Efficacy of modified folding intraocular lens suspension surgery in treatment of traumatic dislocation of lens
2022-07-12
Department of Ophthalmology, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710061, Shaanxi Province, China
Abstract
KEYWORDS: intraocular lens suspension surgery; dislocation of lens; scleral-fixated technique
INTRODUCTION
Traumatic dislocation of lens is a common complication of ocular blunt trauma, and it may lead to loss of vision, glaucoma, vitreous hemorrhage and retinal detachment[1-2]. So, the patients with traumatic dislocation of lens should receive surgery as soon as possible. Instead of implanting the intraocular lens (IOL) into the capsular bag, IOL suspension surgery is preferred in treatment of traumatic dislocation of lens. The IOL must be fixated in alternative sites of the eye globe, for example, in the iris or the sclera[3-4]. Surgical options includes anterior chamber IOL, iris claw IOL, iris sutured IOL and scleral-fixated posterior chamber IOL which are either sutureless or use suture or glue[5-8]. In recent years, most ophthalmologists prefer the surgery for suture IOL in posterior chamber[9-10]. However, the surgery is complex and it is prone to the postoperative complications, such as slip off, breakage and degradation of the suture. Our study conducts a modified folding IOL suspension surgery in treatment of traumatic dislocation of lens. Suspension with polypropylene suture with no sewing, even suspension with no suture was used in the surgery. The modified surgery efficiently improved the postoperative visual acuity, reduced the surgical injury, lowers the surgical difficultly and avoids the post-operation complications.
SUBJECTSANDMETHODS
SubjectsThere were 15 patients included in this study. The inclusion criteria were listed as follows: 1) The patients were suffered traumatic dislocation of lens would like to receive folding IOL suspension surgery; 2) The best corrected visual acuity (BCVA) was better than uncorrected visual acuity (UCVA); 3) Pupil diameter was less than 5 mm under natural light. The exclusion criteria were listed as follows: 1) The patients were suffered traumatic retinopathy or severe eye traumas; 2) The patients who had a history of keratitis, glaucoma, retinopathy or some other eye diseases; 3) The patients who underwent ophthalmic surgery before. This study was conducted from January 2020 to February 2021 in the department of ophthalmology, the First Affiliated Hospital of Xi’an Jiaotong University. The study was approved by the ethics review committee of Xi’an Jiaotong University and was conducted in accordance with the Declaration of Helsinki. We obtained informed consent from each subject for all examinations and procedures.
IOLSelectionTwo aspheric folding IOL were selected in our study. One was Akreos AO, a single-piece IOL, it had four circular haptics. Another was Tecnis ZA9003, a triplicate-pieces IOL, which was made of polymethyl methacrylate. The haptics of Tecnis ZA9003 were robust and would not kink or break easily. Additionally, even when the haptics had been bent acutely, they would return to their original configuration. The detailed characters of the two IOL were shown in Table 1. All the patients selected one type by themselves, based on the personal preference, such as the materials, price and brand.
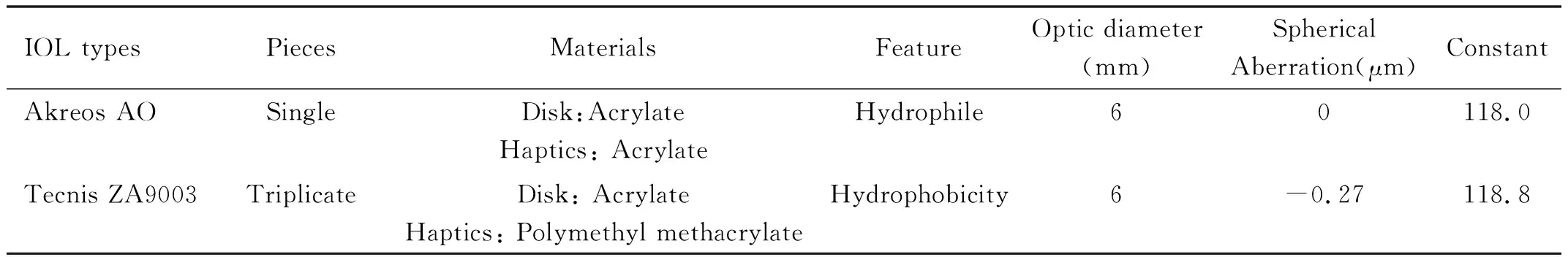
Table 1 Characters of Akreos AO and Tecnis ZA9003
PreoperativeManagementsAll the patients received complete physical examination, including blood coagulation, blood pressure, blood glucose and cardio-pulmonary function, in order to make sure that they could sustain the ophthalmic surgery. Then, complete ophthalmic examinations were performed, including parameters of cornea and corneal endothelium, fundus image, ocular A/B-ultrasound and so on. The IOL degrees were measured by IOL Master 700 and target degree was set as -0.5D. SRK-Ⅱ formula was used. The visual acuity was measured by Snellen visual acuity chart and recorded using five-grade notation. Besides, patients used levofloxacin eye drops for 12 times and received rinsing lacrimal passage before the surgery. The same ophthalmologist performed all of the surgeries.
ModifiedSurgicalTechniqueWhen Akreos AO IOL was used, we first marked the patient carefully and ensured that the four marks were exactly 180° apart and exactly the same distance from the limbus. Then we threaded two unilateral haptics of Akreos AO with 5-0 polypropylene sutures. Then, 27-gauge syringe needle was used to guide the polypropylene sutures to puncture out through the sclera (1.5 millimeter behind the corneal limbus). The direction was started from posterior chamber to the ocular surface. After four sutures were all appropriately placed, the ends of sutures were thermal expanded with thermal cautery set. As a result, the sutures were fixed in the sclera (Figure 1).
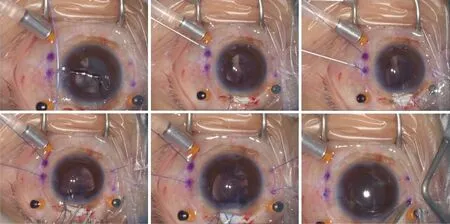
Figure 1 Modified folding IOL suspension surgery with Akreos AO IOL (5-0 polypropylene sutures).
When Tecnis ZA9003 IOL was used, we first marked the patient carefully and ensured that the two marks were exactly 180° apart and exactly the same distance from the limbus. Then we implanted Tecnis ZA9003 into anterior chamber. Then, 27-gauge syringe needle was used to make two incisions on the sclera (1.5 millimeter behind the corneal limbus). The haptics of Tecnis ZA9003 were guided and puncture out from the sclera incision with intraocular microforceps. After two haptics were both appropriately placed, the ends of haptics were thermal expanded with thermal cautery set. As a result, the haptics were fixed in the sclera (Figure 2).

Figure 2 Modified folding IOL suspension surgery with Tecnis ZA9003 IOL (no sutures).

RESULTS
DemographicandBaselineClinicalCharacteristicsofthePatientsThe demographic and baseline clinical characteristics of the patients (age, gender, course of disease and IOL type) were shown in Table 2. And the preliminary analysis was shown in Table 3. There were 9 patients chose Akreos AO IOL and 6 patients chose Tecnis ZA9003 IOL. There was no significant difference between each group (P>0.05).

Table 2 Demographic and baseline clinical characteristics of the patients
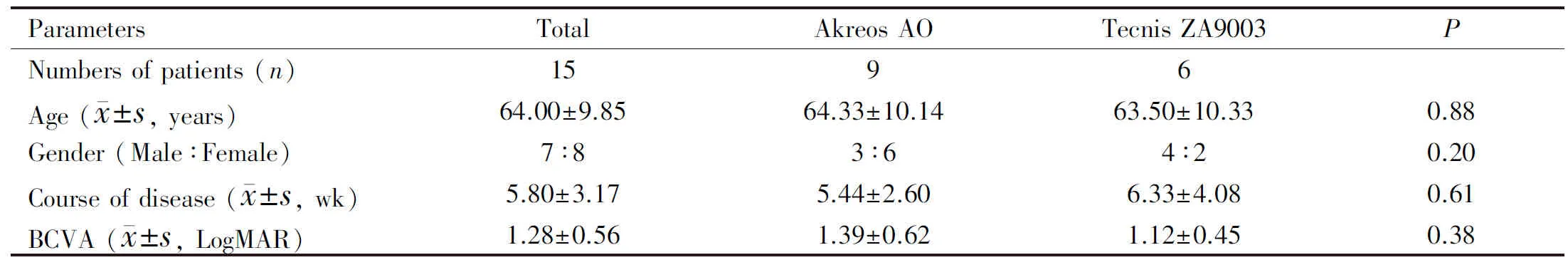
Table 3 Preliminary analysis of demographic and baseline clinical characteristics of the patients
ClinicalCharacteristicsofPatientsAfterSurgeryAfter the surgery at 1 and 3mo, we observed BCVA (LogMAR)of the patients. At 1mo post-surgery, the BCVA (LogMAR) of all patients was 0.59±0.28. The BCVA (LogMAR) of patients who chose Akreos AO was 0.68±0.23, and those who chose Tecnis ZA9003 was 0.43±0.31. At 3mo post-surgery, the BCVA (LogMAR) of all patients was 0.52±0.30. The BCVA (LogMAR) of patients who chose Akreos AO was 0.59±0.25, and those who chose Tecnis ZA9003 was 0.42±0.35. Visual acuity of all the 15 patients was significantly enhanced at 1 and 3mo after the modified folding IOL suspension surgery (allP<0.05; Figure 3). Meanwhile, the duration of surgery dramatic declined.

Figure 3 The BCVA of patients improved significantly after modified folding IOL suspension surgery aP<0.05 vs pre-surgery.
ObservationofPostoperativeComplicationsWe observed the postoperative complications 3mo after the surgery, which including IOL dislocation, corneal endothelial edema, pupillary block and hemorrhage (Table 4). There was one patients suffered a mild IOL dislocation. The IOL optical surface was mild oblique. Besides, there was no severe complication occurred.

Table 4 Postoperative complications after modified folding IOL suspension surgery n
DISCUSSION
Intrascleral IOL haptic fixation via a double-needled, flanger haptic technique (Yamane technique) was first described by Yamane and colleagues[11]. It had been used as a replacement for a dislocated IOL or as rescue therapy when the lens were dislocated. The technique has been popularized but two issues still existed, the suture remains over the sclera and the knot, due to its thickness, it was not easily buried inside the eye, and it often requires enlargement of sclerotomy, making leakage more frequent.
In the past decades, efforts have been made to avoid IOL incline or decentring, increase suture longevity, and minimize complications[12-13]. In our study, we presented two modified folding IOL suspension surgery technique and overcame the problems of leakage. Two kinds of IOL including Akreos AO and Tecnis ZA9003 were used. We chose Akreos AO because it had four annular haptics, and we could thread 5-0 polypropylene sutures through the haptics. Furthermore, after the polypropylene sutures were guided and puncture out through the sclera, the ends of sutures were thermal expanded to fix in the sclera. This modified scleral fixation of IOL without sewing obtained a lower risk of suture exposure, and reduced the operating time because it avoided intricate surgical techniques. In 2020, Canabravaetal[14]reported a four-flanged intrascleral IOL fixation technique. He used 5-0 polypropylene suture and a bipolar cautery to fixate the IOL. Our study also used four flanged. The difference was that we thread 5-0 polypropylene sutures through the annular haptics and the four flanged were all fixed in the sclera. Obviously, four haptics could achieve more stable IOL fixation. The second surgery technique with Tecnis ZA9003 in our study further avoided suture. The haptics of Tecnis ZA9003 were guided and puncture out from the sclera incision. Then, the ends of haptics were thermal expanded and fixed in the sclera. The risk of suture erosion, exposure and breakage were thorough eliminated, and it further reduced the operating time.
Loosened or broken sutures might lead to malposition of IOL, which was one of the severe complications in IOL suspension surgery. A study with an intra-scleral fixation technique reported a 12.5% to 24% IOL dislocation[15-18]. The visual acuity would decrease and it had a higher risk of physical contact with the iris and corneal endothelium. Besides, suture erosion could induce inflammation and increase risk for endophthalmitis[19- 20]. One reason of IOL dislocation was that the suture knots between suture and loop were not firm, and the suture was slipped. Another reason was the degradation and breakage of the suture. In our study, only one patient showed IOL dislocation during the investigation stage. The IOL optical surface was mild oblique. We guessed that it was caused by the weak fixation. The other nine patients who chose Akreos AO avoided this problem well. Moreover, it might due to the relatively short follow-up period in our study.
Severe postoperative complications were not evident in our study, such as intraoperative hyphema, vitreous hemorrhages and secondary glaucoma[21]. But we still asked all the patients in our study to visit subsequently every 3mo. Another possible long-term complication which we had not encountered to date was exposure of the haptic tips. In our study, the ends of sutures were thermal expanded with thermal cautery set. It was blunt and no easily punched out through the conjunctiva.
To sum up, the results of our study showed that modified folding IOL suspension surgery technique resulted in good visual and outcomes with no severe complication, making it an effective option for IOL suspension surgery.
In conclusion, our study conducts a modified folding IOL suspension surgery with no sewing or no suture. It efficiently improved the postoperative visual acuity, reduced the surgical injury, lowers the surgical difficultly and avoids the post-operation complications.
