益生菌联合乳糖酶治疗婴幼儿乳糖不耐受引起的慢性腹泻的临床效果
2020-10-09张莹黄鸣剑张凯真
张莹 黄鸣剑 张凯真
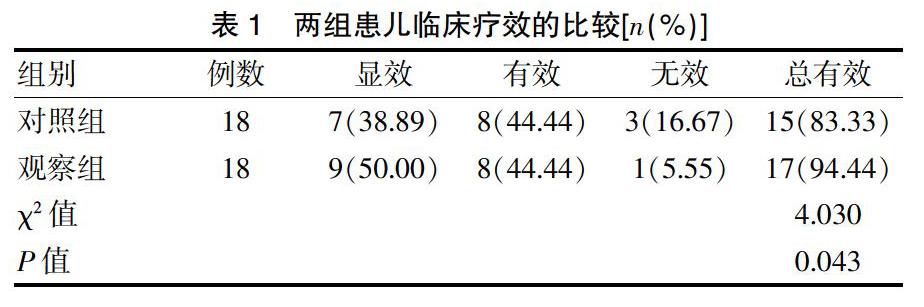
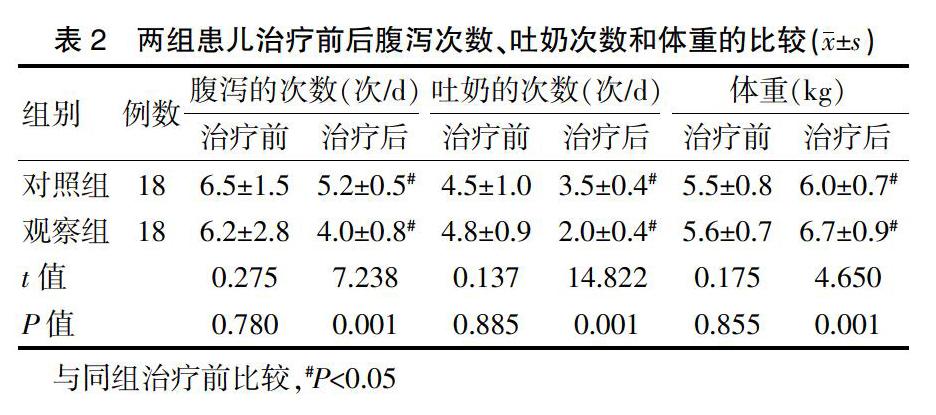
[摘要]目的 探讨益生菌联合乳糖酶治疗婴幼儿乳糖不耐受引起的慢性腹泻的临床效果。方法 选取2019年8月~2020年1月我院收治的36例乳糖不耐受引起的慢性腹泻患儿作为研究对象,按照随机数字表法将其分为对照组和观察组,每组各18例。对照组采用乳糖酶治疗,观察组采用益生菌(酪酸梭菌二联活菌散)+乳糖酶治疗。比较两组患儿的治疗效果、腹泻次数、吐奶次数、体重变化。结果 观察组患儿的临床治疗总有效率(94.44%)高于对照组(83.33%),差异有统计学意义(P<0.05);治疗后,观察组患儿的腹泻次数、吐奶次数少于对照组,体重高于对照组,差异有统计学意义(P<0.05)。结论 益生菌联合乳糖酶治疗婴幼儿乳糖不耐受引起的慢性腹泻效果显著,可以有效减少患儿的腹泻次数和吐奶次数,增加患儿的体重,值得临床推广应用。
[关键词]益生菌;乳糖酶;乳糖不耐受;婴幼儿;慢性腹泻
[中图分类号] R725.7 [文献标识码] A [文章编号] 1674-4721(2020)8(c)-0151-03
[Abstract] Objective To explore the clinical effect of probiotics combined with Lactase in the treatment of chronic diarrhea caused by lactose intolerance in infants and young children. Methods A total of 36 children with chronic diarrhea caused by lactose intolerance admitted to our hospital from August 2019 to January 2020 were selected as the research objects, and they were divided into the control group and the observation group according to the random number table method, with 18 cases in each group. The control group was treated with Lactase, and the observation group was treated with probiotics (Clostridium Caseate Bivalent Viable Powder) combined Lactase. Treatment effect, number of diarrhea, number of vomiting and weight changes were compared between two groups of children. Results The total effective rate of treatment of children in the observation group was 94.44%, which was higher than that of the control group of 83.33%, the difference was statistically significant (P<0.05). After treatment, the numbers of diarrhea and milking in the observation group were fewer than those in the control group, and the weight was higher than that in the control group, the differences were statistically significant (P<0.05). Conclusion The combination of probiotics and Lactase is effective in treating chronic diarrhea caused by lactose intolerance in infants and young children. It can effectively reducing the frequency of diarrhea and vomiting in children, increasing the weight of children, and is worthy of clinical application.
[Key words] Probiotics; Lactase; Lactose intolerance; Infants and young children; Chronic diarrhea
嬰幼儿腹泻是临床上一种较为常见的肠道疾病,主要表现为腹泻、呕吐等症状,其中腹泻分为急性腹泻和慢性腹泻。急性腹泻一般多以感染性为主,慢性腹泻的常见原因为乳糖不耐受。因为婴幼儿的主要能量来源为乳糖,乳糖酶的缺乏使母乳或奶制品中的乳糖不能被分解吸收,随后引起肠腔渗透压增高导致渗透性腹泻;乳糖不耐受为未水解的乳糖被结肠吸收后经细菌分解产生大量的气体,易引发腹胀、腹泻等症状[1]。因乳糖不耐受易导致婴幼儿营养不良、能量摄入不足、贫血,从而影响体格发育和智能发育。因此,婴幼儿慢性腹泻治疗的关键在于解决乳糖不耐受。但是有部分诊断为乳糖不耐受的婴幼儿,使用乳糖酶后腹泻症状改善不明显,因此考虑是否有部分婴幼儿同时存在肠道菌群失调加重其腹泻症状[2]。本研究选取我院收治的36例乳糖不耐受引起的慢性腹泻患儿作为研究对象,探讨益生菌联合乳糖酶治疗婴幼儿乳糖不耐受引起的慢性腹泻的临床效果,现报道如下。
综上所述,当婴幼儿出现乳糖不耐受发生慢性腹泻时,采用益生菌联合乳糖酶的治疗,可明显改善婴幼儿的临床症状,减少患儿的腹泻次数和吐奶次数,增加患儿的体重,改善肠道菌群,提高肠黏膜屏障功能,值得临床推广应用。
[参考文献]
[1]任立红,仰曙芬,孙晓晗.小儿腹泻应用乳糖酶的干预研究[J].中国儿童保健杂志,2011,19(1):62-64.
[2]欧阳美文,周树根,王磊鑫.微生态制剂对小儿急性感染性腹泻患者血清炎性因子肠黏膜屏障功能肠道菌群的影响研究[J].基层医学论坛,2018,22(14):1873-1875.
[3]田巍巍.婴幼儿乳糖不耐受的现状调查及干预效果分析[J].中国儿童保健杂志,2017,25(8):812-814.
[4]刘春贤,方玉玲.美洛西林联合微生态制剂治疗小儿感染性腹泻的疗效观察[J].北方药学,2018,15(2):32-33.
[5]张美玲.小儿肺炎继发腹泻的相关因素分析与微生态制剂的治疗效果观察[J].中外医学研究,2018,16(3):114-115.
[6]陆惠钢.微生态制剂联合蒙脱石散治疗小儿慢性腹泻的临床效果观察[J].中外医疗,2017,36(29):137-139.
[7]马红霞.小儿迁延性腹泻应用锌制剂联合肠道微生态调节剂的临床疗效观察[J].现代消化及介入诊疗,2017,22(4):534-536.
[8]聂非,杨超凡,刘晓红.微生态制剂治疗小儿腹泻的临床疗效探讨[J].当代医学,2017,23(21):92-94.
[9]苑赟.乳糖酶治疗小儿乳糖不耐受临床疗效观察[J].中国社区医师,2017,33(22):79-80,82.
[10]江爱清,余蓉,陈春花.布拉酵母菌联合去乳糖奶粉治疗婴幼儿继发性乳糖不耐受症疗效探讨[J].中国社区医师,2016,32(22):98-99.
[11]胡玉莲,孙文,金二丽.低乳糖奶粉佐治婴幼儿轮状病毒肠炎并乳糖不耐受症临床观察[J].社区医学杂志,2016, 14(14):36-37.
[12]劉艳.无乳糖奶粉用于乳糖不耐受腹泻患儿的效果分析[J].中国继续医学教育,2015,7(33):135-136.
[13]刘晖.乳糖酶辅助治疗轮状病毒肠炎继发乳糖不耐受婴幼儿的疗效观察[J].江苏医药,2015,41(13):1574-1575.
[14]杨辉,李小芹,于静,等.乳糖酶治疗小儿急性腹泻继发乳糖不耐受的临床观察[J].中国民康医学,2015,27(1):63-64.
[15]刘跃平,石涵,李红,等.益生菌对病毒性腹泻患者菌群结构及黏膜屏障功能变化的影响[J].中国预防医学杂志,2018,19(6):448-451.
[16]杨艳君.儿童迁延性腹泻患者肠道菌群和肠黏膜屏障功能的变化以及双歧杆菌三联活菌散的干预作用[J].中国微生态学杂志,2018,30(6):700-702,705.
[17]张晓敏.微生态制剂在小儿腹泻中的疗效及对肠道菌群的影响[J].航空航天医学杂志,2018,29(5):585-587.
(收稿日期:2020-03-31)
