Managing intraocular lens dislocation with one-port pars plana vitrectomy under direct vision with microscope illumination
2020-08-06JinYangHongFeiYe3XiaoDiQiuLeiCaiYiLu
Jin Yang*, Hong-Fei Ye3*, Xiao-Di Qiu, Lei Cai, Yi Lu
Abstract
•KEYWORDS:intraocular lens dislocation; one-port; pars plana vitrectomy; cataract surgery
INTRODUCTION
Phacoemulsification and intraocular lens (IOL) implantation is one of the most common surgical procedures worldwide, and it has been dramatically improved due to the development of new techniques and devices that make it safer and decrease complication rates.However, postoperative complications are still possible; among these, IOL dislocation is uncommon but the most serious one.Dislocated IOLs can be managed with various surgical options including repositioning, removing or exchanging the IOL[1-2].The site of the dislocated IOL to some extent defines the difficulty of the surgery, and the difficulty is multiplied if the IOL drops completely into the vitreous cavity.Therefore, safely and efficiently retrieving the dislocated IOL is the goal of a successful surgery.
Three-port pars plana vitrectomy (PPV) was chosen in many previous cases[3-5]of posteriorly dislocated IOL in the vitreous cavity.However, PPV also has complications such as retinal detachment and vitreous haemorrhage[6].Additionally, limited equipment and funding in some primary hospitals must also be considered.Therefore, it would be of great benefit if the surgical procedures were made simpler and safer.We now describe a technique of managing IOLs with deep dislocation[7]in the vitreous cavity by performing PPV with only one pars plana incision.
SUBJECTS AND METHODS
This was a retrospective case series.A series of patients who had in-the-bag or out-of-the-bag (spontaneous) IOL dislocation were included.These patients were seen between January 2013 and May 2018 at the Department of Ophthalmology, Eye and Ear, Nose, and Throat Hospital of Fudan University.The institutional review board approved the study and informed consent was obtained from all patients receiving this technique.All the patients had in-the-bag or out-of-the-bag (spontaneous) IOL dislocation after uneventful phacoemulsification cataract extractions, and the dislocated IOL or IOL-capsular bag complex dropped completely into the vitreous cavity.The remaining inclusion and the exclusion criteria were based on the transparency of the refracting media: patients with mild vitreous opacity, such as eyes after vitrectomy and highly myopic eyes with moderate vitreous cortex liquefaction were included, yet patients with cloudy refracting media of any type, including corneal opacity caused by corneal ulcer, degeneration or trauma, asteroid hyalosis or vitreous haemorrhage, are not inappropriate for this technique.Cases with IOL dislocated into anterior chamber, dislocated into anterior vitreous cavity, or dangled in the peripheral vitreous cavity were also excluded.
EthicsApprovalandConsenttoParticipateThis study has been performed in accordance with the Declaration of Helsinki and was approved by the Research Ethics Committee of Eye and ENT Hospital of Fudan University.Written informed consent was obtained from the participant.
ConsentforPublicationWritten informed consent was obtained from the patient for publication of this case report and any accompanying images.A copy of the written consent is available for review by the editor of this journal.
SurgicalProcedureSurgery was performed by a single experienced surgeon under retrobulbar anaesthesia.After retrobulbar anaesthesia was administered using 5 mL of lidocaine 2.0%, the eye was sterilised with povidone-iodine 5% and then was held open with a lid speculum.As Figures 1A and B showed, a limbal port incision was created using a 15° blade at a 2 o’clock position, through which a 23-G infusion cannula was inserted with balanced salt solution (BSS, Alcon Laboratories, Inc.) to maintain the stabilization of the anterior chamber.With a 2.0-mm crescent blade, a 3.0-mm-wide limbal incision was made with one-third of the limbal thickness.Then a pars plana incision was made using a 23-G trocar at an angled approach 3.5 mm from the limbus at a 10 o’clock position (Figure 1C).Thereafter, as Figure 1D demonstrated, the contact viewing lens was placed on the surface of cornea.Instead of inserting a light pipe through the pars plana incision as a light source, the light from the surgical microscope (OPMI Lumera 700, Carl Zeiss Meditec, Jena, Germany) was used to properly illuminate the surgical field.After adjusting the focus of the microscope to the plane of the dislocated IOL, a 23-G suction cutting tip was inserted through the pars plana incision to cut out the vitreous adherent to the IOL as much as possible.Then, the cutting tip was withdrawn, and a 23-G end-gripping vitreous forceps was inserted to grasp and lift the dislocated IOL into the plane of the iris.Subsequently as in Figures 1E and F, while holding the IOL with the vitreous forceps, a 2.65-mm 45° blade was used to dissect the initially-made intrascleral plane to finish the scleral tunnel incision, then an IOL forceps was inserted through this incision to prevent the IOL from slipping into the vitreous again.With or without cutting the IOL into parts using an IOL cutter or intraocular microscissors, the dislocated IOL was removed from the eye.With or without a newly-prepared IOL implantation, the micro cannula of the pars plana incision was removed, and then the main incision was sutured by 10-0 nylon and hydrated with BSS.Intraocular pressure (IOP) was assured to be within a normal range and all incisions were inspected for leakage.Ophthalmic ointment containing tobramycin 0.3% and dexamethasone 0.1% was applied.The eye was covered with an eye pad and plastic shield.
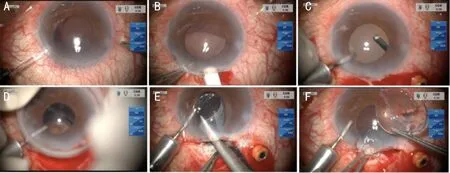
Figure 1 A case of in-the-bag IOL dislocation
ClinicalObservationsPreoperative examination included uncorrected visual acuity (UCVA) and corrected distance visual acuity (CDVA).And no signs of retinal tear/detachment or macular lesion were found in the ultrasound biomicroscopy or optical coherence tomography (OCT) examination respectively, for any of the cases.In all eyes, the IOLs were successfully removed.No intraoperative or postoperative complications related to the procedures occurred.Postoperative patients were followed up for 6mo.CDVA and IOP were recorded (Table 1).
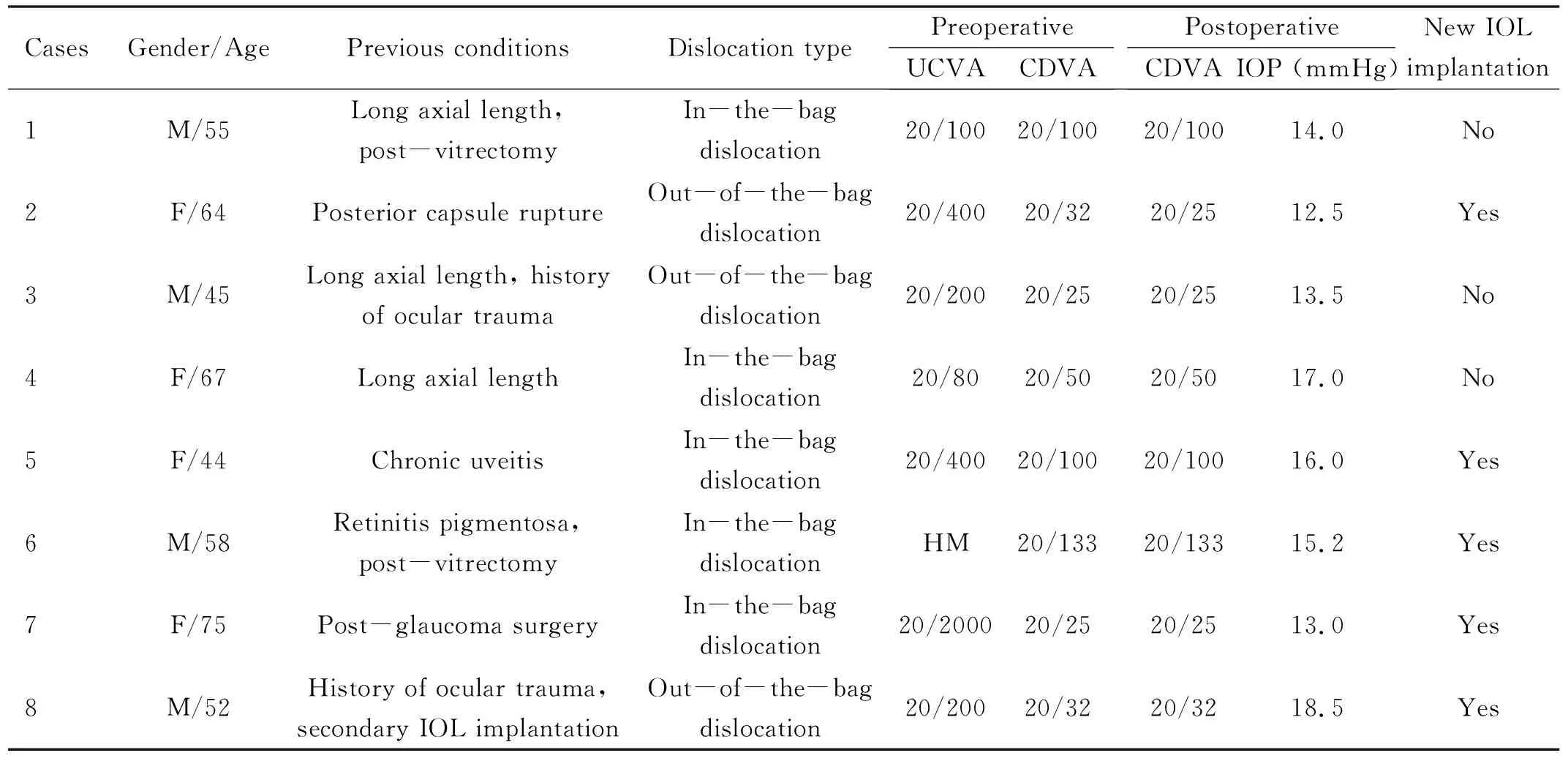
Table 1 Characteristics and clinical data of the cases
RESULTS
The technique was performed in all of the cases referred to our department since 2013 with IOLs deeply dislocated in the vitreous cavity, for a total of 40 surgeries.Among these cases, we chose eight typical ones with detailed follow ups 6mo postoperatively to describe in this paper.All of the pupils were dilated thoroughly, then the peripheral and posterior pole of the patients’ fundus were carefully examined using a three-mirror contact lens.The main possible predisposing conditions included: post-vitrectomy, posterior capsule rupture or broken zonules, a history of ocular trauma, long axial length, secondary IOL implantation, chronic uveitis, retinitis pigmentosa and post-glaucoma surgery.The anterior segment photography showed an absence of IOL in the pupillary zone, and ultrasound biomicroscopy revealed a strong, irregular ribbon-like echo accompanied by a comet tail at the inferior vitreous cavity (Figure 2).
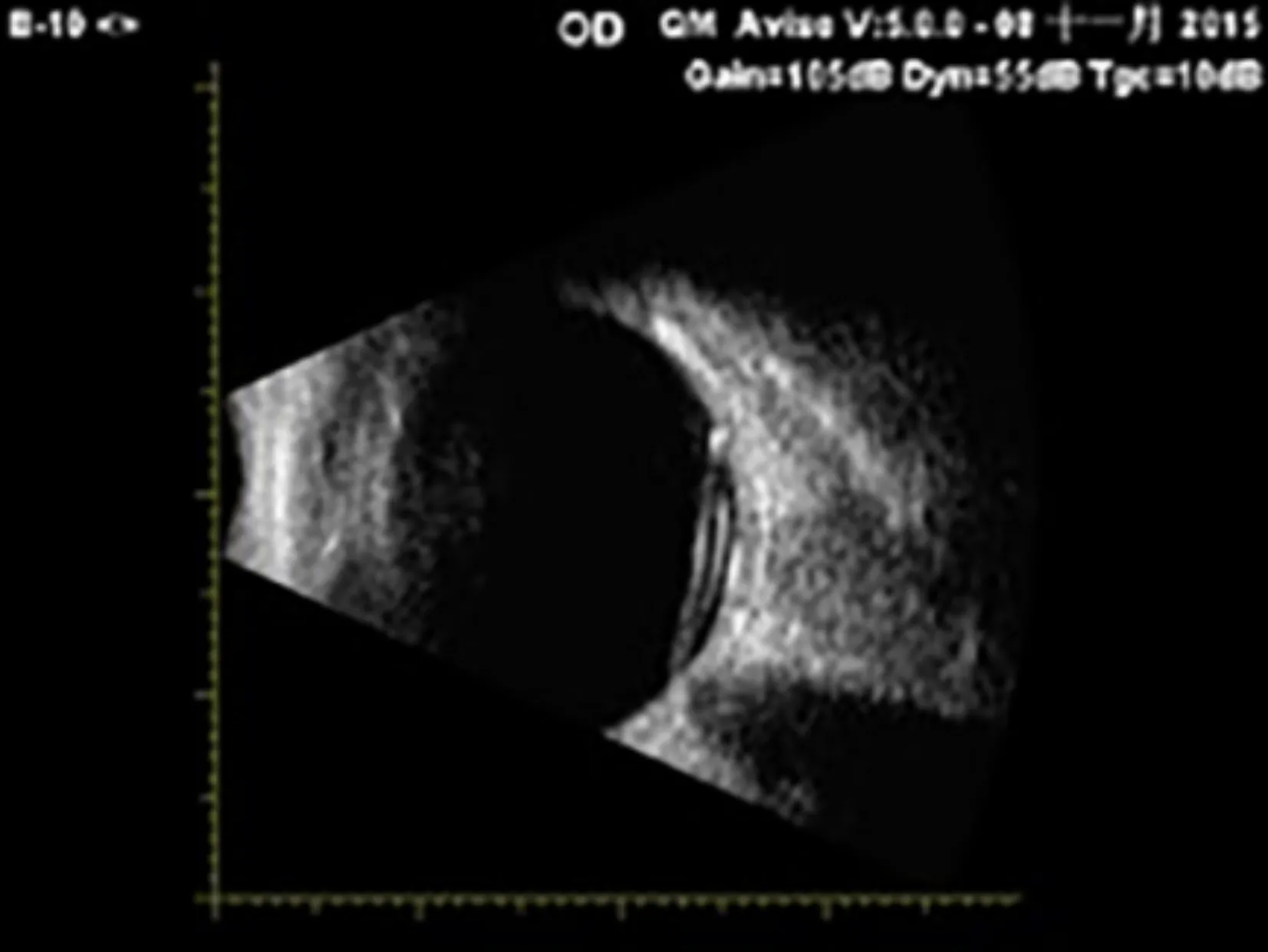
Figure 2 The ultrasound biomicroscopy manifestation of a typical case, showing a strong irregular ribbon-like echo accompanied by a sign of comet tail at inferior vitreous cavity.
Preoperatively, no signs of retinal tear/detachment or macular lesion were found in the ultrasound biomicroscopy or OCT examination, respectively, for any of the cases.In all eyes, the IOLs were successfully removed.No intraoperative or postoperative complications related to the procedures occurred.The preoperative UCVA ranged from hand motion (HM) to 20/80, and CDVA ranged from 20/133 to 20/25.At 6mo postoperatively, the CDVA was similar or the same.None of the eyes lost visual acuity.The IOPs were all in the normal range (Table 1).
DISCUSSION
Our initial experience demonstrates the simplicity and safety of explanting IOLs dislocated deeply in the vitreous cavity using PPV with only one pars plana incision illuminated directly by a surgical microscope light.Compared to conventional three-port PPV, our technique presents several advantages.
Firstly, surgical steps, including making two other pars plana incisions, using a light pipe and fixing the contact viewing lens, are reduced, so that the operation’s speed is greatly improved.We also chose to cut out the vitreous adherent to the IOL instead of the total vitreous, which dramatically shortened the operation time and made the surgery simpler.Secondly, surgical complications have been largely avoided.For conventional three-port PPV, the major complications are bleeding[8](0.14%-0.17%), infection[9](0.039%-0.070%), and retinal detachment[10-11](5.5%-10.0%).Bleeding of pars plana incisions are caused by improper paracentesis, and unstable IOP is a major risk factor for the development of retinal vessel bleeding or even choroidal haemorrhage.Retinal detachment can occur when inadvertent retinal touch causes an iatrogenic retinal break during the procedure.With our technique, the possibilities of bleeding, infection and retinal detachment were significantly reduced due to two fewer incisions.In addition, we performed the anterior chamber infusion through the limbal port incision, which can maintain a more stabilized IOP.More importantly, vitreous adherent to the dislocated IOL was cut, but vitreous around the peripheral retina was left uncut so that risks of iatrogenic retinal break, bleeding and detachment were minimised.These all ensured much safer surgical procedures.Apart from managing IOL dislocation, other cases at the posterior pole, such as a lens nuclear fragment or cortex residue, can also be dealt with this technique.
Limitations should also be mentioned.Surgeons using this technique must be experienced in PPV surgery in case of unforeseen iatrogenic implications.The vitreous forceps should be used carefully because the gripping end of the forceps can easily injure the retina and vessels.Compared with the standard vitreoretinal forceps, an internal limiting membrane forceps is recommended due to its wider-open gripping end, which helps one to stably grasp the dislocated IOL.
In addition, the inclusion criteria should be stricter, especially for the condition of refracting media.We only suggest applying this technique in patients with mild vitreous opacity, such as eyes after vitrectomy and highly myopic eyes with moderate vitreous cortex liquefaction.Cases with cloudy refracting media of any type, such as corneal opacity, asteroid hyalosis or vitreous haemorrhage, are not inappropriate for this technique.Moreover, the microscope’s light will require adjustment.We attempted to find a fixed ratio between red reflex illumination and surrounding field illumination as well as a light intensity that was universally applicable under various conditions, but failed after several attempts.Therefore, to meet the needs of different surgeons for each distinct case, these two parameters should be adjusted for optimum depth perception and detail recognition.
Special concern for intraoperative and postoperative complications should be emphasized using this technique.Only the vitreous adherent to the dislocated IOL, but not those around the peripheral retina, were cut; additionally, the peripheral retina was carefully examined before finishing the surgery.Regular funduscopic examinations are necessary to screen for postoperative retinal break or detachment.With respect to the necessity of implanting new IOLs, no consensus has been reached.For patients with long axial length, we consider it improper to implant a new IOL; it would be a better option for these aphakic eyes to achieve CDVA with the help of frame glasses.