Basal Cell Carcinoma Excision Guided by Dermoscopy: A Retrospective Study in Macau
2023-10-20RicardoCoelhoandSiLeongCheong
Ricardo Coelho* and Si Leong Cheong
Department of Dermatology, Centro Hospitalar Conde de São Januário, Macau SAR 999078, China.
Abstract
Keywords: basal cell carcinoma, dermoscopy, surgery
Introduction
Worldwide, basal cell carcinoma (BCC) is the most common form of skin cancer, and the most frequently occurring malignancy in western countries.Although the incidence of BCC in Asia is lower when compared with the west,the absolute numbers are significant in large populated cities, with consistently increasing disease rates.1-2
Dermoscopy is a well-established diagnostic tool that increases BCC detection sensitivity and specificity, thereby decreasing unnecessary biopsies.Several studies, including those in Chinese patients have demonstrated the utility of this technique.3-5BCC-related criteria include arborizing vessels, leaf-like areas, blue-grey globules/blue-grey ovoid nests, spoke-wheel areas, and ulceration or multiple small erosions.6-7
Apart from its role in cancer diagnosis, several studies have demonstrated the utility of dermoscopic evaluation for peripheral extension in BCC, to accurately detect lateral borders before surgical excision.8-10Since 2016,patients with BCC proposed for surgical excision at our Department, have been submitted for dermoscopic evaluation of tumor margins before surgical excision.
The purpose of this retrospective study was to establish the usefulness of dermoscopically detecting BCC tumor margins before surgical excision, and to comprehensively evaluate our experience with this technique.
Materials and methods
This retrospective study evaluated all BCC cases selected for surgical excision between 2016 and 2018 in Centro Hospitalar Conde de São Januário.Morphea-form BCC were excluded.
For all BCC analyses, peripheral clinical borders were detected with the naked eye, and provisional excision margins were marked using a dermographic pencil,2-4 mm from clinical borders, according to location and tumor type.BCC peripheral borders were subsequently evaluated, confirmed, and adjusted if needed with a polarised-light dermoscope (DermLite® DL3, 3Gen,LLC, Dana Point, CA, USA).Finally, definitive excision margins were traced and marked for excision (Fig.1).
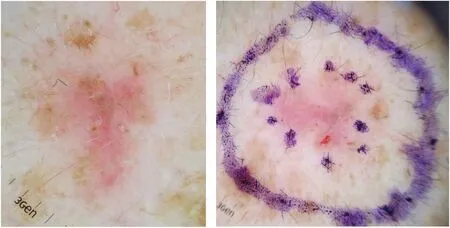
Figure 1.Basal cell carcinoma - excision margins evaluated by dermoscopy (A) and marked for excision (B).
All surgically excised BCC samples were submitted for whole specimen histological examination.The study was approved by Ethics committee of Centro Hospitalar Conde de São Januário (Approval ID: 03/CHCSJHMEC-C-0013-20114), and was performed in adherence to the Helsinki declaration.Informed consent was obtained from all patients before surgery.
Statistical analysis
Descriptive statistical analysis was carried out by using frequencies and percentages.
Results
In total, 60 tumors from 54 patients were included in this study.The median age of participants was 66.7 years;34 patients were male and 20 were female.We treated 39 Caucasians, 14 Chinese, and 7 mixed ethnicity patients.Most tumors were located on the head and face (Table 1).The histological subtype of excised BCC was nodular in 54 cases and superficial in 6; 17 tumors were pigmented and 43 were non-pigmented.
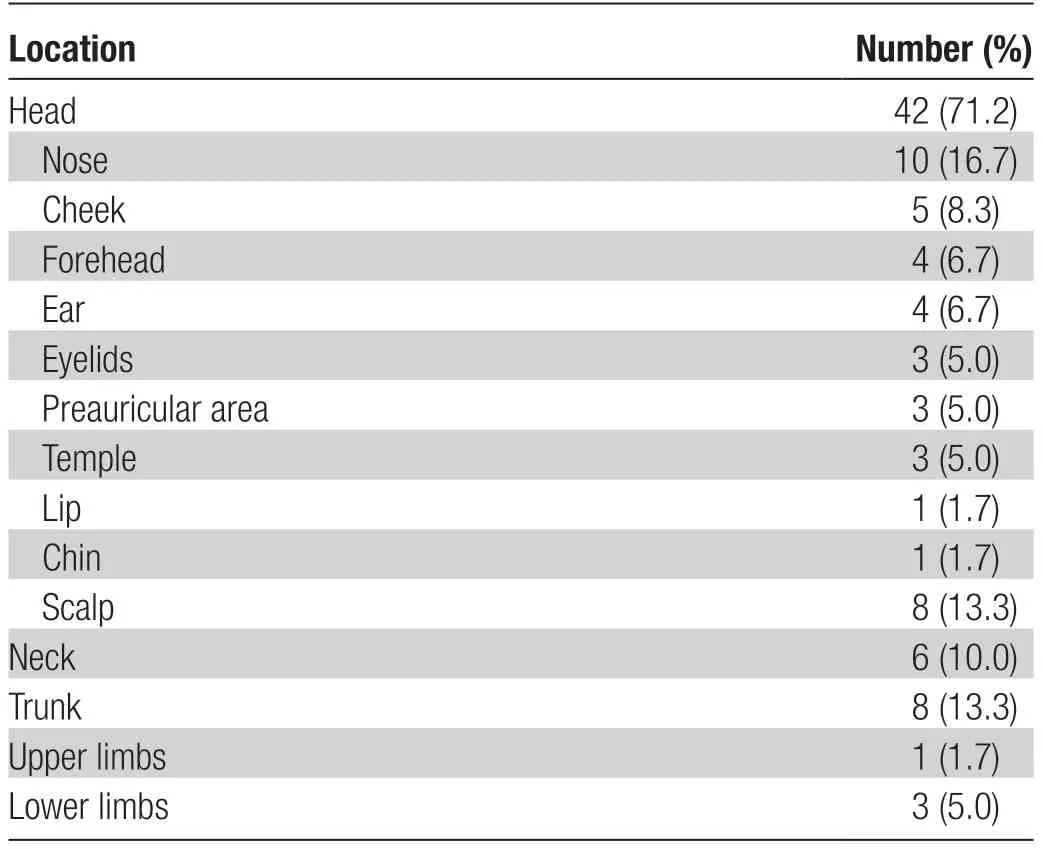
Table 1 Location of the 60 cases of excised basal cell carcinoma.
In all 60 tumors, surgical excision with dermoscopic controlled margins were tumor-free according to the pathology report (Table 2); five tumors had small excision safety margins (≤ 1 mm from the tumor edge), albeit tumorfree.No re-excisions were performed; these patients are under close follow-up, with no tumor recurrences registered.During a medium follow-up period of 31 months, none of the 60 cases showed any clinical evidence of relapse.
Discussion
BCC is a locally invasive cutaneous malignancy.Complete surgical excision is recommended as standard therapy for this common skin cancer.Dermatologists have an extensive training and experience in BCC diagnoses, surgical treatment, and patient follow-up.According to some studies, BCCs were more often excised by dermatologists,rather than plastic surgeons, presumably because the former group had improved clinical skills in recognizing and demarcating tumors, preoperatively.11-13Dermoscopy can increase the diagnostic accuracy for BCC; this technique is increasingly recognized as an important tool for BCC diagnosis, enhancing both sensitivity and specificity when compared to the naked eye.
In addition to improve diagnostic accuracy, several studies have reported that pre-surgical dermatoscopic margin assessments have improved BCC excision over clinical assessments alone.8-10The procedure is easy to perform, is non-invasive, and greatly improves the surgical performance of BCCs for most tumor types and locations.In some of our patients, borders were well-defined clinically, however, dermoscopy showed larger extensions, occasionally with non-pigmented areas.In these cases, without dermoscopy, a complete excision would have been difficult.
In our practice, international guidelines recommend that low-risk primary BCCs are surgically excised with 4-mm clinical margins.This is in spite of several studies suggesting that narrow margins of approximately 3 mm can be safely used for non-morpheaform basal BCCs.14-15
Equally, some studies pre-surgically evaluate borders using dermoscopy; safety margins can be decreased to 2 mm, sparing healthy tissue without compromising a successful and complete BCC excision.8,10Such a narrow excision margin in dermoscopy-guided surgery facilitates easier reconstruction, with direct closure and better cosmetic results for most cases.However, more studies are required to confirm this data and to review existing guidelines.
In Macau, the Portuguese community enjoy high recreational sun exposure that frequently requires follow-up for different cutaneous malignancies.This fact is reflected by the high numbers of Caucasians in our sample with BCC.
Dermoscopy-guided BCC surgery in the 60 tumors showed complete excision in all cases after histological examination.In five cases, the excision margin was<1 mm, only a few microns from the tumor edge, albeit tumor free.No re-excision was performed and no relapses occurred during the follow-up period.
This study had several limitations: patient numbers were relatively small, and we had a short median follow-up period of just 31 months.Additionally, the extension of the safety margin in our sample was not compared with a control group and further studies comparing dermoscopy-assisted excision versus conventional excision are needed in order to better evaluate the value of this technique.
This retrospective study supports the notion that pre-surgical evaluation of tumoral margins using dermoscopy, adequately facilitate lesion excision - increasing the prospects for a successful BCC excision, sparing healthy adjacent tissue.
杂志排行
国际皮肤性病学杂志的其它文章
- Transcription and Secretion of lnterleukin-1β and HMGB1 in Keratinocytes Exposed to Stimulations Mimicking Common lnflammatory Damages
- Dermoscopic Assessment of Pityriasis Versicolor: A Cross-Sectional Observational Study
- Evaluation of Serum Vitamin D Concentration and Blood Eosinophil and Basophil Counts in Patients With Vitiligo: A Cross-sectional Study From Rafsanjan and Zarand, Iran
- Teledermatology During the COVID-19 Pandemic in a Developing Country: Could This Be the Answer to Improving the Reach of Dermatology Care?
- The Role of Endoplasmic Reticulum Stress in Melanoma
- The Relationship Between Ultraviolet B and DNA Methylation in Skin Cancers
