超声引导腰方肌阻滞联合全身麻醉对老年结直肠癌患者术后早期认知功能及应激的影响
2020-04-20牟俊英刘涛叶刚
牟俊英 刘涛 叶刚
[摘要] 目的 評价超声引导腰方肌阻滞(QLB)联合全身麻醉对老年结直肠癌患者术后早期认知功能及应激的影响。 方法 选择2018年7月~2019年7月恩施土家族苗族自治州中心医院行开腹结直肠癌手术的患者60例,依据随机数字表法将其分为超声引导QLB联合全身麻醉组(T组)和全身麻醉组(C组),每组30例。T组患者术前在超声引导下行双侧QLB,阻滞20 min后开始麻醉诱导;C组同法注射等量生理盐水。记录并比较两组入室10 min(T1)、麻醉诱导5 min(T2)、切皮后5 min(T3)、切皮后2 h(T4)及手术结束时(T5)平均动脉压(MAP)、心率(HR)、血糖(GLu)和C-反应蛋白(CRP)水平。记录并比较两组手术当晚8时及次日清晨6时BIS值,记录深睡眠时间(BIS<80)和有效睡眠指数(SEI)。记录并比较术后24、48 h视觉模拟评分(VAS),术后第1天、第3天认知功能障碍(POCD)例数,术后舒芬太尼用量及恶心呕吐例数。记录并比较术前1 d(Ta)、术后1 d(Tb)、术后3 d(Tc)及术后5 d(Td)简易智力状态量表(MMSE)及蒙特利尔认知评估量表(MoCA)评分。 结果 T组术后第1天POCD例数、恶心呕吐例数、术后舒芬太尼用量、术后24 h VAS评分低于C组,差异均有统计学意义(均P < 0.05);两组术后第3天POCD例数、术后48 h VAS评分比较,差异无统计学意义(P > 0.05)。T组术后当晚8时、次日清晨6时BIS值小于C组,SEI值大于C组,深睡眠时间长于C组,差异均有统计学意义(均P < 0.05)。T组Tb MMSE及MoCA评分低于C组,Tc MMSE评分低于C组,差异均有统计学意义(均P < 0.05)。T组T3~T5 MAP低于C组,T3、T5 HR低于C组,差异均有统计学意义(均P < 0.05)。T组T3~T5 Glu水平低于C组,T2 CRP水平低于C组,差异均有统计学意义(均P < 0.05)。 结论 QLB联合全身麻醉可减轻老年结直肠癌患者围术期应激反应,降低术后早期POCD的发生率。
[关键词] 腰方肌阻滞;早期认知功能;应激;老年患者
[中图分类号] R614.2 [文献标识码] A [文章编号] 1673-7210(2020)03(a)-0106-05
[Abstract] Objective To evaluate the effect of ultrasound-guided quadratus lumborum block (QLB) combined with general anesthesia on early postoperative cognitive function and stress response in elderly patients with colorectal cancer. Methods From July 2018 to July 2019, 60 cases with open colorectal cancer surgery in the Central Hospital of Enshi Tujia and Miao Autonomous Prefecture were collected. They were divided into ultrasound-guided QLB combined with general anesthesia group (group T) and general anesthesia group (group C) according to the radom number table method, with 30 cases in each group. Group T patients were guided by ultrasound to bilateral QLB before surgery, and anesthesia induction began after block for 20 min. Group C was injected with the same normal saline. Mean arterial pressure (MAP), heart rate (HR), blood glucose (Glu) and C-reaction protein (CRP) levels were recorded and compared at 10 min after the patient entered the operating room (T1), 5 min after anesthesia induction (T2), 5 min after incision (T3), 2 h after incision (T4), and at the end of surgery (T5). BIS was measured at 8 o′clock on the night of operation and 6 o′clock in the morning of the next day. Deep sleep time (BIS<80) and effective sleep index (SEI) were recorded and compared between the two groups. Visual analogue scores (VAS) 24 and 48 h after surgery, postoperative cognitive dysfunction (POCD) cases on the first and third day after surgery, dosages of Sufentanil and cases of nausea and vomiting were recorded and compared. Mini-mental state examination (MMSE) and montreal cognitive assessment scale (MoCA) were recorded and compared at preoperative 1 d (Ta), postoperative 1 d (Tb), postoperative 3 d (Tc) and postoperative 5 d (Td). Results The number of cases of POCD on the first day after surgery, nausea and vomiting, postoperative Sufentanil dosages and 24 h VAS scores after surgery in group T were lower than those in group C, with statistically significant differences (all P < 0.05). There were no significant differences between the two groups in the number of cases of POCD on the third day after surgery and 48 h VAS scores after surgery (P > 0.05). BIS values in group T were lower than those in group C at 8 o′clock in the evening and 6 o′clock in the morning of the next day and SEI values in group T were higher than those in group C, the deep sleep time was longer than that in group C, with statistically significant differences (all P < 0.05). Tb MMSE and MoCA scores in group T were lower than those in group C, and Tc MMSE scores were lower than those in group C, with statistically significant differences (all P < 0.05). T3-T5 MAP in group T were lower than those in group C, and T3, T5 HR were lower than those in group C, with statistically significant differences (all P < 0.05). The levels of T3-T5 Glu in group T were lower than those in group C, and the levels of T2 CRP were lower than those in group C, with statistically significant differences (all P < 0.05). Conclusion Ultrasound-guided QLB combined with general anesthesia can reduce perioperative stress response, and decrease the incidence of early POCD in elderly patients with colorectal cancer.
[Key words] Quadratus lumborum block; Early cognitive function; Stress response; Elderly patients
术后认知功能障碍(POCD)是老年患者术后常见并发症,发病率为12%~45%[1-3]。结直肠癌以老年患者居多,是POCD的高发人群,主要与围术期应激、术后疼痛、睡眠障碍等有关[4-5]。超声引导腰方肌阻滞(QLB)是在超声可视化技术的引导下在腰方肌周围注射局部麻醉药,通过胸腰筋膜扩散,产生区域阻滞与镇痛的效果,可有效緩解围术期应激反应及术后疼痛[6-7]。本研究旨在探讨超声引导QLB对老年结直肠癌患者术后疼痛、认知功能及应激的影响,为临床应用提供参考。
1 资料与方法
1.1 一般资料
选择2018年7月~2019年7月恩施土家族苗族自治州中心医院(以下简称“我院”)行全身麻醉下开腹结直肠癌手术患者60例。依据随机数字表法将其分为超声引导QLB联合全身麻醉组(T组)和全身麻醉组(C组),每组30例。两组患者性别、年龄、体重指数(BMI)、匹兹堡睡眠质量指数(PSQI)评分、受教育年限、美国麻醉医师协会(ASA)分级、肿瘤部位、TNM分期、高血压、糖尿病、麻醉时间、术中输液量等一般资料比较,差异无统计学意义(P > 0.05),具有可比性,见表1。本研究为前瞻性、双盲、随机对照临床研究,本研究经我院医学伦理委员会批准[2018伦审第(82)号]。
纳入标准:①年龄65~80岁;②ASA分级Ⅱ~Ⅲ级;③BMI 18~25 kg/m2;④病理确诊为结直肠癌且术前简易智力状态量表(MMSE)评分≥24分[8],蒙特利尔认知评估量表(MoCA)评分≥26分[8],PSQI评分≤6分[9];⑤所有患者及家属均签署知情同意书。排除标准:①行放化疗者;②伴有严重心肺肝肾等疾病者;③有精神系统疾病及认知功能障碍病史;④长期使用阿片类药物者;⑤局部麻醉药物过敏者;⑥凝血功能障碍者;⑦腰部皮肤破溃感染者。
1.2 方法
所有患者术前不给予镇静止痛药,采用静脉注射咪达唑仑(宜昌人福药业,生产批号:91F04021)0.05 mg/kg,舒芬太尼(宜昌人福药业,生产批号:91A07011)0.5 μg/kg,依托咪酯(江苏恩华药业,生产批号:20180425)0.3 mg/kg,顺式阿曲库铵(江苏恒瑞医药,生产批号:180622AK)0.2 mg/kg,全身麻醉诱导后经口气管插管。维持麻醉:术中靶向输注瑞芬太尼(宜昌人福药业,生产批号:90A07031),丙泊酚(四川国瑞药业,生产批号:1809082),间断静注顺式阿曲库铵。常规监测心率(HR)、血压(BP)和脉搏氧饱和度(SpO2),并维持术中HR、平均动脉压(MAP)波动不超过20%,呼气末二氧化碳分压为35~45 mmHg(1 mmHg=0.133 kPa),脑电双频指数(BIS)为40~60。两组患者术后均行舒芬太尼为主的静脉自控镇痛。
T组患者术前在M-Turbo超声(SonoSite公司,美国)引导下行双侧QLB,阻滞20 min后开始麻醉诱导。患者取侧卧位,将凸阵低频探头放置于髂峭上方水平,消毒铺巾后2%利多卡因(遂成药业,生产批号:31905201)局部浸润麻醉,22G、120 mm神经刺激针Stimuplex?誖 D Plus(B.BRAUN公司,日本)在探头后方经前内侧方向穿至腰方肌后侧,背阔肌深部的胸腰筋膜中层与后层深筋膜相延续处,回抽无血后将0.3%罗哌卡因(宜昌人福药业,生产批号:93B05031)25 mL注射于此处筋膜,同法行对侧QLB。C组同法注射等量生理盐水,所有操作由同1位具有丰富神经阻滞经验的麻醉主治医师实施,配药由另1位麻醉医师完成。
1.3 观察指标
①记录并比较两组入室10 min(T1)、麻醉诱导5 min(T2)、切皮后5 min(T3)、切皮后2 h(T4)及手术结束时(T5)的MAP、HR、血糖(Glu)及C-反应蛋白(CRP)水平。②记录并比较手术当晚8时及次日清晨6时BIS值,记录深睡眠时间(BIS<80)和有效睡眠指数(SEI)。SEI指深睡眠占夜间睡眠时间10 h的比例[10]。③记录并比较术后24、48 h视觉模拟评分(VAS),术后第1天、第3天POCD例数,术后舒芬太尼用量及恶心呕吐例数。④记录并比较术前1 d(Ta)、术后1 d(Tb)、术后3 d(Tc)及术后5 d(Td)随访,采用MMSE及MoCA量表评估认知功能。
1.4 统计学方法
采用SPSS 19.0统计学软件进行数据分析,计量资料数据用均数±标准差(x±s)表示,多组间比较采用单因素方差分析,组间两两比较采用LSD-t检验,两组间比较采用t检验;计数资料用率表示,组间比较采用χ2检验或Fisher精确概率法;等级资料采用秩和检验。以P < 0.05为差异有统计学意义。
2 结果
2.1 两组围术期相关指标比较
T组术后第1天POCD例数、恶心呕吐例数、术后舒芬太尼用量、术后24 h VAS评分低于C组,差异均有统计学意义(均P < 0.05);两组术后第3天POCD例数、术后48 h VAS评分比较,差异无统计学意义(P > 0.05)。见表2。
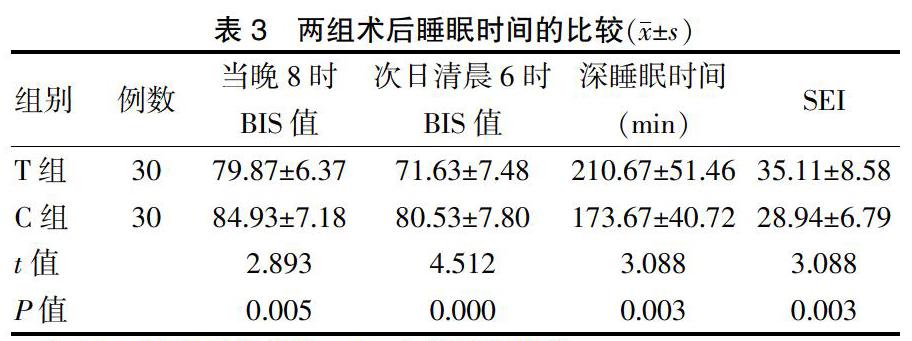
2.2 两组术后睡眠质量比较
T组术后当晚8时、次日清晨6时BIS值小于C组,SEI值大于C组,深睡眠时间长于C组,差异均有统计学意义(均P < 0.05)。见表3。
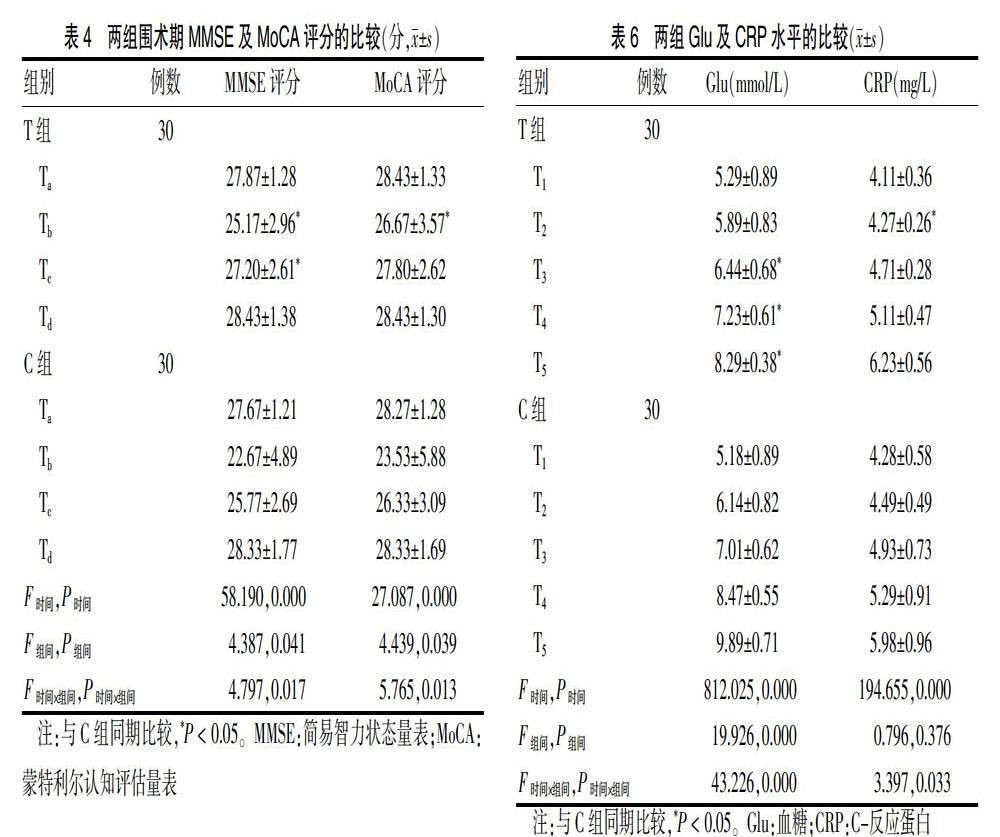
2.3 两组围术期MMSE及MoCA评分比较
两组围术期MMSE及MoCA评分比较时间效应、组间效应及时间×组间交互效应均有统计学意义(均P < 0.05)。T组Tb MMSE及MoCA评分低于C组,Tc MMSE评分低于C组,差异均有统计学意义(均P < 0.05)。见表4。
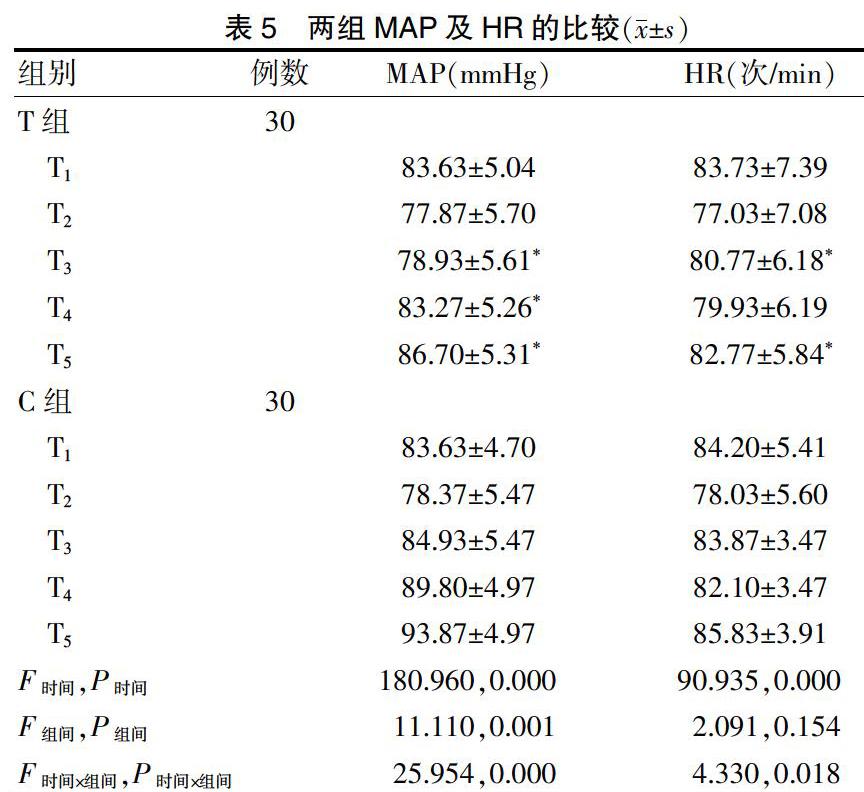
2.4 两组MAP及HR比较
两组MAP比较,时间效应、组间效应及时间×组间交互效应有统计学意义(P < 0.05);两组HR比较,时间效应及时间×组间交互效应有统计学意义(P < 0.05)。T组T3~T5 MAP水平低于C组,T3、T5 HR水平低于C组,差异均有统计学意义(均P < 0.05)。见表5。
2.5 两组Glu及CRP水平比较
两组Glu水平比较,时间效应、组间效应及时间×组间交互效应均有统计学意义(均P < 0.05);两组CRP水平比较,时间效应及时间×组间交互效应均有统计学意义(均P < 0.05)。T组T3~T5 Glu水平低于C组,T2 CRP水平低于C组,差异均有统计学意义(均P < 0.05)。见表6。
3 讨论
目前对于认知功能的评定并无统一标准,MMSE和MoCA评分是最为常用的认知功能筛查工具,但其评估效能会因受多种因素干扰使结果不一致[11],因此本研究将二者结合应用,更合理地筛查围术期POCD患者。研究显示[12],POCD的高发人群为65岁以上老年患者,故本研究选择65岁以上患者作为研究对象。本研究结果显示,术后第1天POCD发生率为28.33%;C组POCD发生率为40.00%,术后第3天仍有16.67%的POCD患者,而T组POCD发生率更低,提示QLB对于减少POCD的发生有一定积极作用。其作用机制可能是通过某些肽类分子阻止痛觉神经对免疫系统的激活,抑制炎性反应[13],促进海马神經元生成增加,提高空间认知能力[14-15]。
QLB是一种新的腹部躯干阻滞技术,阻滞平面可达T7-L1,且其药物在胸腰筋膜及椎旁间隙扩散,可阻滞此区域走行的交感神经[16],对内脏痛及腹壁切口痛均有效果,作用可持续术后24~48 h[17-18]。本研究结果显示,两组患者深睡眠时间、恶心呕吐、术后舒芬太尼用量、术后第1天VAS评分及POCD例数比较,差异有统计学意义(P < 0.05),但两组术后第3天VAS评分及POCD例数比较,差异无统计学意义(P > 0.05),提示QLB对减轻术后早期疼痛效果明显,可减少舒芬太尼用量[19],进一步减轻相关镇痛药物带来的恶心呕吐、呼吸抑制等副作用。睡眠对认知活动的影响可能有赖于睡眠中与记忆活动相关的神经元活动,一些睡前激活过的神经元可在睡眠中选择性地再次激活,进而增强人体的认知活动[20]。本研究结果显示,T组QLB后术后早期疼痛减轻,术后24 h深睡眠时间延长可能也在一定程度上增强了患者的认知功能。但因本研究术后随访时间短,对此类患者术后远期认知功能的评价还有待进一步研究。
血压波动过大是围术期老年患者死亡的高危因素[21],T组在全身麻醉前实施QLB干预后MAP、HR变化趋势更趋平稳,尤其血压波动减小,疼痛耐受性增强,对围术期安全有保护作用。Glu、CRP可有效反映围术期应激及急性炎性反应水平[22]。有报道称[23],腹横肌平面阻滞等神经阻滞方法可明显减少腹部手术患者的围术期应激。本研究显示,QLB后Glu的应激反应有所减轻;两组间CRP水平比较,变化无显著影响,可能是因为C组有注射生理盐水的应激情况,且手术本身对CRP亦有一定干扰,加之样本量较小、测量时间点较近,不一定真实反映了CRP的变化水平。以后应进一步扩大样本量,适当延长监测时间,并增加白细胞介素-6、皮质醇等指标的综合判定,以期进一步了解QLB对围术期应激的影响。
综上所述,QLB联合全身麻醉可减轻老年结直肠癌患者的术后疼痛,降低围术期应激反应,改善睡眠质量并有助于减少术后早期POCD。
[参考文献]
[1] Scott JE,Mathias JL,Kneebone AC. Postoperative cognitive dysfunction after total joint arthroplasty in the elderly:a meta-analysis [J]. J Arthroplasty,2014,29(2):261-267.
[2] 陈春茹,郑晋伟,孟波,等.腰丛神经阻滞对老年股骨上段手术患者脑氧代谢及术后认知功能的影响[J].浙江医学,2019,41(6):583-586.
[3] Needham MJ,Webb CE,Bryden DC. Postoperative cognitive dysfunction and dementia:what we need to know and do [J]. Br J Anaesth,2017,119(suppl_1):i115-i125.
[4] Plas M,Rotteveel E,Izaks GJ,et al. Cognitive decline after major oncological sugery in the elderly [J]. Eur J Cancer,2017,86:394-402.
[5] Zarbo C,Brivio M,Brugnera A,et al. Post-operative cognitive decline(POCD)after gynaecologic surgery:current opinions and future applications [J]. Arch Gynecol Obstet,2018,297(3):551-554.
[6] Akerman M,Pej N,Velikovi I. A Review of the Quadratus Lumborum Block and ERAS [J]. Front Med (Lausanne),2018,5:44.
[7] Ueshima H,Otake H,Lin JA. Ultrasound-Guided Quadratus Lumborum Block:An Updated Review of Anatomy and Techniques [J]. Biomed Res Int,2017,2017:2752876.
[8] Suda S,Muraga K,Ishiwata A,et al. Early Cognitive Assessment Following Acute Stroke:Feasibility and Comparison between Mini-Mental State Examination and Montreal Cognitive Assessment[J]. J Stroke Cerebrovasc Dis,2020,14:104688.
[9] Mollayeva T,Thurairajah P,Burton K,et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples:A systematic review and meta-analysis[J]. Sleep Med Rev,2016, 25:52-73.
[10] Boume RS,Mills GH,Minelli C. Melatonin therapy to improve noctumal sleep in critically ill patients:encouraging results from a small randomized controlled trial [J]. Crit Care,2008,12(2):R52.
[11] Bergeron D,Flynn K,Verret L,et al. Multicenter validation of an MMSE-MoCA conversion table [J]. J Am Geriatr Soc,2017,65(5):1067-1072.
[12] Scott DA,Evered L,Maruff P,et al. Cognitive function before and after left heart catheterization [J]. J Am Heart Assoc,2018,7(6):e008004.
[13] Liebert AD,Chow RT,Bicknell BT,et al. Neuroprotective Effects Against POCD by Photobiomodulation:Evidence from Assembly/Disassembly of the Cytoskeleton [J]. J Exp Neurosci,2016,10(1):1.
[14] Yang X,Shi Z,Li X,et al. Impacts of stellate ganglion block on plasma NF-κB and inflammatory factors of TBI patients [J]. Int J Clin Exp Med,2015,8(9):15630-15638.
[15] 王天海,朱红革,侯彦深,等.增强中枢胆碱能神经系统活性对小鼠术后认知障碍的影响[J].中国医药导报,2019, 16(18):17-20,41,182.
[16] Kumar A,Sadeghi N,Wahal C,et al. Quadratus lumborum spares paravenebral space in fresh cadaver injection [J]. Anesth Analg,2017,125(2):708-709.
[17] Kukreja P,MacBeth L,Sturdivant A,et al. Anterior quadratus lumborum block analgesia for total hip arthroplasty:a randomized,controlled study [J]. Reg Anesth Pain Med,2019,44(12):1075-1079.
[18] Murouchi T,Iwasaki S,Yamakage M. Quadratus lumborum block:Analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery [J]. Reg Anesth Pain Med,2016,41(2):146-150.
[19] Kukreja P,MacBeth L,Potter W,et al. Posterior quadratus lumborum block for primary total hip arthroplasty analgesia:a comparative study [J]. Einstein (S?觔o Paulo),2019,17(4):eAO4905.
[20] Zander T,Volz KG,Born J,et al. Sleep increases explicit solutions and reduces intuitive judements of semantic coherence [J]. Learn Mem,2017,24(12):641-645.
[21] 张京岚,叶清,孙建萍,等.老年人围手术期急性脑卒中危险因素分析[J].中华老年医学杂志,2009,28(3):213-216.
[22] Tong DC,Whitbourn R,Maclsaac A,et al. High-sensitivity c-reactive protein is a predictor of coronary microvascular dysfunction in patients with ischemic heart disease [J]. Front Cardiovasc Med,2018,12(4):81.
[23] 朱利君,俞玉龍,王钰,等.超声引导下腹直肌后鞘阻滞联合腹横肌阻滞对开腹结直肠癌术患者应激反应的影响[J].中华全科医学,2019,17(9):1515-1517.
(收稿日期:2019-10-12 本文编辑:刘明玉)
