈值与年龄相关,建议使用年龄校正的DD阈值,即年龄>50岁患者,DD阈值为年龄×10μg/L(包括Vidas®、Tinaquant®、HemosIL-DD®,Liatest®和MDA®等检测方法),然而,对于明确诊断PTE的患者,年龄与DD和PAOI的关系尚未得到关注,本研究创新性地对比研究老年组(>60岁)和非老年组(≤60岁)DD和PAOI水平,结果表明二者在两组患者中差异均无统计学意义。
4 结 论
DD水平与CTPA肺动脉新鲜血栓负荷和RV/LV呈正相关,因其检测方法的简便性、可重复性和应用普遍性,有助于急性PTE患者的临床评估病情、指导治疗和判断预后。老年与非老年急性PTE患者的DD和PAOI水平差异无统计学意义。
[1] Bĕlohlávek J, Dytrych V, Linhart A. Pulmonary embolism. Part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism[J]. Exp Clin Cardiol, 2013, 18(2): 129−138.
[2] Klok FA, Djurabi RK, Nijkeuter M,. High D-dimer level is associated with increased 15-d and 3 months mortality through a more central localization of pulmonary emboli and serious comorbidity[J]. Br J Haematol, 2008, 140(2): 218−222.
[3] Grau E, Tenías JM, Soto MJ,. D-dimer levels correlate with mortality in patients with acute pulmonary embolism: findings from the RIETE registry[J]. Crit Care Med, 2007, 35(8): 1937−1941.
[4] Nural MS, Elmali M, Findik S,. Computed tomographic pulmonary angiography in the assessment of severity of acute pulmonary embolism and right ventricular dysfunction[J]. Acta Radiol, 2009, 50(6): 629−637.
[5] van der Meer RW, Pattynama PM, van Strijen MJ,. Right ventricular dysfunction and pulmonary obstruction index at helical CT: prediction of clinical outcome during 3-month follow-up in patients with acute pulmonary embolism[J]. Radiology, 2005, 235(3): 798−803.
[6] Galle C, Papazyan JP, Miron MJ,. Prediction of pulmonary embolism extent by clinical findings, D-dimer level and deep vein thrombosis shown by ultrasound[J]. Thromb Haemost, 2001, 86(5): 1156−1160.
[7] Kucher N, Schroeder V, Kohler HP. Role of blood coagulation factorⅩⅢ in patients with acute pulmonary embolism. Correlation of factor ⅩⅢ antigen levels with pulmonary occlusion rate, fibrinogen, D-dimer, and clot firmness[J]. Thromb Haemost, 2003, 90(3): 434−438.
[8] Ghanima W, Abdelnoor M, Holmen LO,. D-dimer level is associated with the extent of pulmonary embolism[J]. Thromb Res, 2007, 120(2): 281−288.
[9] Jeebun V, Doe SJ, Singh L,. Are clinical parameters and biomarkers predictive of severity of acute pulmonary emboli on CTPA[J]? Q J Med, 2010, 103(2): 91−97.
[10] Qanadli SD, El Hajjam M, Vieillard-Baron A,. New CT index to quantify arterial obstruction in pulmonary embolism: comparison with angiographic index and echocardiography[J]. Am J Roentgenol, 2001, 176(6): 1415−1420.
[11] Mastora I, Remy-Jardin M, Masson P,. Severity of acute pulmonary embolism: evaluation of a new spiral CT angiographic score in correlation with echocardiographic data[J]. Eur Radiol, 2003, 13(1): 29−35.
[12] Engelke C, Rummeny EJ, Marten K. Acute pulmonary embolism on MDCT of the chest: prediction of cor pulmonale and short-term patient survival from morphologic embolus burden[J]. Am J Roentgenol, 2006, 186(5): 1265−1271.
[13] Quiroz R, Kucher N, Schoepf UJ,. Right ventricular enlargement on chest computed tomography: prognostic role in acute pulmonary embolism[J]. Circulation, 2004, 109(20): 2401−2404.
[14] Torbicki A, Perrier A, Konstantinides S,. Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2008, 29(18): 2276−2315.
[15] Konstantinides SV, Torbicki A, Agnelli G,. 2014 ESC Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism. Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2014, 35(43): 3033−3069.
[16] Harper PL, Theakston E, Ahmed J,. D-dimer concentration increases with age reducing the clinical value of the D-dimer assay in the elderly[J]. Intern Med J, 2007, 37(9): 607−613.
[17] Douma RA, Le GG, Sohne M,. Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts[J]. BMJ, 2010, 340: c1475.
[18] Douma RA, Tan M, Schutgens RE,. Using an age-dependent D-dimer cut-off value increases the number of older patients in whom deep vein thrombosis can be safely excluded[J]. Haematologica, 2012, 97(10): 1507−1513.
[19] Schouten HJ, Koek HL, Oudega R,. Validation of two age dependent D-dimer cut-off values for exclusion of deep vein thrombosis in suspected elderly patients in primary care: retrospective, cross sectional, diagnostic analysis[J]. BMJ, 2012, 344: e2985.
(编辑: 周宇红)
Correlation of D-dimer level with clot burden of pulmonary embolism: report of 69 cases
FANG Chun-Xiao1, AN Jun1, JI Ying-Qun1*, SUN Bo2, LI Zhi-Yong2, ZHANG Zhong-He1
(1Department of Respiratory Diseases,2Department of Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian 116011, China)
To determine the correlation of plasma level of D-dimer (DD) with clot burden of pulmonary embolism.A prospective study was performed on 69 consecutive patients with acute pulmonary thromboembolism (PTE) confirmed by computed tomographic pulmonary angiography (CTPA) in our hospital from January 2009 to August 2011. A pulmonary artery obstruction index (PAOI, Mastora score) >21.3% indicated severe obstruction of PTE. A right ventricle/left ventricle (RV/LV) >0.9 indicated RV dysfunction. The plasma level of DD was determined by immunoturbidimetric assay.The median DD level was 765µg/L (95%CI: 750−1 205µg/L) and that of PAOI was 16.77% (95%CI: 16.32%−23.06%). Plasma DD level was positively correlated with PAOI (=0.417,=0.000). The patients with PAOI >21.3% had significantly higher DD levels than those with PAOI ≤21.3% (993663µg/L,=-2.991,=0.003). DD level was positively correlated with RV/LV (=0.272,=0.024). The patients with RV/LV >0.9 had obviously higher DD levels than those with RV/LV ≤0.9 (880634µg/L,=-2.070,=0.038). There was a positive correlation between PAOI and RV/LV (=0.390,=0.001). Negative correlation was found in the PTE onset time with DD level (=-0.407,=0.000), but not with PAOI (=-0.140,=0.245). There was no significant difference in the DD level and PAOI between the elderly patients (>60 years old) and those younger (≤60 years old) (727.0792.5µg/L,=-0.180,=0.857; 14.84%20.97%,=-1.382,=0.167). After 3 months’ standard anticoagulant therapy, both DD level and PAOI were decreased in the cohort (=-6.976,=0.000;=-7.009,=0.000), and their decreases were correlated (=0.609,=0.000).DD level is positively correlated with CTPA clot burden and RV/LV respectively, and is helpful in illness assessment, management guidance and prognostic evaluation for the acute PTE patients. There is no significant difference in DD level and PAOI between the patients older and less than 60 years.
D-dimer; pulmonary embolism; pulmonary artery obstruction index; computed tomographic pulmonary angiography
(2011BAI11B17).
R563.5
A
10.11915/j.issn.1671-5403.2015.12.206
2015−09−21;
2015−10−23
国家“十二五”科技支撑计划课题(2011BAI11B17)
季颖群, E-mail: jiyingqun@163.com
