先天性心脏病病儿围手术期血清PCT、IL6及CRP的变化规律
2020-09-29刘乃香曹倩陈瑞吕蓓侯可峰李自普
刘乃香 曹倩 陈瑞 吕蓓 侯可峰 李自普
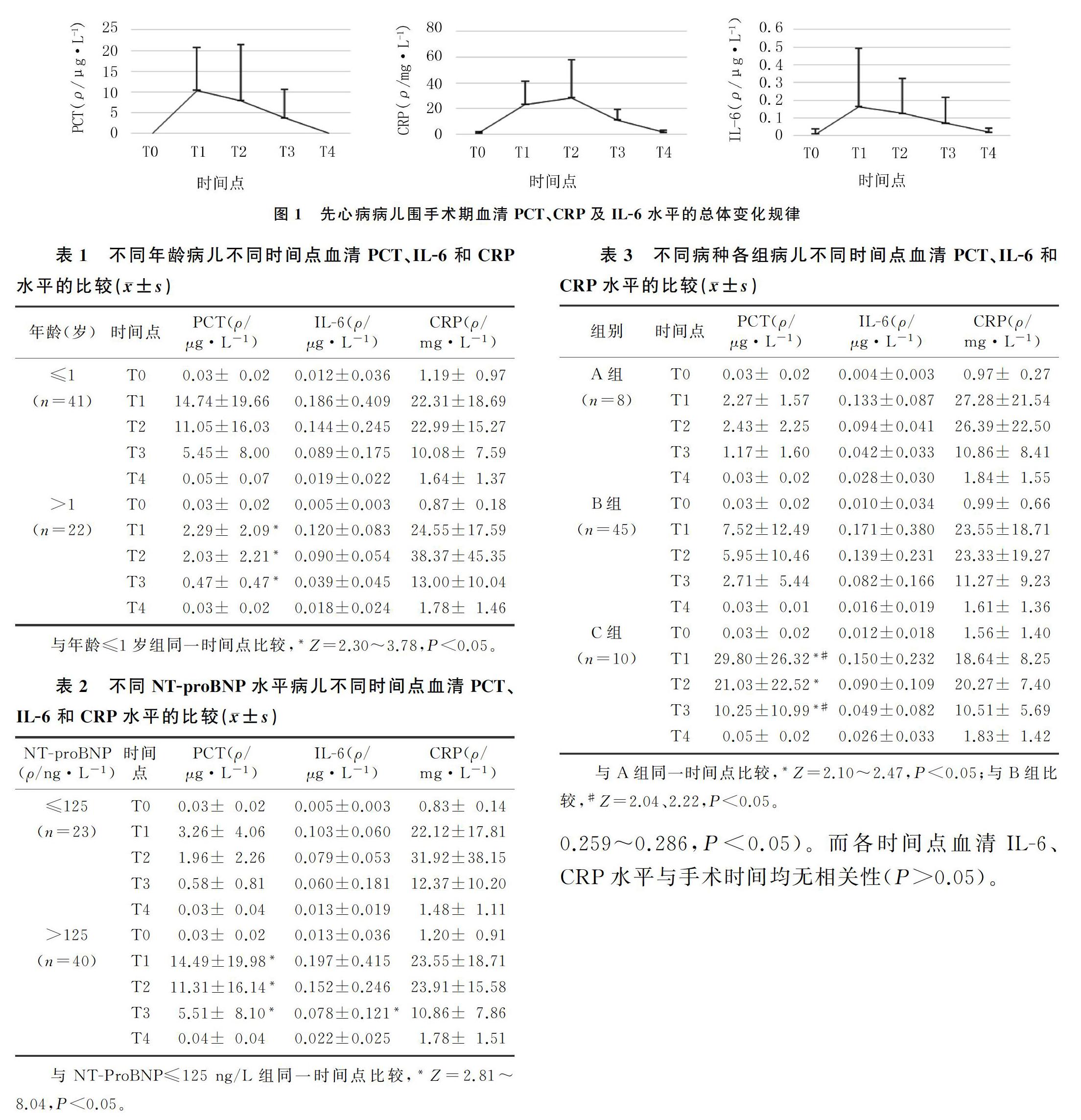
[摘要] 目的 觀察先天性心脏病病儿围手术期血清降钙素原(PCT)、白细胞介素6(IL-6)及C反应蛋白(CRP)水平的变化规律。方法 收集2018年6—8月我院收治的63例拟行体外循环下心内直视手术的先天性心脏病病儿,分别于术前以及术后第1、2、3、7天采集静脉血检测血清PCT、IL-6及CRP水平。结果 先天性心脏病病儿血清PCT、IL-6水平在实施体外循环后开始升高,术后第1天达峰值,之后缓慢下降,至术后第7天接近正常水平;CRP水平在术后第2天达峰值,后渐降至正常。术后PCT峰值水平与手术时间相关(r=0.411,P<0.01),术后第2、3、7天的PCT水平与手术时间也存在相关性(r=0.259~0.286,P<0.05);而术后各时间点IL-6、CRP水平与手术时间均无相关性(P>0.05)。不同年龄、病种、术前N端脑钠肽前体水平的先天性心脏病病儿比较,术后第1、2、3天血清PCT水平差异有统计学意义(Z=2.10~3.78,P<0.05)。结论 血清PCT、IL-6水平在先天性心脏病病儿体外循环术后开始升高,术后第1天达峰值,之后缓慢下降,至术后第7天接近正常水平;而CRP水平在术后第2天达峰值,后渐降至正常。年龄、心功能状态及手术复杂性可影响病儿术后PCT的水平变化。
[关键词] 心脏病;围手术期;降钙素;白细胞介素6;C反应蛋白质;儿童
[中图分类号] R725.411 [文献标志码] A [文章编号] 2096-5532(2020)05-0592-05
doi:10.11712/jms.2096-5532.2020.56.097 [开放科学(资源服务)标识码(OSID)]
[ABSTRACT] Objective To observe the dynamic changes in serum procalcitonin (PCT), interleukin-6 (IL-6), and C-reactive protein (CRP) in children with congenital heart disease (CHD) during the perioperative period. Methods Sixty-three children with CHD, who were admitted to our hospital from June to August 2018 and planned to undergo open-heart surgery with extracorporeal circulation, were enrolled in the study. Venous blood samples were collected from the patients before operation and on the first, second, third, and seventh days after operation to measure serum PCT, IL-6, and CRP levels. Results The serum levels of PCT and IL-6 began to increase after extracorporeal circulation, reached their peaks on the first postoperative day, and then decreased slowly until approaching the normal levels on the seventh postoperative day. The CRP level peaked on the second postoperative day and then gradually decreased to the normal level. The peak level of PCT after operation was significantly correlated with operation time (r=0.411,P<0.01), and the PCT level on the second, third, and seventh days after operation was also significantly correlated with operation time (r=0.259-0.286,P<0.05); neither IL-6 nor CRP level at each time point after operation was significantly correlated with operation time (P>0.05). The serum PCT level on the first, second, third days after operation was significantly different between different age groups, different CHD type groups, and different N-terminal pro-brain natriuretic peptide level groups (Z=2.10-3.78,P<0.05). Conclusion The serum levels of PCT and IL-6 in children with CHD began to increase after extracorporeal circulation, reached their peaks on the first postoperative day, and then decreased slowly until approaching the normal levels on the seventh postoperative day; the CRP level peaked on the second postoperative day and then gradually decreased to the normal level. Age, cardiac function, and surgical complexity are the factors that influence the changes in serum PCT level in CHD children after operation.
3 讨 论
PCT为降钙素前体,正常生理情况下主要由甲状腺C细胞和肺内的一些神经内分泌细胞产生,不具有激素活性。在细菌感染时,细菌内毒素和肿瘤坏死因子-α(TNF-α)、IL-6等细胞因子诱导肝脏的巨噬细胞、肺及肠道组织的淋巴细胞合成并分泌PCT,导致血清PCT水平迅速升高。目前,临床上常用的发热、白细胞计数、血红细胞沉降率及CRP等传统监测指标对炎症反应的灵感度较高,但特异度低[4],且很难区分CPB引起的非感染全身炎症及感染相关性炎症。1993年,ASSICOT等[3]首次提出PCT可作为败血症和感染的生物标志物,并报告其水平与细菌感染的严重程度有关。在大手术(如心胸及腹部手术等)、严重创伤、大面积烧伤等应激下,即使没有细菌感染也可以激发体内TNF-α、IL-6及IL-8等炎性细胞因子释放而诱导血清PCT水平升高,这是一种非特异性表现[5-6]。1998年,HEN-SEL等[7]在急性肺损伤的研究中发现,所有病人血清PCT浓度均显著升高。而手术后即使無感染,血清PCT水平亦会出现一过性升高,且常与CPB术后炎症反应密切相关。KILGER等[8]研究结果显示,术后血清PCT水平显著升高,且行CPB术病人的血清PCT水平比未行CPB术病人高。在CPB下行心内直视手术会影响血清PCT水平[9]。文献报道,在无全身感染情况下,术后血清PCT水平升高,可能与手术创伤、CPB时间、手术时间及主动脉阻断时间等有一定相关性[10-11]。但有关先心病病儿CPB术后血清PCT变化方面的研究较少。因此,本研究探讨了先心病病儿在CPB下行心内直视手术围手术期血清PCT水平的变化规律,结果显示,所有病儿术前血清PCT水平均在正常范围内,在CPB术后无感染的情况下,病儿血清PCT水平在术后24 h内升高并达峰值,术后第2、3天逐渐下降,术后第7天可降至正常水平。对多数病人来说,在无感染等并发症情况下,术后3~5 d内血清PCT水平逐渐下降到正常范围内[10];当发生术后感染等并发症时,SIRS可持续存在,从而导致血清PCT水平持续保持较高水平。另有临床研究发现,新生儿出生后2 d内血清PCT水平生理性增高,达峰值后逐渐恢复到成人水平[12]。不同年龄病儿行CPB后血清PCT水平是否有差异有待研究。本文研究结果显示,年龄≤1岁病儿术后第1、2、3天的血清PCT水平均较年龄>1岁病儿高,差异具有统计学意义。因此,年龄可能是影响CPB后血清PCT水平的重要因素。MALLAMACI等[13]研究显示,心功能不全病人血清PCT水平升高,原因可能与心功能不全时肺部充血显著,易导致肺部细菌生长,从而导致肺部感染率增高有关。国内外的研究均证实,NT-ProBNP在心力衰竭病人血清中的含量与心力衰竭的严重程度呈正相关[14-15]。本研究结果显示,术前NT-ProBNP>125 ng/L病儿术后第1、2、3天的血清PCT水平明显高于NT-ProBNP≤125 ng/L病儿。提示心功能状态亦可能是影响血清PCT水平的重要因素之一。先心病病种不同,手术的复杂程度就不同,对病儿血清PCT水平的变化也有所影响[16-17]。本研究用先心病病种复杂程度分类代表手术的复杂程度,结果表明手术复杂程度亦可影响血清PCT水平变化。
IL-6是一种由两条糖蛋白组成的多肽,主要由单核细胞和巨噬细胞产生,在炎症反应调节中起核心作用,可诱导肝细胞和肺内成纤维细胞合成释放CRP、PCT等急性时相蛋白。某些非感染因素亦会引起血清IL-6水平的非特异性升高[18]。血清IL-6水平升高的程度与病情严重程度及死亡率显著相关,可作为判断预后及观察疗效的指标之一[19-20]。IL-6可调节急性期蛋白质产生,终止B细胞免疫球蛋白分化和分泌,使T细胞失活,也是一种内源性致热原。IL-6主要来源于心肌,和心肌损害具有密切相关性[21]。有文献报道,在儿童心脏手术后IL-6水平升高[22]。本研究中,NT-ProBNP>125 ng/L病儿术后第3天的血清IL-6水平明显高于NT-ProBNP≤125 ng/L病儿,而术后其他时间点两组无明显差异,提示心功能不全可能对血清IL-6水平的下降程度具有一定影响,但这还需进一步研究。CRUICKSHANK等[23]对不同手术类型病人的检测结果显示,血清IL-6水平在切皮后2~4 h均升高,在术后24 h内达到峰值,后逐渐降至正常水平,这与本研究结果一致。CRUICKSHANK等[23]的研究还结果显示,血清IL-6水平与手术复杂程度有密切关系,手术越复杂,手术持续时间越长,IL-6水平越高。本研究结果则显示,手术复杂程度与血清IL-6水平无关,并且手术时间与血清IL-6水平也无明显相关性。本研究结果与上述文献报道不一致,可能是由于IL-6的半衰期短,两研究的标本采集时间差异较大有一定关系。
CRP是在机体受到创伤或炎症造成组织损伤时,由肝脏细胞在IL-6作用下合成释放入血的一种非特异性急性时相蛋白。在感染或任何组织创伤等应激状态下(包括急性创伤、烧伤及手术等非感染状态),CRP水平均显著增高[24]。已有研究显示,病人血清CRP水平均在心脏术后第3天达到峰值[10]。本研究结果显示,CPB术后在无感染状态下,血清CRP水平逐渐升高,在术后第2天达峰值后逐渐下降,至术后第7天大致恢复正常水平,且血清CRP水平不受年龄、心功能状态及手术时间的影响。
综上所述,在CPB术后无感染情况下,血清PCT水平一过性增高,与年龄、心功能状态、手术复杂程度及手术时间等存在一定关系。临床上可于CPB术后24 h开始检测血清PCT水平,若在术后第3天没有迅速下降,应警惕感染及并发症可能。了解CPB术后PCT的变化规律,对临床针对性治疗有一定指导作用,可合理指导抗生素的应用,预防术后并发症的发生。
[参考文献]
[1] SCHULTZ J M, KARAMLOU T, SWANSON J, et al. Hypothermic low-flow cardiopulmonary bypass impairs pulmonary and right ventricular function more than circulatory arrest[J]. The Annals of Thoracic Surgery, 2006,81(2):474-480.
[2] SULEIMAN M S, ZACHAROWSKI K, ANGELINI G D. Inflammatory response and cardioprotection during open-heart surgery: the importance of anaesthetics[J]. British Journal of Pharmacology, 2008,153(1):21-33.
[3] ASSICOT M, GENDREL D, CARSIN H, et al. High serum procalcitonin concentrations in patients with sepsis and infection[J]. Lancet, 1993,341(8844):515-518.
[4] YUKIOKA H, YOSHIDA G, KURITA S, et al. Plasma procalcitonin in sepsis and organ failure[J]. Annals of the Academy of Medicine, Singapore, 2001,30(5):528-531.
[5] SCHUETZ P, AFFOLTER B, HUNZIKER S, et al. Serum procalcitonin, C-reactive protein and white blood cell levels following hypothermia after cardiac arrest: a retrospective cohort study[J]. European Journal of Clinical Investigation, 2010,40(4):376-381.
[6] SPONHOLZ C, SAKR Y, REINHART K, et al. Diagnostic value and prognostic implications of serum procalcitonin after cardiac surgery: a systematic review of the literature[J]. Critical Care (London, England), 2006,10(5):R145.
[7] HENSEL M, VOLK T, DCKE W D, et al. Hyperprocalcitonemia in patients with noninfectious SIRS and pulmonary dysfunction associated with cardiopulmonary bypass[J]. Anesthesiology, 1998,89(1):93-104.
[8] KILGER E, PICHLER B, GOETZ A, et al. Procalcitonin as a marker of systemic inflammation after conventional or minimally invasive coronary artery bypass grafting[J]. The Thoracic and Cardiovascular Surgeon, 1998,46(3):130-133.
[9] ABDELLAH A, PIRIOU V, BASTIEN O, et al. Usefulness of procalcitonin for diagnosis of infection in cardiac surgical patients[J]. Critical Care Medicine, 2000,28(9):3171-3176.
[10] BEGHETTI M, RIMENSBERGER P C, KALANGOS A, et al. Kinetics of procalcitonin, interleukin 6 and C-reactive protein after cardiopulmonary-bypass in children[J]. Cardiology in the Young, 2003,13(2):161-167.
[11] ZANT R, STOCKER C, SCHLAPBACH L J, et al. Procalcitonin in the early course post pediatric cardiac surgery[J]. Pe-diatric Critical Care Medicine: a Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 2016,17(7):624-629.
[12] 彭蕾,朱艷萍. 血清降钙素原和白细胞介素-6及高敏C反应蛋白对新生儿感染性疾病早期诊断价值的研究进展[J]. 中华实用诊断与治疗杂志, 2018,32(4):408-410.
[13] MALLAMACI F, LEONARDIS D, PIZZINI P A, et al. Procalcitonin and the inflammatory response to salt in essential hypertension: a randomized cross-over clinical trial[J]. Journal of Hypertension, 2013,31(7):1424-1430.
[14] TAYLOR C J, ROALFE A K, ILES R, et al. The potential role of NT-proBNP in screening for and predicting prognosis in heart failure: a survival analysis[J]. BMJ Open, 2014,4(4):e004675.
[15] 王正中,王丽,蒲毅,等. 心力衰竭患者血浆BNP、NT-BNP及cTnⅠ水平的变化及其诊断价值研究[J]. 国际检验医学杂志, 2017,38(9):1283-1286.
[16] HAMMER S, ALEXANDRA T F, CARSTEN R, et al. Interleukin-6 and procalcitonin in serum of children undergoing cardiac surgery with cardiopulmonary bypass[J]. Acta Cardiologica, 2004,59(6):624-629.
[17] HVELS-GRICH H H, SCHUMACHER K, VAZQUEZ-JIMENEZ J F, et al. Cytokine balance in infants undergoing cardiac operation[J]. The Annals of Thoracic Surgery, 2002,73(2):601-608.
[18] 徐瑛,谢服役,何立忠,等. PCT、IL-6及hs-CRP在新生儿感染性疾病早期诊断中的价值[J]. 中華医院感染学杂志, 2011,21(9):1934-1935.
[19] BUTLER J, ROCKER G M, WESTABY S. Inflammatory response to cardiopulmonary bypass[J]. Annals Thorac Surg, 1993,55(2):552-559.
[20] WAN S, LECLERC J L, VINCENT J L. Cytokine responses to cardiopulmonary bypass: lessons learned from cardiac transplantation[J]. The Annals of Thoracic Surgery, 1997,63(1):269-276.
[21] HENNEIN H A, EBBA H, RODRIGUEZ J L, et al. Relationship of the proinflammatory cytokines to myocardial ischemia and dysfunction after uncomplicated coronary revascula-rization[J]. The Journal of Thoracic and Cardiovascular Surge-ry, 1994,108(4):626-635.
[22] ARONEN M. Value of C-reactive protein in detecting complications after open-heart surgery in children[J]. Scandinavian Journal of Thoracic and Cardiovascular Surgery, 1990,24(2):141-145.
[23] CRUICKSHANK A M, FRASER W D, BURNS H J, et al. Response of serum interleukin-6 in patients undergoing elective surgery of varying severity[J]. Clinical Science (London, England:1979), 1990,79(2):161-165.
[24] DELANNOY B, GUYE M L, SLAIMAN D H, et al. Effect of cardiopulmonary bypass on activated partial thromboplastin time waveform analysis, serum procalcitonin and C-reactive protein concentrations[J]. Critical Care, 2009,13(6):R180.
(本文编辑 马伟平)
