Dermoscopic Assessment of Pityriasis Versicolor: A Cross-Sectional Observational Study
2023-10-20NavakumarManickamPraveenVasanthiSaminathanDeepikaVazhavanthanKannanGopalan
Navakumar Manickam, Praveen Vasanthi Saminathan, Deepika Vazhavanthan, Kannan Gopalan
Department of Skin & STD, Vinayaka Mission’s Kirupananda Variyar Medical College & Hospital, Vinayaka Mission’s Research Foundation (deemed to be University), Salem, Tamil Nadu 636308, India.
Abstract
Keywords: dermoscopy, hypopigmented, hyperpigmented, pityriasis versicolor, tinea versicolor
Introduction
Pityriasis versicolor (PV) or tinea versicolor is a mild,chronic, recurrent/relapsing superficial infection of the skin caused by theMalasseziaspecies, which is a lipophilic dimorphic fungus.PV is characterized by discrete or confluent, scaly, discolored, or depigmented areas that mainly involve the upper trunk.1The organism is present as a normal commensal of the skin in 90% to 100% of individuals.PV occurs when there is an overgrowth of fungus due to certain predisposing factors such as moisture, heat, and skin occlusion by clothing or cosmetics.1It can present as hypopigmented/achromic lesions, hyperpigmented/chromic lesions, or a combination of both.Morphologically, the lesions can be macular, patchy, papular, follicular, or perifollicular.2The prevalence of PV in tropical countries such as India is about 40% to 50%, mainly because of the warm and humid climate.3
PV is usually asymptomatic, and the social stigma of discolored patches or a cosmetic concern is the main reason that patients seek medical consultation.Although PV is a straightforward diagnosis, it can sometimes mimic other disorders such as early vitiligo, pityriasis alba, seborrheic dermatitis, pityriasis rosea, erythrasma, or confluent and reticulated papillomatosis.4In uncertain cases,microscopic examination with 10% potassium hydroxide(KOH) is performed to confirm the diagnosis.However,KOH does not always reveal the hyphae and spores, and fungal culture is time-consuming and expensive to perform on a regular basis.5Dermoscopy can be a valuable aid in such cases because it can easily detect the fine scaling in PV that is not visible to the naked eye.
Dermoscopic studies of PV have been previously reported in the literature.6-9However, such data are sparse, prompting us to study the various dermoscopic features and their utility in the diagnosis of PV.
Materials and methods
Patients
This was a hospital-based cross-sectional observational study conducted among 57 patients with newly diagnosed PV who visited our dermatology outpatient department over a period of 1 year from September 2020 to September 2021.
The inclusion criteria of patients were the presence of PV and an age of ≥18 years.The exclusion criteria were lack of consent, previous use of topical or systemic antifungals in the past 6 months, and coexisting dermatoses such as psoriasis or vitiligo.
Demographic details and relevant clinical findings were recorded in a predesigned pro forma document, and all clinically diagnosed cases were further confirmed by microscopic examination with 10% KOH.The evoked scale sign was elicited, in which the lesion was stretched between the forefinger and thumb thereby making the fine scales over the lesion more apparent.10-11One representative lesion from each patient was selected and subjected to dermoscopy using a handheld pocket dermoscope(DermLite DL4; DermLite LLC, San Juan Capistrano,California, USA).The glass plate of the instrument was placed directly over the skin lesion, and the lesions were observed in polarized mode at 10× magnification without any contact medium.Dermoscopic images were captured using a high-resolution mobile phone camera (iPhone X;Apple Inc., Cupertino, California, USA) attached to the dermoscope.Dermoscopic patterns in the images were interpreted by two independent dermatologists.
The study was approved by the institutional ethics committee (VMKVMC&H/IEC/21/024), and was performed in adherence to the Helsinki declaration.All patients gave written informed consent.
Statistical analysis
SPSS version 22 software (IBM Corp., Armonk, New York) was used.Continuous variables are expressed as mean ± standard deviation, and categorical variables are expressed as number and percentage.The possible associations between qualitative data (ie, dermoscopic patterns,PV types, and sites involved) were analyzed using the chisquare test or Fisher’s exact test.APvalue of < 0.05 was considered statistically significant.
Results
The 57 patients comprised 35 (61.40%) men and 22(38.60%) women, and the male:female ratio was 1.6:1.0.The patients’ ages ranged from 19 to 85 years (mean age,31.09 ± 14.97 years).The disease duration ranged from 2 months to 3 years.The upper trunk was the most commonly affected site, followed by the upper trunk and arms.PV over the face alone was seen in eight (14.03%)patients.Regarding the type of PV, the hypopigmented type constituted the majority, followed by the hyperpigmented type and the perifollicular type.All patients with facial involvement had hypopigmented PV.The details of the patients’ demographic and clinical characteristics are listed in Table 1.
Nonuniform pigmentation was the most common dermoscopic finding observed in both hypopigmented PV (n= 42, 97.67%) and hyperpigmented PV (n= 12,100%) (Fig.1).Scaling was the next most common finding; patchy scaling (n= 25, 58.13%) and perifollicular scaling (n= 13, 30.23%) were commonly seen in hypopigmented PV, while hyperpigmented PV showed more diffuse scaling (n= 6, 50.00%) followed by patchy scaling (n= 5, 41.66%) (Fig.2A-2D).Furrow scaling was seen in 11 (19.30%) lesions overall, and all of them showed unique “double-edged scales” on dermoscopy after eliciting a positive evoked scale sign (Fig.3A).Hypopigmentation around the hair follicle (n= 24,55.81%) and perilesional hyperpigmentation (the halo sign) (n= 15, 34.88%) (Fig.3B) were the other unique and interesting features seen in hypopigmented PV and were statistically significant.Clearly demarcated borders(n= 20, 46.51%) and inconspicuous ridges and furrows(n= 20, 46.51%) (Fig.1) were also frequently seen in hypopigmented PV.Erythema was seen in 8 (14.03%)lesions, including 7 (16.28%) patients with hypopigmented PV and 1 (8.33%) with hyperpigmented PV(Figs.3B and 3C).Both patients with perifollicular PV showed dermoscopic features such as hypopigmentation around the hair follicle and perifollicular scaling(Fig.2D).The dermoscopic findings among various types of PV are compared in Table 2.We also assessed the dermoscopic findings with respect to the sites examined and found that facial lesions showed predominant patchy scaling, none of them showed diffuse scales, and only one lesion showed furrow scaling; by contrast, PV over the upper trunk and arms showed all types of scaling.Other findings were similar, and the dermoscopic findings with respect to sites examined are shown in Table 3.
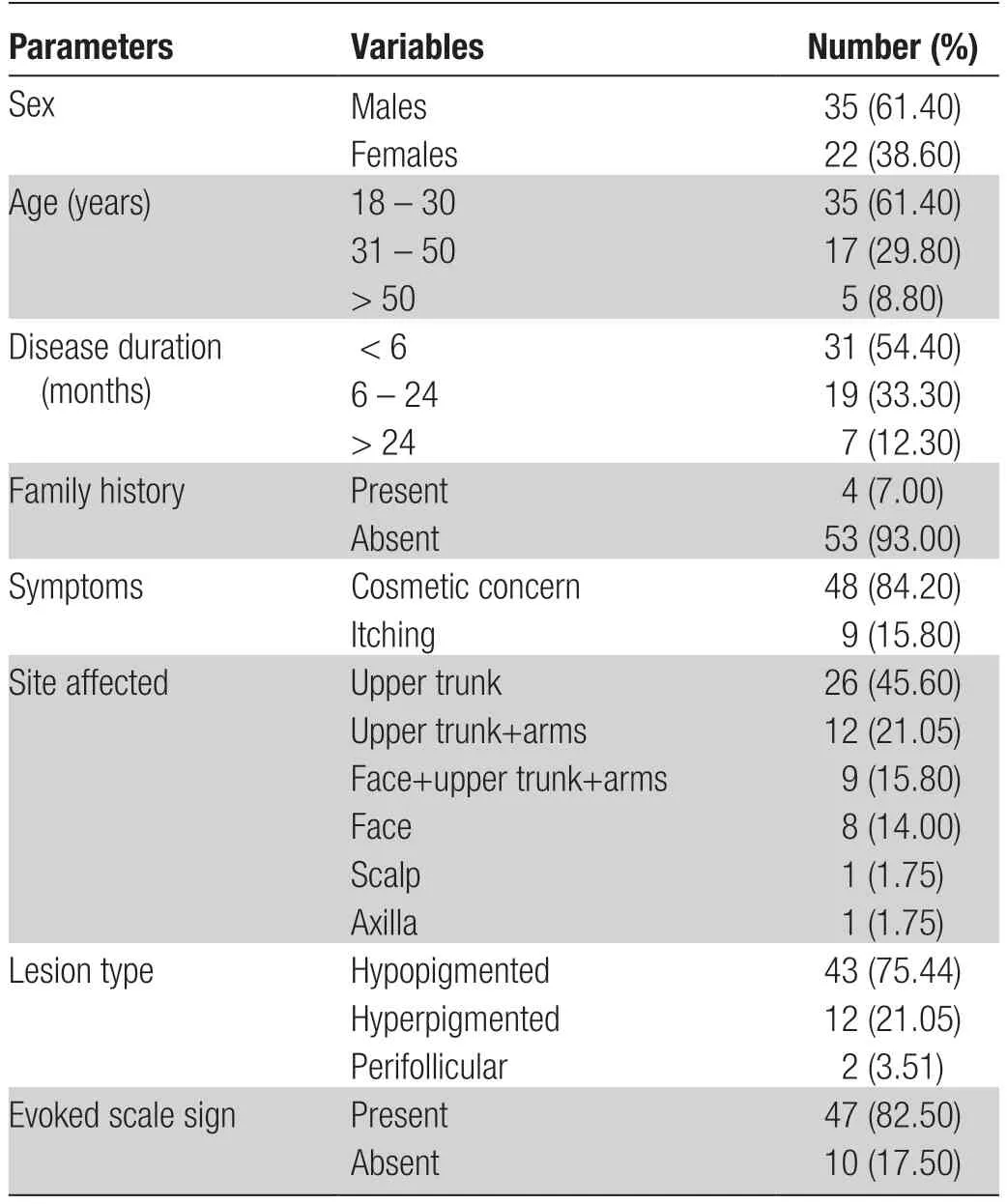
Table 1 Demographic and clinical characteristics of the patients with pityriasis versicolor included in this study.
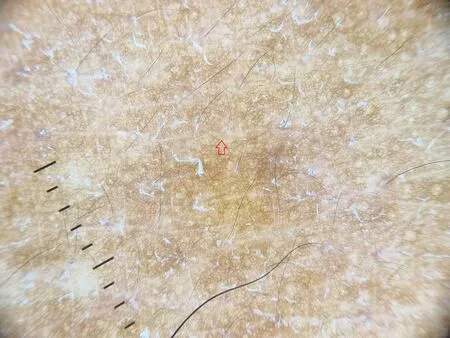
Figure 1.Dermoscopy of hypopigmented pityriasis versicolor(× 10).Nonuniform pigmentation and inconspicuous ridges and furrows (red arrow) are observed.
Discussion

Figure 2.Dermoscopy showing various patterns of scaling in PV (× 10).(A) Diffuse scaling in hyperpigmented PV.(B) Simultaneous presence of patchy (red arrow) and perifollicular scaling (black arrow) in hypopigmented PV.(C) Furrow scaling in hypopigmented PV.(D)Hypopigmentation around the hair follicle with scaling in perifollicular PV (black arrow).PV: pityriasis versicolor.

Figure 3.Dermoscopy features of hypopigmented lesion of pityriasis versicolor ( × 10).(A) “Double-edged” scales (black arrow) in a hypopigmented lesion with furrow scaling after eliciting the evoked scale sign.(B) Perilesional hyperpigmentation (the halo sign) (black arrow) and erythema (red arrow).(C) Erythema (red arrow) within the lesion (arrows).
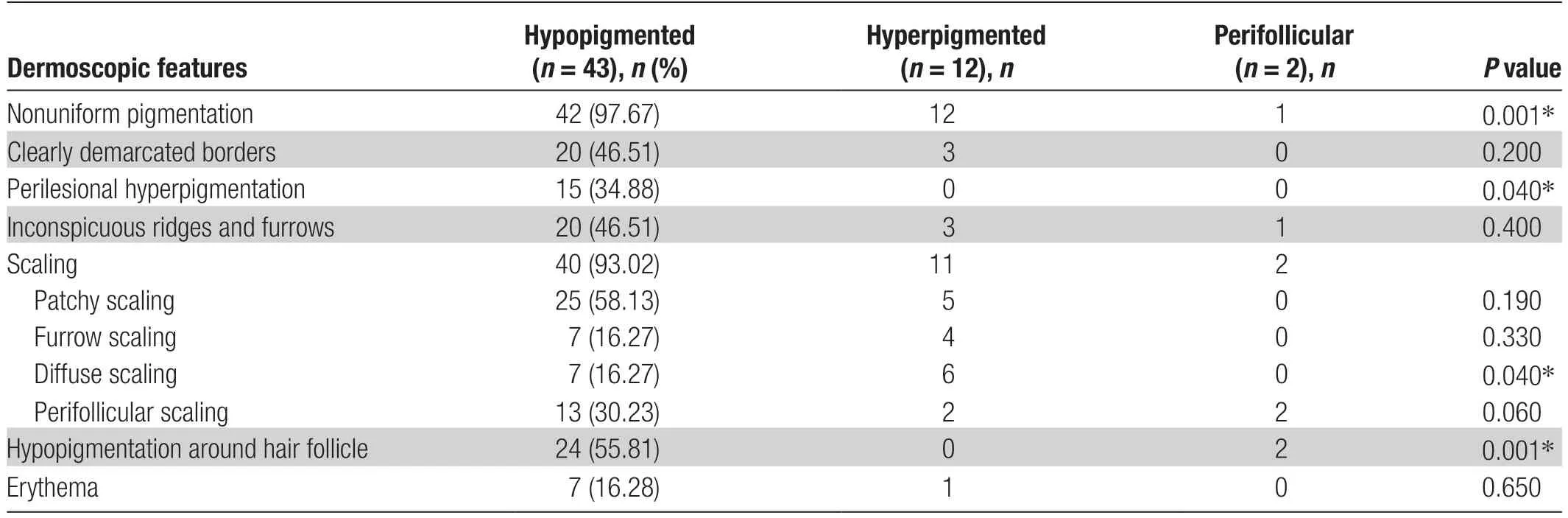
Table 2 Dermoscopic variables of various types of pityriasis versicolor lesions.
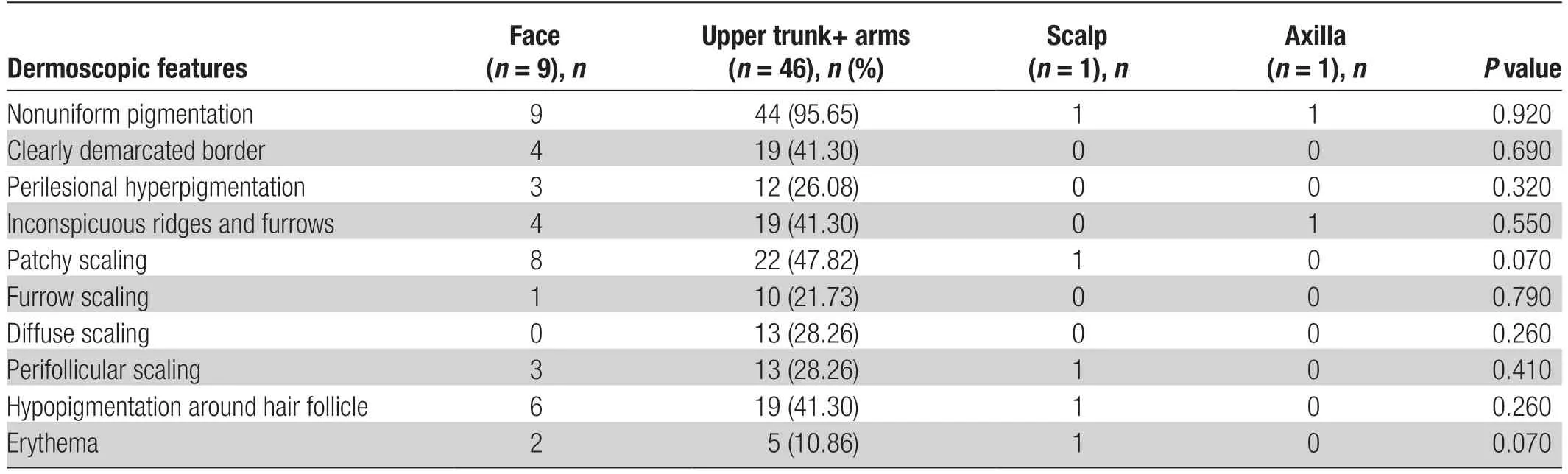
Table 3 Dermoscopic features of pityriasis versicolor lesions from various sites examined.
PV is uncommon in childhood but becomes more common in the late teens, with a peak in the early 20s.The condition is more common in tropical countries than in temperate zones, affecting as much as 40% of the population.The diagnosis of PV is mainly clinical and based on the characteristic clinical appearance and distribution of the lesions.12In uncertain cases, microscopic examination of skin scrapings with 10% KOH can be performed, which readily identifies theMalasseziayeasts.KOH examination demonstrates the characteristic short,thick hyphae with clusters of a large number of rounded or oval yeast spores (spaghetti and meatball appearance)diagnostic of PV.3,13However, KOH mount is not 100%sensitive for the diagnosis of PV.14Additionally, interpretation of the KOH results requires a certain amount of expertise and time because of the absence of color contrast in smears.Examination of the lesion with a Wood’s lamp may show gold-yellow, yellowish-green, or coppery-orange fluorescence, although some lesions do not fluoresce.11Other investigations, such as culture and molecular methods, are time-consuming and expensive.5
Dermoscopy, or skin surface microscopy, is a noninvasive tool that was previously used in the evaluation of skin malignancies and has emerged as an important aid in the diagnosis of other nonmalignant skin conditions during the last decade.15Dermoscopy is still a relatively unexplored area in the diagnosis of PV, with very few data reported thus far.In the present study, we made various dermoscopic observations and compared their relevance with previous studies, which could add more significance to dermoscopy being an effective tool in the diagnosis of PV.
Most (n= 35, 61.40%) of the patients in our study were in the younger age group of 18 to 30 years, consistent with previous studies.3,16-17This is an expected outcome given the increased sebum production at a younger age and the lipophilic nature of the yeast.We discovered that male patients (n= 35, 61.40%) outnumbered female patients (n= 22, 38.60%) by a ratio of 1.6:1.0,a finding that is almost identical to that reported by Kauret al.9(1.5:1.0) and other studies.3,17This could be attributed to excessive sweating in men caused by heat and humidity during outdoor work.We observed that PV favored sebum-rich areas such as the upper trunk(n= 26, 45.46%) and face (n= 8, 14.03%) and was characterized by predominantly hypopigmented lesions(n= 43, 75.44%), similar to other studies.3,9,16-17
In a retrospective study by Mathuret al.,8nonuniform pigmentation was the most common dermoscopic feature in all hyperpigmented lesions and in 92.68% of hypopigmented lesions.It was characterized by altered colors within the lesion.8Kauret al.9also observed an altered pigmentary network in all patients with hypopigmented and hyperpigmented lesions.In the present study, we observed nonuniform pigmentation as the most common dermoscopic finding in both hypopigmented (97.67%) and hyperpigmented lesions(100.00%), similar to the above-mentioned studies.
A clearly demarcated border was seen in 20 (46.51%)hypopigmented and 3 (25.00%) hyperpigmented lesions.These proportions are higher than those reported by Mathuret al.,8who described a clearly demarcated border in 26 (15.85%) hypopigmented lesions and 2 (15.28%)hyperpigmented lesions.However, the number of patients and the number of lesions studied were much higher in their study, which might have affected the sensitivity.
In the present study, all patients with perilesional hyperpigmentation (n= 15, 34.88%) on dermoscopy had hypopigmented PV clinically, and this finding was statistically significant (P= 0.036).This is consistent with the observation by Mathuret al.,8who reported that 56(34.15%) hypopigmented lesions had perilesional hyperpigmentation compared with no hyperpigmented lesions.This finding was also reported by Kauret al.9(91.66%hypopigmentedvs.66.66% hyperpigmented lesions).They proposed that the contrast halo in the hypopigmented variant could be a result of reactive melanogenesis to the cytotoxic damage mediated by yeasts and abnormal melanosomes in the primary lesion.In the hyperpigmented variant, this contrast halo could be due to the utilization of melanocytes in the process of stimulated melanogenesis occurring as a result of ongoing perivascular inflammation in the primary lesion.
Inconspicuous ridges and furrows were another common and interesting dermoscopic finding noted in 20(46.51%) hypopigmented and 3 (25.00%) hyperpigmented lesions, consistent with the report by Mathuret al.8This could be due to the obscuring of ridges and furrows by increased scaling and an altered pigmentary network within the lesion.
Vitiligo, pityriasis alba, indeterminate leprosy, and progressive macular hypomelanosis resemble lesions of hypopigmented PV.18The classic fine scales in PV lesions are not easily visible to the naked eye.12Similarly, it is difficult to appreciate perifollicular and perilesional scaling; in such cases, dermoscopy can serve as an effective tool to demonstrate such scales and help differentiate PV from other pigmentary disorders.12,19In pityriasis alba,the scales are white and focally distributed and are not prominent in skin cleavage lines.This particular dermoscopic feature differentiates pityriasis alba from PV.Scales present in the furrows in PV detach from the skin and break into two parts when the lesions are stretched,a feature described as “double-edged” scales.This may be a special clue indicating PV because this feature is not seen in other hypopigmented lesions.18,20In the present study, we observed this unique dermoscopic pattern in all lesions with furrow scales after eliciting a positive evoked scale sign.Mathuret al.8observed scaling as a frequent dermoscopic finding, with patchy scaling (57.93%) more commonly seen in hypopigmented lesions and scaling in the furrows (50.00%) commonly seen in hyperpigmented lesions.They also found more diffuse scaling in hyperpigmented lesions than in hypopigmented lesions(35.71%vs.8.54%, respectively) and suggested that this increased severity of scaling in hyperpigmented lesions can be correlated with disease activity.Hyperpigmented PV is characterized by a higher number of organisms and a more pronounced inflammatory infiltrate compared with hypopigmented PV.8We also observed patchy scaling (58.13%) more commonly in hypopigmented lesions,followed by perifollicular scales (30.23%).In contrast,the hyperpigmented type showed more diffuse scaling(50.00%), and this was found to be statistically significant (P= 0.04).Kauret al.9observed scaling in 83.33%of cases, and the scales were seen predominantly along the dermatoglyphics.
Hypopigmentation around the hair follicle indicates invasion of the hair follicle byMalasseziayeasts, which are known to show a tendency for similar follicle invasion in pityrosporum folliculitis.21This may serve as an important diagnostic clue to differentiate PV from other hypopigmented disorders.In their cross-sectional study,Kauret al.9observed hypopigmentation around the hair follicle in 6 (25.00%) of the patients with hypopigmented lesions.In our study, hypopigmentation around the hair follicle was a significant feature seen in hypopigmented lesions (24, 55.81%) (P= 0.001).Another sign of follicle involvement was the perifollicular scaling noted in both hypopigmented (n= 13, 30.23%) and hyperpigmented(n= 2, 16.66%) lesions.Although only two patients had perifollicular PV, both of them showed perifollicular hypopigmentation and scaling.
Erythema was observed in a few patients in our study,including seven (16.28%) hypopigmented lesions and one hyperpigmented lesion.Mathuret al.8observed vascular features less frequently and only in hypopigmented lesions.They suggested that vascular features may indicate an ongoing inflammatory reaction to the causative agent.
We also assessed the dermoscopic findings with respect to the site examined and found that facial lesions showed predominant patchy scaling, whereas none of them showed diffuse scales and only one lesion showed furrow scaling.However, there were too few facial lesions to comment on their significance.Common dermoscopic findings are compared between previous studies and the present study in Table 4.
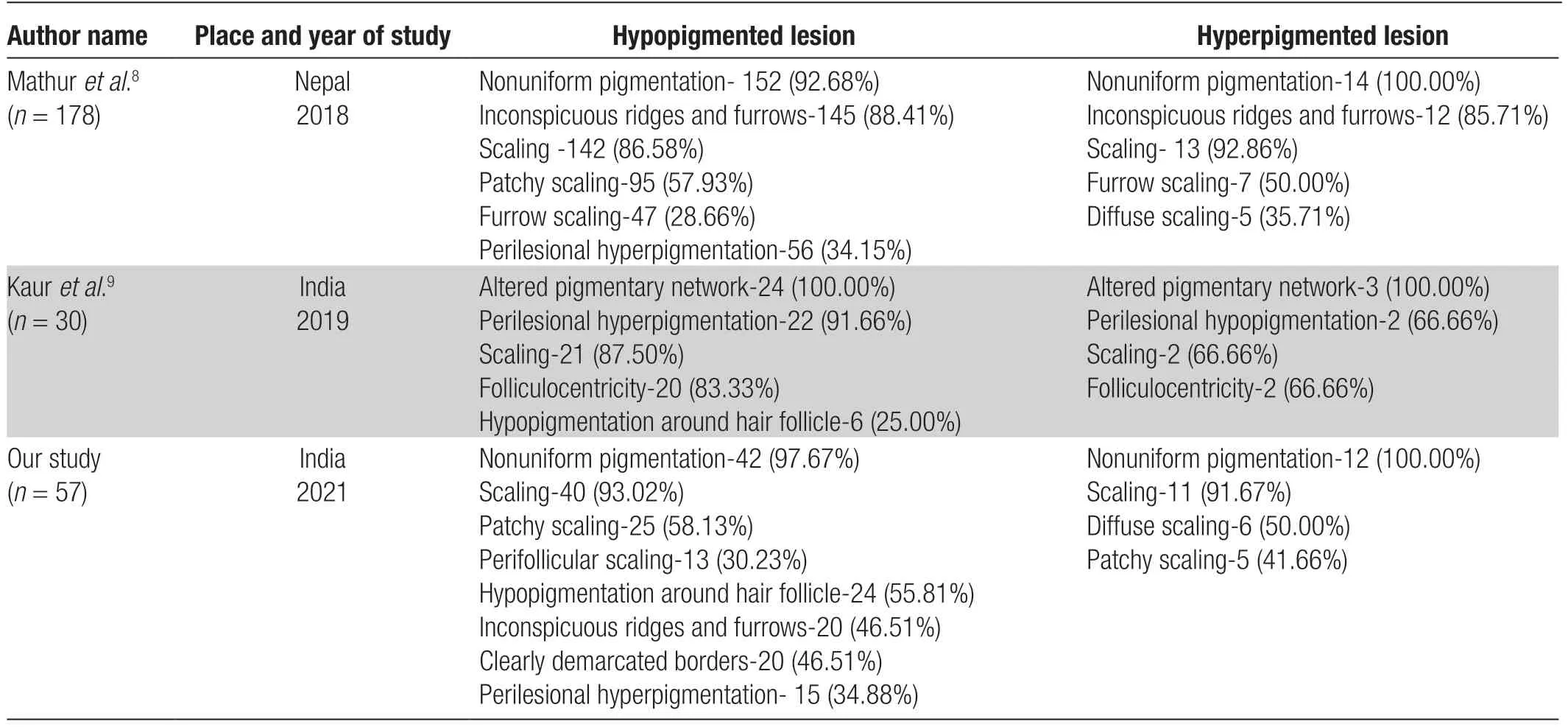
Table 4 Summary of common dermoscopic findings in various studies.
The major limitations of our study were the small sample size and the inclusion of a relatively low number of patients with hyperpigmented PV.Another limitation was the cross-sectional nature of the study design; a large case-control study would have further substantiated the dermoscopic features of PV.
In conclusion, our study revealed several dermoscopic features such as nonuniform pigmentation, scaling, clearly demarcated borders, inconspicuous ridges and furrows, perilesional hyperpigmentation (the halo sign), and perifollicular hypopigmentation.All of these findings can be utilized in the diagnosis of PV, especially in atypical cases and uncertain cases after the KOH test.“Double-edged” scales on dermoscopy are an interesting feature seen as unique to PV.Detection of perifollicular hypopigmentation and fine scales in particular can be important diagnostic clues for differentiating PV from other pigmentary disorders.Dermoscopy can be a valuable addition to the diagnostic armamentarium of PV.
杂志排行
国际皮肤性病学杂志的其它文章
- Transcription and Secretion of lnterleukin-1β and HMGB1 in Keratinocytes Exposed to Stimulations Mimicking Common lnflammatory Damages
- Evaluation of Serum Vitamin D Concentration and Blood Eosinophil and Basophil Counts in Patients With Vitiligo: A Cross-sectional Study From Rafsanjan and Zarand, Iran
- Teledermatology During the COVID-19 Pandemic in a Developing Country: Could This Be the Answer to Improving the Reach of Dermatology Care?
- Basal Cell Carcinoma Excision Guided by Dermoscopy: A Retrospective Study in Macau
- The Role of Endoplasmic Reticulum Stress in Melanoma
- The Relationship Between Ultraviolet B and DNA Methylation in Skin Cancers
