“Shamrock method”超声引导连续腰丛神经阻滞用于老年患者全膝关节置换术后镇痛的临床观察
2015-04-21公茂伟孙永海
公茂伟,孙永海,傅 强
“Shamrock method”超声引导连续腰丛神经阻滞用于老年患者全膝关节置换术后镇痛的临床观察
公茂伟,孙永海*,傅 强
(解放军总医院麻醉手术中心,北京 100853)
评价“Shamrock method”超声引导联合刺激仪定位下连续腰丛神经阻滞与连续股神经阻滞对全膝关节置换术后镇痛的临床效果。采用开放、随机对照的研究方法,选择解放军总医院2014年6月至2014年12月择期行单侧全膝关节置换术的老年患者80例,年龄65~87岁,美国麻醉医师协会(ASA)分级Ⅱ~Ⅲ级,随机均分为连续腰丛神经阻滞组(L组)和连续股神经阻滞组(F组)。L组患者采用“Shamrock method”超声引导联合刺激仪定位下行腰丛神经阻滞,F组则采用超声引导联合刺激仪定位下行股神经阻滞,两组穿刺成功后均注入0.2%罗哌卡因30ml并留置导管,术后镇痛泵背景剂量为0.2%罗哌卡因5ml/h。记录术后6,12,24,48h时静息状态视觉模拟评分法(VAS)评分,术后24,48h膝关节功能锻炼时VAS评分和肌力评分;记录术后局麻药中毒、恶心呕吐和神经损伤等不良反应的发生情况。与L组相比较,F组术后各时点静息状态和功能锻炼VAS评分均明显增高(<0.05),肌力评分两组间差异无统计学意义(>0.05)。两组均未见局麻药中毒、神经损伤发生,且恶心呕吐等不良反应发生率两组间差异无统计学意义。“Shamrock method”超声引导联合刺激仪定位下连续腰丛神经阻滞对于老年患者全膝关节置换术后镇痛的临床效果优于连续股神经阻滞。
shamrock method;超声;腰骶丛;自主神经传导阻滞;股神经;老年人;关节成形术,置换,膝;术后镇痛
随着人口老龄化的日益严重,关节退行性疾病日益增多。人工全膝关节置换术(total knee arthoplasty,TKA)是治疗膝关节严重疾患、重建膝关节功能的主要手段,但创伤较大,常常导致术后严重的疼痛[1]。超声引导连续股神经阻滞术后镇痛广泛应用于临床,但因闭孔神经阻滞不全,往往难以达到满意的镇痛效果。“Shamrock method”[2,3]是一种新式超声引导下以平面内进针方式的腰丛神经阻滞方法,超声引导定位较神经刺激仪定位有较为明显的优势,在超声引导下可直接观察到针头与神经以及周围血管组织的关系,提高了阻滞的成功率,从而减少了肾脏、神经损伤等并发症的发生。本研究通过比较“Shamrock method”超声引导联合刺激仪定位下连续腰丛神经阻滞和超声引导连续股神经阻滞,观察前者用于老年患者TKA术后镇痛的可行性及临床效果。
1 对象与方法
1.1 研究对象
选择解放军总医院2014年6月至2014年12月美国麻醉医师协会(American Society of Anesthesiologists,ASA)分级Ⅱ~Ⅲ级行TKA患者80例,年龄65~87岁,体质量45~98kg,男36例,女44例。既往无局麻药物过敏史和阿片类药物成瘾史,无外周神经病变及凝血功能障碍等。采用开放、随机对照的研究方法,随机分为连续腰丛神经阻滞组(L组)和连续股神经阻滞组(F组),每组40例。
1.2 麻醉方法
两组入手术室后均开放静脉通道,采用多功能监测仪常规监测无创血压(noninvasive blood pressure,NBP)、心率(heart rate,HR)、心电图(electrocardiogram,ECG)及脉搏血氧饱和度(pulse oxygen saturation,SPO2)。
术前30min行神经阻滞,麻醉前均静脉注射咪达唑仑(咪唑安定,midazolam)1~2mg、芬太尼(fentanyl)50μg。L组患者采用“Shamrock method”超声引导联合刺激仪定位下连续腰丛神经阻滞(图1)。患者取侧卧位,患侧在上,两下肢自然伸展略弯曲,以脊柱棘突连线为正中线,过髂嵴最高点作上述直线的垂线,自两直线交点向阻滞侧旁开4~5cm即为穿刺点[4]。确定穿刺点后,应用超声(美国SonoSite公司)低频线阵探头(频率为2~5MHz)横向置于腹外侧腋中线,紧贴髂嵴高点,穿刺针以平面内(in-plane)模式进针,进针方向垂直于皮肤或稍朝向中线。F组应用超声引导联合刺激仪定位下行股神经阻滞,在腹股沟韧带下方2cm处水平放置高频线阵探头(频率为7~13MHz),长轴与大腿纵轴垂直,待清晰显示髂耻弓筋膜处由内向外排列的股静脉、股动脉和股神经横断面超声图像,采用平面内技术,由大腿外侧皮肤进针。两组同时联合使用神经刺激器(Stimuplex Dig型,德国贝朗公司)辅助定位,设定刺激波宽0.1ms,频率2Hz,电流强度为1mA,出现股四头肌收缩伴髌骨跳动时,减小刺激强度,同时调整穿刺针位置,当电流减小至0.3~0.4mA时,仍有肌群抽搐,回抽无血即可注药1ml后肌肉颤搐即消失,调大刺激强度至1mA,无肌肉收缩可继续注入局部麻醉药0.2%罗哌卡因(ropivacaine)30ml,并留置导管,置管长度均为超出针尖后5cm。
所有患者于神经阻滞实施后置入喉罩,静脉靶控输注丙泊酚(异丙酚,propofol)2.5~3.0mg/L,芬太尼50~100μg和顺苯磺酸阿曲库铵(atracurium besilate)0.1~0.2mg/kg,置入一次性Supreme喉罩(德国LMA公司)。术中吸入0.6%~1.0%七氟烷(七氟醚,sevoflurane),静脉靶控输注丙泊酚0.8~1.8mg/L,瑞芬太尼(remifentanil)0.1~0.2μg/(kg·h)维持麻醉,维持呼气末二氧化碳分压(end-tidal carbon dioxide,ETCO2)35~40mmHg(1mmHg=0.133kPa)。术毕患者完全清醒后拔除喉罩。手术结束前两组患者均接一次性术后镇痛泵,背景剂量0.2%罗哌卡因5ml/h,保留镇痛48h。任一时间点若患者的视觉模拟评分法(Visual Analogue Scale,VAS)评分>4分,则加用帕瑞昔布钠(parecoxib sodium)40mg静脉注射。
1.3 观察指标
1.3.1 疼痛评分 疼痛强度采用VAS进行评分,分值为0~10,0代表无痛,10代表难以忍受的疼痛。记录术后6,12,24,48h时静息状态VAS评分(Rest VAS,RVAS),术后24,48h膝关节功能锻炼时VAS评分(Functional Exercise VAS,FVAS)。
1.3.2 肌力评分 记录各时间点患肢股四头肌肌力,0分为完全瘫痪,1分为可收缩,2分为不能抗重力,3分为抗重力不抗阻力,4分为可抗弱阻力,5分为正常。
1.3.3 不良反应 包括术后局部麻醉药中毒症状、恶心呕吐、神经损伤等情况。
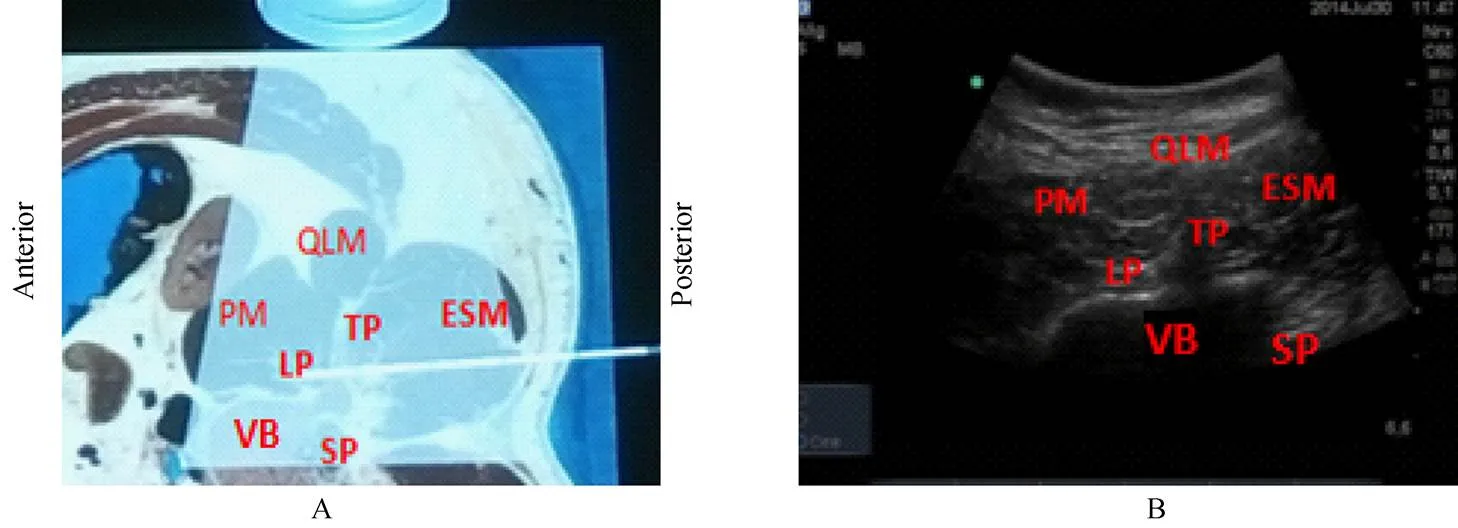
图1 腰丛“Shamrock method”入路
Figure 1 Shamrock method ultrasound-guided lumbar plexus blocks
ESM: erector spinae muscles; LP: lumbar plexus; PM: psoas major muscle; QLM: quadratus lumborum muscle; SP: spinous process; TP: transverse process; VB: vertebral body. A: diagrammatic drawing, white arrow is puncture needle; B: ultrasound images
1.4 统计学处理
2 结 果
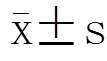
两组患者性别、年龄、体质量一般情况差异无统计学意义(>0.05;表1)。术后6,12,24,48h RVAS评分(表2)和术后24h、48h FVAS评分(表3)L组明显低于F组(<0.05);术后24和48h肌力评分L组分别为(2.6±0.5)分和(4.2±0.3)分,F组分别为(2.7±0.4)分和(4.3±0.4)分,两组间差异无统计学意义(>0.05)。术后24h功能锻炼时,两组均有加用帕瑞昔布钠病例(L组2例,F组5例)。两组均无局部麻醉药中毒、神经损伤发生,且恶心呕吐等不良反应发生率两组间差异无统计学意义。
3 讨 论
TKA常伴随骨质、骨膜等组织的损伤以及术中止血带的使用造成血管的缺血再灌注损伤,因此术后患者早期会经历剧烈疼痛[5,6]。TKA术后完善的镇痛利于患者早期行康复训练,从而防止术后黏连、缩短术后恢复时间、减少心血管及肺部并发症发生[7]。本研究应用“Shamrock method”超声引导联合刺激仪定位下连续腰丛阻滞用于老年患者TKA术后,取得满意的镇痛效果。“Shamrock method”[2]在超声引导下可以直接观察到针头与神经以及周围血管组织的关系,并且可以看到注射药物后局部扩散的整个动态过程,不仅缩短了操作时间、加快了神经阻滞,而且增加了阻滞的成功率。联合应用超声和刺激器进行神经穿刺使操作更简便、有效和安全[8],使得穿刺定位更精确,确保药液准确注射在其周围。从而减少了肾脏、神经的损伤等并发症的发生。
表1 两组患者基本情况比较
L group: continuous lumbar plexus nerve blocks group; F group: continuous femoral nerve blocks group

表2 两组患者静息时术后不同时间点VAS评分
L group: continuous lumbar plexus nerve blocks group; F group: continuous femoral nerve blocks group; RVAS: Rest Visual Analogue scale; TKA: total knee arthoplasty. Compared with L group,*<0.05

表3 两组患者功能锻炼时术后不同时间点VAS评分
L group: continuous lumbar plexus nerve blocks group; F group: continuous femoral nerve blocks group; FVAS: Functional Exercise Visual Analogue Scale; TKA: total knee arthoplasty. Compared with L group,*<0.05
静脉镇痛操作简便、不影响肌力、适用范围广,但阿片类药物有较严重的呼吸抑制、恶心呕吐、尿潴留和瘙痒等不良反应。硬膜外术后镇痛效果较为满意,但关节置换术后常使用的低分子肝素等抗凝剂预防术后深静脉血栓,有形成椎管内血肿的风险,限制了其临床使用[9]。
Singelyn等[10]报道有效的外周神经阻滞能缓解疼痛、减少吗啡类药物的应用。并且外周神经阻滞还具有对患者血流动力学影响小的特点,尤其适用于老年合并心血管疾病的患者[11]。国内TKA术后多采用连续股神经阻滞镇痛,股神经阻滞基本只能抑制膝关节前方的伤害性刺激传导,对TKA术后静息状态和功能锻炼引起的疼痛均不能完全阻断[12]。Macalou等[13]的研究表明,股神经阻滞联合闭孔神经阻滞的镇痛效果较单纯股神经阻滞显著提高,说明闭孔神经阻滞不全是导致术后疼痛的主要原因之一,大腿下1/3段内侧区被认为是闭孔神经支配区域。本研究应用“Shamrock method”超声引导联合刺激仪定位下连续腰丛神经阻滞用于老年患者TKA,结果为L组术后各时点RVAS和FVAS均明显低于F组(<0.05),表明腰丛神经阻滞对闭孔神经作用相对完善,从而明显提高了镇痛效果。
完善的腰丛神经阻滞需要局麻药量较大,局麻药通过周围及中枢两条途径预防和减少疼痛,缓解由股四头肌痉挛所致的功能障碍。罗哌卡因是一种新的酰胺类局部麻醉药,其作用强度和药代动力学与布比卡因类似,但它的心脏毒性较低,使用低浓度、小剂量时几乎只阻滞感觉神经[14],相关研究证实0.2%罗哌卡因用于连续神经阻滞能有效减轻痛觉而不抑制运动纤维[15],可达到最佳的镇痛和最小的运动阻滞平衡[16]。本观察中应用0.2%罗哌卡因取得较满意的镇痛效果。
综上所述,本研究认为“Shamrock method”超声引导联合刺激仪定位下连续腰丛神经阻滞用于老年患者TKA术后镇痛,效果优于连续股神经阻滞,并且增加了阻滞的成功率及安全性,此种方法应用于临床具有可行性。
[1] Jia DL, Li SQ, Han Bin,. Analgesic efficacy of stimulating catheter for continuously postoperative femoral nerve block[J]. J Clin Anesthesiol, 2011, 27(3): 257−260. [贾东林, 李水清, 韩 彬, 等. 刺激型导管连续股神经阻滞术后镇痛效果观察[J]. 临床麻醉学杂志, 2011, 27(3): 257−260.]
[2] Lin JA, Lee YJ, Lu HT. Finding the bulging edge: a modified shamrock lumbar plexus block in average-weight patients[J]. Br J Anaesth, 2014, 113(4): 718−720.
[3] Lin JA, Lu HT. Solution to the challenging part of the shamrock method during lumbar plexus block[J]. Br J Anaesth, 2014, 113(3): 516−517.
[4] Grant SA, Breslin DS, Macleod DB,. Variability in determination of point of needle insertion in peripheral nerve blocks: a comparison of experienced and inexperienced anaesthetists [J]. Anaethesia, 2003, 58(7): 688−692.
[5] Dorr LD, Chao L. The emotional state of the patient after total hip and knee arthroplasty[J]. Clin Orthop Relat Res, 2007, 463: 7−12.
[6] Salinas FV, Liu SS, Mulroy MF. The effect of single-injection femoral nerve blockcontinuous femoral nerve block after total knee arthroplasty on hospital length of stay and longterm functional recovery within an established clinical pathway [J]. Anesth Analg, 2006, 102(4): 1234−1239.
[7] Wang XD, Lin HH. Analgesic effect of continuous femoral nerve block in postoperative analgesia undergoing total knee arthroplasty[J]. Shandong Med J, 2007, 47(21): 91−92. [王晓东, 林惠华. 连续股神经阻滞用于全膝关节置换术后镇痛效果观察[J]. 山东医药, 2007, 47(21): 91−92.]
[8] Abrahams MS, Aziz MF, Fu RF,. Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: a systematic review and meta-analysis of randomized controlled trials[J]. Br J Anaesth, 2009, 102(3): 408−417.
[9] Guan ZP, Lyu HS, Wu C,. Early diagnosis and treatment of pulmonary embolism after total joint replacement: report of five cases [J]. Chin J Surg, 2003, 41(1): 37−40. [关振鹏, 吕厚山, 吴 淳, 等. 人工关节置换术后肺栓塞的早期诊断和处理[J]. 中华外科杂志, 2003, 41(1): 37−40.]
[10] Singelyn FJ, Deyaert M, Joris D,. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty[J]. Anesth Analg, 1998, 87(1): 88−92.
[11] Murray JM, Derbyshire S, Shields MO. Lower limb blocks[J]. Anaesthesia, 2010, 65(Suppl 1): 57−66.
[12] Capdevila X, Macaire P, Dadure C,. Continuous psoas compartment block for postoperative analgesia after total hip arthroplasty: new landmarks, technical guidelines, and clinical evalution[J]. Anesth Analg, 2002, 94(6): 1606−1613.
[13] Macalou D, Trueck S, Meuret P,. Postoperative analgesia after total knee replacement: the effect of an obturator nerve block added to the femoral 3-in-1 nerve block[J]. Anesth Analg, 2004, 99(1): 251−254.
[14] Wu ZD. Surgery[M]. Beijing: People’s Medical Publishing House, 2008: 85−86. [吴在德. 外科学[M]. 北京: 人民卫生出版社, 2008: 85−86.]
[15] Brodner G, Buerkle H, Van Aken H,. Postoperative analgesia after knee surgery: a comparison of three different concentrations of ropivacaine for centrations of ropivacaine for continuous femoral nerve blockade[J]. Anesth Analg, 2007, 105(1): 256−262.
[16] Smet I, Vlaminck E, Vercauteren M. Randomized controlled trial of patient-controlled epidural analgesia after orthopaedic surgery with sufentanil and ropivacaine 0.165% or levobupivacaine 0.125%[J]. Br J Anaesth, 2008, 100(1): 99−103.
(编辑: 周宇红)
Efficiency of ultrasound-guided “Shamrock” continuous lumbar plexus block for postoperative analgesia in the elderly after total knee arthroplasty
GONG Mao-Wei, SUN Yong-Hai*, FU Qiang
(Anesthesia and Operation Center, Chinese PLA General Hospital, Beijing 100853, China)
To evaluate the efficacy of the “Shamrock method”, ultrasound combined with stimulator guided continuous lumbar plexus nerve block for postoperative analgesia in the elderly after total knee arthroplasty by compared with continuous femoral nerve block.An open, randomized, controlled trial was conducted on 80 ASA Ⅱ or Ⅲ patients (65 to 87 years old) undergoing total knee arthroplasty in our hospital from June to December 2014. The patients were randomly assigned to continuous lumbar plexus nerve block group (L group) and continuous femoral nerve block group (F group). The patients of the former group received continuous lumbar plexus nerve block by ultrasound guided “shamrock” and electronic nerve stimulator, and those of the latter group received continuous femoral nerve block by ultrasound guiding combined with stimulator. After the nerve block catheters were inserted and 30ml 0.2% ropivacaine was given, all patients received patient-controlled analgesia (PCA) after the surgery with 0.2% ropivacaine 5ml/h as the background dose. Visual Analogue Scale (VAS) was employed to evaluate the pain level at 6, 12, 24 and 48h, postoperatively. VAS pain scores were recorded at 24 and 48h, postoperatively, during functional excise and muscle strength. The toxic reaction, nausea and vomiting, and nerve damage were recorded after surgery.The VAS scores during rest and functional excise were significantly higher in F group than in L group (<0.05), but there was no difference in the muscle strength between the 2 groups (>0.05). No local anesthetic toxicityor nerve damage was founded in the both groups, and there was no statistical difference in the incidence of side effect such as nausea and vomiting during postoperative analgesia.The ultrasound-guided “shamrock” combined with stimulator for continuous lumbar plexus nerve block is superior to continuous femoral nerve block in analgesia for postoperative analgesia in the elderly after total knee arthroplasty.
shamrock method; ultrasound; lumbosacral plexus; autonomic nerve blocks; femoral nerve; aged; arthroplasty, replacement, knee; postoperative analgesia
R592; R614.4
A
10.11915/j.issn.1671-5403.2015.06.095
2015−03−20;
2015−05−10
孙永海,E-mail:sunyonghai68@aliyun.com
