小儿支气管哮喘血T、B淋巴细胞异常表达的临床意义
2017-08-07王成林
文 勃,王成林,罗 丽,冯 杨
(雅安市人民医院,四川 雅安 625000)
小儿支气管哮喘血T、B淋巴细胞异常表达的临床意义
文 勃,王成林,罗 丽,冯 杨
(雅安市人民医院,四川 雅安 625000)
目的 探讨小儿支气管哮喘血T、B淋巴细胞异常表达的临床意义。方法 选择2016年1至10月在雅安市人民医院就诊的哮喘患儿198例为研究对象(哮喘组),按照1:1配对,随机选取同期体检儿童为对照组;在哮喘组患儿中急性发作期107例,缓解期91例,对照组198例。检测哮喘急性发作、哮喘缓解和对照组儿童外周血的T淋巴细胞(CD3、CD3+CD4+、CD3+CD8+和CD4+/CD8+)、B淋巴细胞(CD19+CD23+),比较其相关指标的差异。结果 哮喘组急性发作期患儿的CD3+CD4+、CD19+CD23+分别明显高于哮喘缓解期(t值分别为2.479和2.341,均P<0.05)和对照组的患者(t值分别为2.421和2.524,均P<0.05);哮喘组急性发作期患儿的CD4+/CD8+明显高于哮喘缓解期的患儿和对照组,经比较均有显著性差异(t值分别为2.516和2.325,均P<0.05)。结论 支气管哮喘患儿外周血T、B淋巴细胞明显异常高表达,可作为支气管哮喘轻重程度及治疗效果的评价指标。
支气管哮喘;B淋巴细胞;T淋巴细胞;儿童;治疗效果
支气管哮喘(bronchial asthma,以下简称哮喘)是一种以慢性气道炎症和气道高反应性为特征的异质性疾病,多于儿童期发病。虽然在西方发达国家哮喘的发病率趋于稳定,但在发展中国家,其发病率呈逐年升高趋势,成为严重影响儿童生长发育的慢性疾病之一,给患儿家庭及社会带来了沉重的经济负担。细胞免疫的主要执行者为T淋巴细胞,体液免疫的主要执行者为B淋巴细胞,淋巴细胞的失衡与小儿支气管哮喘的发病密切相关[1-5]。T淋巴细胞和B淋巴细胞是否可作为小儿支气管哮喘严重程度的评判标准及治疗效果的随访指标有待研究。本资料对198例哮喘患儿和按1:1配对同期体检儿童的外周血T淋巴细胞(CD3、CD3+CD4+、CD3+CD8+和CD4+/CD8+)、B淋巴细胞(CD19+CD23+)进行检测分析,比较其相关指标的差异,为探讨外周血淋巴细胞相关指标在小儿哮喘患儿中的临床应用价值提供理论依据。
1对象与方法
1.1研究对象
收集2016年1至10月在雅安市人民医院就诊的哮喘患儿为研究对象(哮喘组),按照1:1配对,随机选取同期在本院体检的儿童为对照组。将符合支气管哮喘纳入标准的患儿,根据有无临床症状的急性发作分为急性发作期和缓解期。纳入标准:患儿年龄为1~14周岁,并符合儿童哮喘的临床诊断标准[6];排除标准:①年龄<1岁或者>14岁;②首次喘息发作;③近2周有糖皮质激素或免疫调节剂的使用史;④合并有其他免疫性疾病、心肺脑基础疾病等;⑤对照组儿童排除既往反复感染病史及喘息史,近2周有糖皮质激素或免疫调节剂的使用史,存在特应性体质及过敏性疾病家族史,存在心肺脑基础疾病和/或免疫疾病等基础疾病。
1.2标本采集
收集患儿的年龄、性别等基本信息,记录淋巴细胞亚群主要参数,包括T淋巴细胞(CD3、CD3+CD4+、CD3+CD8+和CD4+/CD8+)和B淋巴细胞(CD19+CD23+)及免疫球蛋白E(IgE)。采用MACSQuant八色流式细胞仪(德国)及贝克曼库尔特Gallios流式细胞仪(美国)对标本血进行淋巴细胞亚群检测。
1.3统计学方法

2结果
2.1研究对象的一般资料
本次共纳入符合标准的研究对象396例。哮喘组198例,其中急性发作期患儿107例,占54.04%,哮喘缓解期患儿91例,占45.96%;对照组198例,见表1。
2.2两组T淋巴细胞亚群的检测情况
哮喘组急性发作期患儿的CD3+CD4+和CD4+/CD8+均明显高于哮喘组缓解期患儿和对照组儿童,经比较有显著性差异(均P<0.05);哮喘组缓解期患儿的CD3+CD4+和CD4+/CD8+均高于对照组儿童,经比较有显著性差异(均P<0.05),见表2。

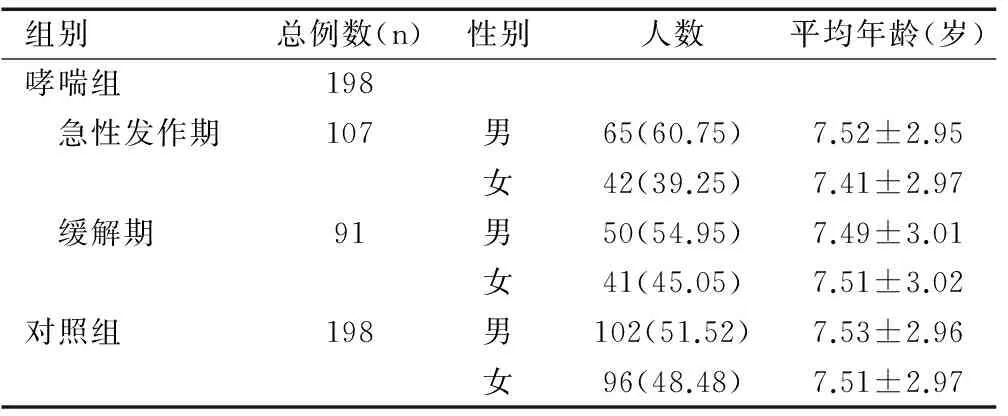
组别总例数(n)性别人数平均年龄(岁)哮喘组198 急性发作期107男65(60.75)7.52±2.95女42(39.25)7.41±2.97 缓解期91男50(54.95)7.49±3.01女41(45.05)7.51±3.02对照组198男102(51.52)7.53±2.96女96(48.48)7.51±2.97


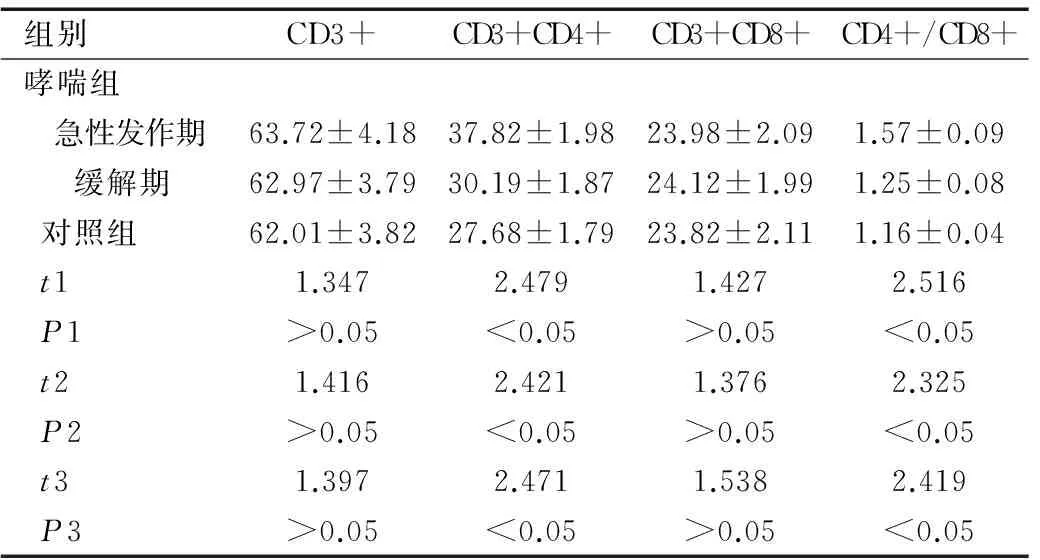
组别CD3+CD3+CD4+CD3+CD8+CD4+/CD8+哮喘组 急性发作期63.72±4.1837.82±1.9823.98±2.091.57±0.09 缓解期62.97±3.7930.19±1.8724.12±1.991.25±0.08对照组62.01±3.8227.68±1.7923.82±2.111.16±0.04t11.3472.4791.4272.516P1>0.05<0.05>0.05<0.05t21.4162.4211.3762.325P2>0.05<0.05>0.05<0.05t31.3972.4711.5382.419P3>0.05<0.05>0.05<0.05
注:t1和P1为哮喘组急性发作期与缓解期之间的比较;t2和P2为哮喘组急性发作期与对照组之间的比较;t3和P3为哮喘组缓解期与对照组之间的比较。
2.3两组B淋巴细胞和IgE的检测情况
哮喘组急性发作期患儿的CD19+CD23+明显高于哮喘组缓解期患儿和对照组儿童,经比较均有显著性差异(均P<0.05);哮喘组急性发作期患儿IgE明显高于哮喘组缓解期患儿和对照组儿童,经比较均有显著性差异(均P<0.05),见表3。

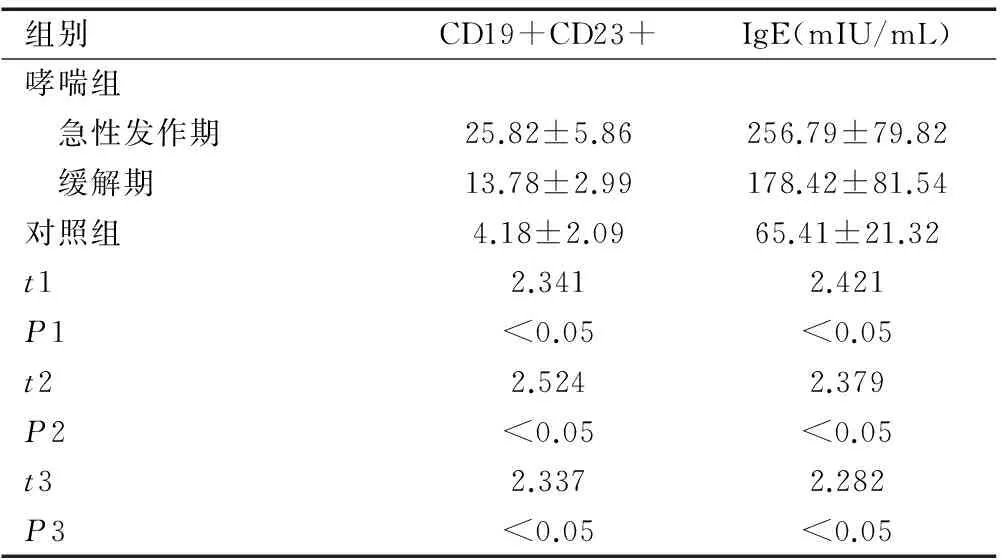
组别CD19+CD23+IgE(mIU/mL)哮喘组 急性发作期25.82±5.86256.79±79.82 缓解期13.78±2.99178.42±81.54对照组4.18±2.0965.41±21.32t12.3412.421P1<0.05<0.05t22.5242.379P2<0.05<0.05t32.3372.282P3<0.05<0.05
注:t1和P1为哮喘组急性发作期与缓解期之间的比较;t2和P2为哮喘组急性发作期与对照组之间的比较;t3和P3为哮喘组缓解期与对照组之间的比较。
3讨论
支气管哮喘被认为是遗传、环境、免疫病理机制共同参与的多基因遗传性疾病。支气管哮喘的具体发病机制尚未明确,但免疫机制在哮喘发生发展中的作用成为近年来的研究热点,以期为哮喘的诊断、治疗、控制提供新的方向。有研究显示体内细胞免疫失衡与哮喘发生、发展存在密切关系[7-11]。
3.1血清T淋巴细胞异常表达在小儿支气管哮喘中的临床意义
作为细胞免疫的主要功能执行者,T淋巴细胞受不同协同刺激信号影响,其中CD4/CD8比值平衡是维持机体免疫平衡的关键环节,机体在受到变应原刺激后,外周T细胞亚群含量会出现异常变化,速发性哮喘多见CD8+细胞水平下降,迟发性哮喘多见CD4+细胞水平增多[12-13]。本研究结果显示,哮喘组急性发作期患儿的CD3+CD4+和CD4+/CD8+均分别明显高于哮喘组缓解期患儿和对照组儿童(均P<0.05),说明患儿血清T淋巴细胞水平与患者疾病状态密切相关,可作为支气管哮喘轻重程度及治疗效果的评价指标。
3.2外周血B淋巴细胞异常表达在小儿支气管哮喘中的临床意义
体液免疫的主要执行者为B淋巴细胞。CD19和CD23分别是B淋巴细胞膜上的特征标志及IgE的低亲和力受体,其中CD23可介导细胞间的粘附,促进嗜碱性粒细胞释放组胺,调节IgE的合成和分泌,触发IgE介导炎症递质的释放和Ⅰ型变态反应的产生[14-16]。本研究中哮喘组急性发作期患儿的CD19+CD23+和IgE均明显高于哮喘组缓解期患儿和对照组儿童(均P<0.05),说明患儿血清B淋巴细胞水平及与IgE水平患者疾病状态密切相关,可作为支气管哮喘轻重程度及治疗效果的评价指标。
总之,支气管哮喘患儿外周血T、B淋巴细胞明显异常高表达,可作为支气管哮喘病情程度及治疗效果的评价指标。本研究的不足为样本量较小,更重要的结果还有待多中心、大样本的研究证实。
[1]Ishimori A, Harada N, Chiba A,etal.Circulating activated innate lymphoid cells and mucosal-associated invariant T cells are associated with airflow limitation in patients with asthma[J].Allergol Int,2017,66(2):302-309.
[2]Chu M, Chu I M, Yung E C,etal.Aberrant expression of novel cytokine IL-38 and regulatory T lymphocytes in childhood asthma[J].Molecules,2016,21(7):E933.
[3]Amin K.The role of the T lymphocytes and remodeling in asthma[J].Inflammation,2016,39(4):1475-1482.
[4]Raemdonck K, Baker K, Dale N,etal.CD4+ and CD8+ T cells play a central role in a HDM driven model of allergic asthma[J].Respir Res,2016,17:45.
[5]Zuska-Prot M, Ziókowski H, Jaroszewski J J,etal.Distribution of CD4+CD8+ double positive T cells in a mouse model of allergic asthma[J].Pol J Vet Sci,2016,19(1):217-219.
[6]中华医学会呼吸病学分会哮喘学组.支气管哮喘防治指南(2016年版)[J].中华结核和呼吸杂志,2016,39(9):675-697.
[7]Ling M F, Luster A D.Allergen-specific CD4(+) T cells in human asthma[J].Ann Am Thorac Soc,2016,Suppl 1:S25-S30.
[8]Troy N M, Hollams E M, Holt P G,etal.Differential gene network analysis for the identification of asthma-associated therapeutic targets in allergen-specific T-helper memory responses[J].BMC Med Genomics,2016,9:9.
[9]Yang S H, Yu C L, Yang Y H,etal.The immune-modulatory effects of a mixed herbal formula on dendritic cells and CD4+ T lymphocytes in the treatment of dust mite allergy asthma and perennial allergic rhinitis[J].J Asthma,2016,53(4):446-451.
[10]Schedel M, Jia Y, Michel S,etal. 1,25D3 prevents CD8(+)Tc2 skewing and asthma development through VDR binding changes to the Cyp11a1 promoter[J].Nat Commun,2016,7:10213.
[11]Wang W, Li P, Yang J.Decreased circulating interleukin-35 levels are related to interleukin-4-producing CD8+ T cells in patients with allergic asthma[J].Iran J Allergy Asthma Immunol,2015,14(4):379-385.
[12]Li X M, Peng J, Gu W,etal.TCDD-iInduced activation of Aryl hdrocarbon receptor inhibits Th17 polarization and regulates non-eosinophilic airway inflammation in asthma[J].PLoS One,2016,11(3):e0150551.
[13]Tao B, Ruan G, Wang D,etal.Imbalance of peripheral Th17 and regulatory T cells in children with allergic rhinitis and bronchial asthma[J].Iran J Allergy Asthma Immunol,2015,14(3):273-279.
[14]Haenen S, Vanoirbeek J A, De Vooght V,etal.Proteomic alterations in B lymphocytes of sensitized mice in a model of chemical-induced asthma[J].PLoS One,2015,10(9):e0138791.
[15]Kamekura R, Shigehara K, Miyajima S,etal.Alteration of circulating type 2 follicular helper T cells and regulatory B cells underlies the comorbid association of allergic rhinitis with bronchial asthma[J].Clin Immunol,2015,158(2):204-211.
[16]Hong G U, Lim J Y, Kim N G,etal.IgE and IgA produced by OX40-OX40L or CD40-CD40L interaction in B cells-mast cells re-activate FcεRI or FcαRI on mast cells in mouse allergic asthma[J].Eur J Pharmacol,2015,754:199-210.
[专业责任编辑:侯 伟]
Clinical significance of abnormal expressions of T and B lymphocytes in children with bronchial asthma
WEN Bo, WANG Cheng-lin, LUO Li, FENG Yang
(Ya’an People’s Hospital, Sichuan Ya’an 625000, China)
Objective To investigate the clinical significance of abnormal expressions of T and B lymphocytes in children with bronchial asthma. Methods Altogether 198 children with bronchial asthma treated in Ya’an People’s Hospital from January to October in 2016 were selected as study objects (asthma group), and healthy children receiving physical examination at the same time were randomly selected as control group according to 1:1 matching. In asthma group there were 107 cases in acute stage and 91 cases in remission stage, and 198 children were in the control group. T lymphocyte (CD3, CD3+CD4+, CD3+CD8+ and CD4+/CD8+) and B lymphocyte (CD19+CD23+) in peripheral blood of children in acute stage and in remission stage and of children in the control group were tested, and relative indexes were compared. Results Levels of CD3+CD4+ and CD19+CD23+ of cases in acute stage were significantly higher than those in remission stage (tvalue was 2.479 and 2.341, respectively, bothP<0.05) and those in the control group (tvalue was 2.421 and 2.524, respectively, bothP<0.05). Level of CD4+/CD8+ of cases in acute stage was significantly higher than that of cases in remission stage and in the control group, and the differences had statistic significance (tvalue was 2.516 and 2.325, respectively, bothP<0.05). Conclusion Expressions of T and B lymphocytes in peripheral blood of children with bronchial asthma are obviously high-expressed, which can be used as an index to evaluate the severity and therapeutic effect of bronchial asthma.
bronchial asthma; B lymphocytes; T lymphocytes; children; therapeutic effect
2016-11-08
文 勃(1980-),男,主治医师,主要从事儿科临床工作。
王成林,主任医师。
10.3969/j.issn.1673-5293.2017.06.014
R562.2
A
1673-5293(2017)06-0659-03
