原发性甲状腺淋巴瘤的临床和CT表现
2016-10-27周正荣
陈 红,周正荣
复旦大学附属肿瘤医院影像诊断科,复旦大学上海医学院肿瘤学系,上海 200032
原发性甲状腺淋巴瘤的临床和CT表现
陈红,周正荣
复旦大学附属肿瘤医院影像诊断科,复旦大学上海医学院肿瘤学系,上海 200032
背景与目的:原发性甲状腺淋巴瘤(primary thyroid lymphoma,PTL)较为少见,临床处理不同于甲状腺其他恶性肿瘤,因此,认识PTL具有重要意义。该研究旨在分析PTL的临床及CT表现。方法:收集22例经病理证实为PTL患者的临床和影像学资料,回顾性分析其临床症状,包括肿瘤的部位、大小、形态、边缘、CT密度及强化方式、与周围组织关系和颈部淋巴结情况。结果:22例患者中男性8例,女性14例,年龄范围39~77岁,平均年龄60岁。临床症状表现为短期内肿块迅速增大者12例。肿瘤累及双侧11例,累及单侧8例,同时累及右侧及峡部3例。肿瘤长径范围12~104 mm,短径范围11~71 mm。弥漫型、多发结节型和孤立结节型分别为12、5和5例。CT平扫15例低密度,7例等密度,肿瘤内部发现钙化0例,坏死5例。增强后19/22例轻中度强化,3/22例明显强化。CT增强均质密度13例,混杂密度9例。17例气管受压,5例食管受压,12例病灶突入前上纵隔内,8例颈部见肿大淋巴结。结论:老年女性颈部肿块迅速增大,CT表现为均质、低密度、轻中度强化、弥漫性肿大的实质性肿块,伴有邻近组织的压迫及侵犯,提示PTL可能。
甲状腺;原发性淋巴瘤;临床表现;CT
原发性甲状腺淋巴瘤(primary thyroid lymphoma,PTL)发病率较低,在甲状腺恶性肿瘤中所占比例小于5%,占结外淋巴瘤的比例小于2%[1-2],临床及影像科医师易误诊为甲状腺良性病变及其他恶性肿瘤。其发病机制尚不明确,治疗方法和预后有别于甲状腺其他恶性肿瘤,行手术切除对总生存期并无益处[3],手术仅用于病理活检及解除局部压迫,治疗主要以放疗及化疗为主。因此,影像对PTL准确而及时的诊断非常重要。超声对软组织有较高的分辨率可用于该病的检查,但对纵隔内及颈深部的病变显示困难,且病变整体及周围侵犯情况较难观察。叶智卫等[4]的研究结果表明,联合核医学甲状腺99mTc-MIBI显像和99mTcO4显像,可对甲状腺结节的良恶性进行判断和鉴别,但核素显像耗时长,试剂有放射性,部分人群不宜接受检查。但CT图像可以补充以上不足。本研究回顾性分析22例复旦大学附属肿瘤医院2009年5月—2015年12月经病理证实有完整临床、CT资料的PTL患者,分析总结其临床表现及CT征象,旨在提高对该病的认识,更好地为临床治疗提供导向。
1 资料和方法
1.1一般资料
回顾性分析本院2009年5月—2015年12月经病理证实的PTL患者22例,其中4例细针穿刺证实,5例空心针穿刺活检证实,13例手术病理证实。TL是指淋巴瘤浸润甲状腺或甲状腺及其区域淋巴结,而全身其他部位未见累及的淋巴瘤[5]。22例患者均行颈部、胸部和腹部CT,除外继发性淋巴瘤。结果显示22例均为PTL。
1.2影像学检查方法
22例患者均采用德国Siemens公司Sensation 64层螺旋CT常规检查,扫描范围从下颌角至主动脉弓水平。22例患者均行甲状腺平扫及增强检查。增强扫描采用非离子型对比剂碘海醇(购自上海博来科信谊药业有限责任公司,300 mg/mL)100 mL,注射速率为2.5~ 3.0 mL/s,注射对比剂后进行动脉期扫描,扫描层厚为5 mm,层距0。
1.3影像分析方法
由2名影像科主治医师对影像资料进行独立分析,如有异议进行商讨并达成共识。CT上按照病灶的形态及其与正常甲状腺的关系将病灶分为3种类型[6]:① 孤立结节型指单发结节,周围有正常甲状腺组织环绕;② 多发结节型指大于等于2个结节,结节边界可见;③ 弥漫型指一侧或两侧(包括或不包括峡部)正常甲状腺组织被弥漫性低密度病灶代替或仅存非常薄的高密度甲状腺组织。测量病变以病灶最大截面为准,多个结节测量最大结节的最大截面。强化度为平扫和增强CT值的差值。增强扫描病灶强化程度分级标准(CT值增加值):0~20 HU为轻度(不包含0 HU);21~40 HU为中度;40 HU以上为明显。2位影像医师测出的结果取平均值为最终数据。分析内容包括:① 病灶形态;② 病灶大小(长径mm×短径mm) ;③ 密度高低(与同侧胸锁乳突肌相比,分低、中、高);④ 增强扫描密度是否均匀;⑤ 病灶平扫及增强CT值、强化特点;⑥ 是否有囊变坏死及钙化;⑦ 边界是否清晰(清晰、不清晰);⑧ 区域内是否有淋巴结受累及是否伴有囊变、钙化(短径大于10 mm认为有淋巴结累及[7];⑨ 是否压迫或侵犯颈部血管、气管、食管等(肿瘤包绕上述器官超过一半或周围脂肪间隙消失为侵犯)[8];⑩ 是否有肌肉受累。
2 结 果
2.1一般临床及病理资料
22例患者的年龄、性别、主要症状、实验室检查和病理类型见表1。12例出现无痛性颈前肿块短期内(1~3个月)增大迅速,其中2例在服用甲状腺素后明显增大;10例自觉肿块缓慢性增大,无明显其他不适。
2.2CT表现
22例肿瘤的大小、累及范围、分型、平扫密度、强化程度、钙化、囊变及颈部淋巴结情况见表2。肿瘤长径范围12~104 mm,平均值为(53.73±22.22) mm,短径范围11~71 mm,平均值为(37.18±15.18) mm。长径大于50 mm的肿块中,弥漫型、多发结节型和孤立结节型分别为9、2和1例,长径小于50 mm的肿块各型分别为3、3和4例。12例病灶突入前上纵隔内。12例边缘见明显压缩变薄的甲状腺组织。CT值为30~55 HU,平均值为(41.5±6.52) HU。CT值为38~103 HU,平均值为(62.14±18.67) HU,强化程度为4~55 HU,平均值为(20.64±14.97) HU,总体呈轻中度强化。
17例气管受压,5例食管受包绕,12例病灶突入前上纵隔内,3例见颈部血管被包绕;甲状腺包膜不完整者5例,突破包膜侵犯周围组织。颈部见肿大淋巴结8例(36%),短径范围10~29 mm,其中纵隔淋巴结侵犯7例(32%)。所有的淋巴结均未见钙化及囊变,密度均匀,增强扫描轻度强化5/8例,呈中度3/8例(图1)。
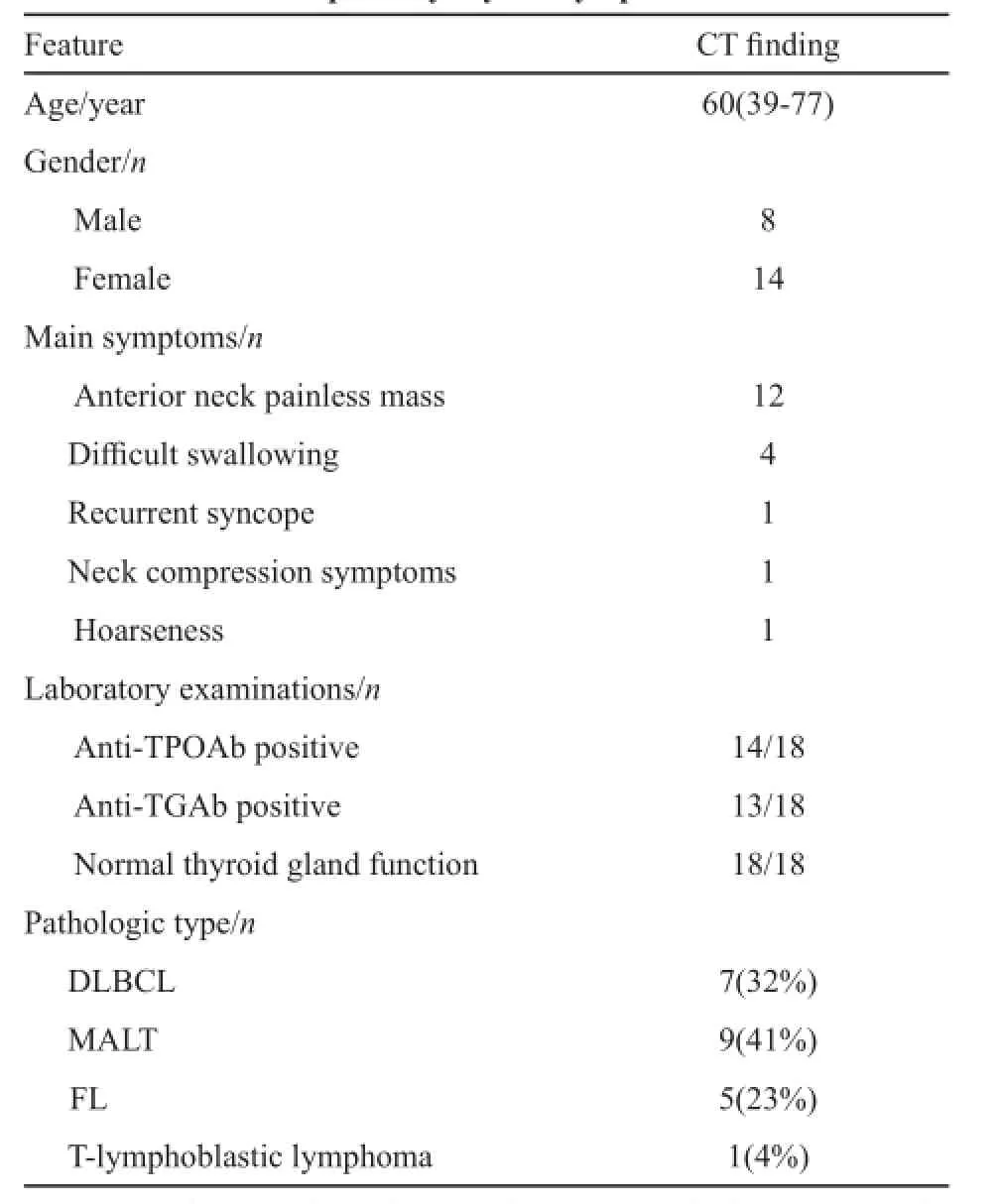
表 1 22例原发性甲状腺淋巴瘤的临床及病理学表现Tab. 1 Clinical and pathological fndings in twenty-two patients with primary thyroid lymphoma

图 1 PTL的影像学表现Fig. 1 Imaging features of PTLA, B: Axial CT scans of a 56-year-old female patient demonstrated that bilateral thyroid with low density, but slightly even enhancement in contrast-enhanced images enlarged difusely, tracheal and cervical vessels were compressed, esophagus got wrapped, and the tumor could not be separated from surrounding muscles; C, D: Axial CT scans of a 76-year-old male patient revealed that bilateral thyroid had isodensity with density decreasing difusely, trachea was pushed to the right side and esophagus got wrapped. Contrast-enhanced axial CT demonstrated the tumor had slight enhancement with well-defned margin, but esophagus and left common carotid artery got wrapped; E, F: Axial CT scans of a 56-year-old female patient demonstrated that the difuse enlargement of the bilateral thyroid had low and homogeneous density with well-defned margin. Multi-nodules and multinodular confuent tumors could be fgured resulting in thyroid gland compressed to a line (arrow), trachea was pushed to the right side and left cervical vessels were showed outside in contrast-enhanced axial CT; G, H: Axial plain CT images of a 62-year-old male patient demonstrated that the left lobe of thyroid gland enlarged with isodensity and the enlarging lymph nodes of Ⅳ region in the left cervical region (arrow) had a close relationship with the tumor. The mass and lymph nodes both had slight enhancement in contrast-enhanced axial CT
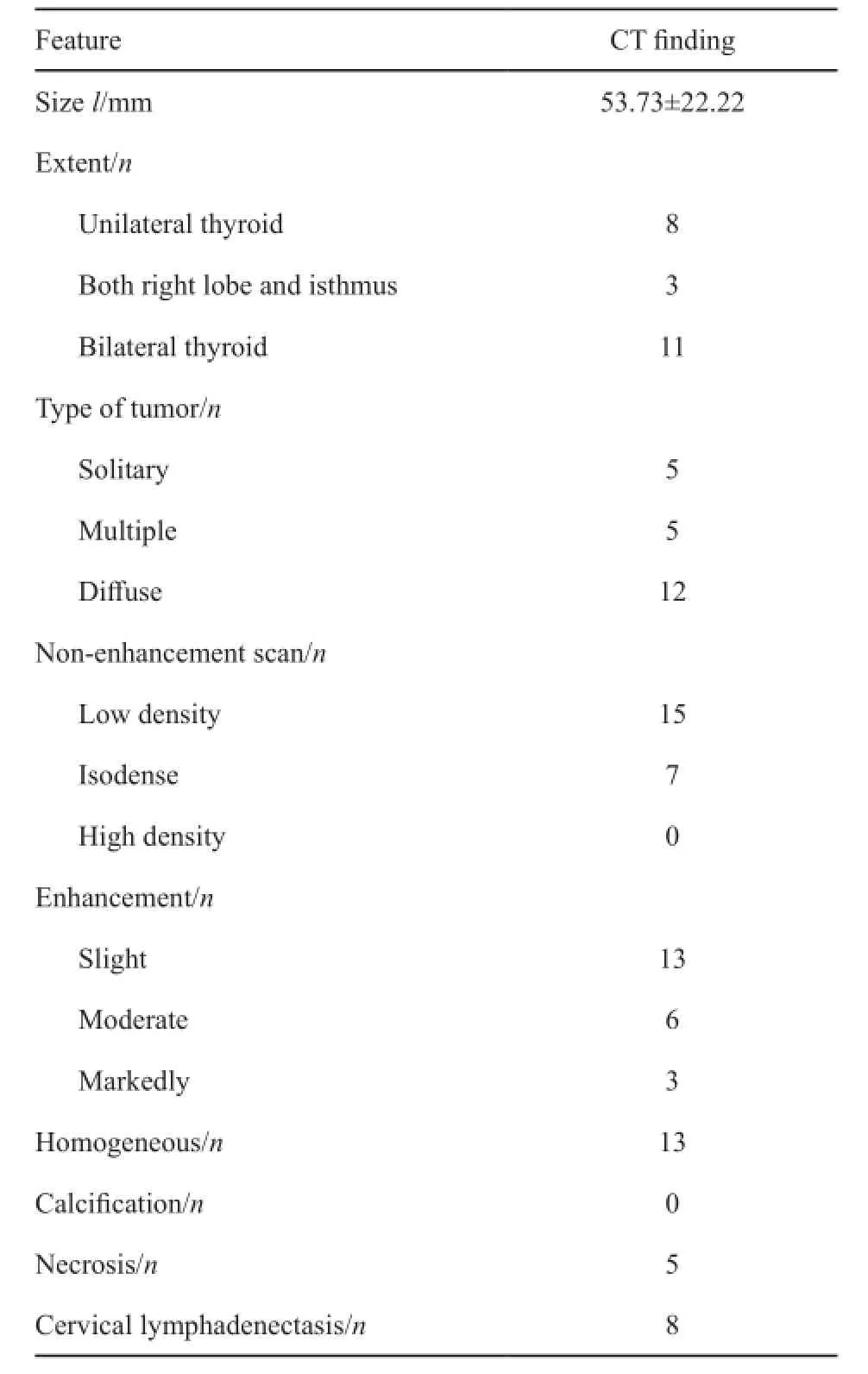
表 2 22例原发性甲状腺淋巴瘤的CT表现Tab. 2 CT fndings in twenty-two patients with primary thyroid lymphoma
3 讨 论
PTL好发于老年患者,女性比例略高于男性,临床表现为无痛性颈前肿块进行性增大或原有肿块的短期内迅速增大,肿块较大时常伴气管、食管的压迫,包绕颈部血管致呼吸不畅、吞咽困难和晕厥等,与文献报道相符[9-10]。有研究报道,PTL患者血清中抗甲状腺抗体均为阳性[11],本次研究结果与之相仿,而患者甲状腺功能均正常,提示PTL可能与自身免疫因素有关。多项研究结果显示,PTL常见的组织学亚型为弥漫大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL)及黏膜相关淋巴组织(mucosa-associated lymphoid tissue,MALT)淋巴瘤,且DLBCL比例略高,滤泡淋巴瘤较为少见,而本研究中MALT淋巴瘤(40%)多于DLBCL(31%),滤泡淋巴瘤比例(23%)相对较高,可能与患者数较少及地区差异有关,有待大样本数据分析[11-12]。
PTL可单侧和双侧发病,可同时累及峡部。肿瘤的最大径在13~75 mm,肿瘤形态多样,可为类圆形、椭圆形和不规则型,病灶长轴与甲状腺长轴一致,沿甲状腺轮廓塑形生长,类似于正常甲状腺形态的放大[13-14]。本组病变双侧发病多见,且多累及峡部,呈弥漫型,单侧及峡部亦有发病。肿瘤的长径范围较文献报道略大,原因可能是病灶长径最大的患者发病时间长(24个月),肿块生长缓慢,病理类型为侵袭性较低的MALT。肿瘤形态本组表现为结节型、多发结节型及弥漫型,肿块类型多与肿块大小相关,较大者多表现为弥漫型,而较小者多表现为结节型。从病灶大小及发病时间长短(结节型发病时间均小于6个月,多发结节及弥漫型为1~48个月)观察,结节型随着疾病进展有向其他病变转化的可能。PTL病灶平扫结果与文献报道[11-14]相似,多呈等或稍低密度,基本无钙化,无或少量囊变,但增强后多数病灶呈轻中度均匀强化,而出现不均匀强化少见。病灶内的低密度灶可能是坏死所致,本组坏死少见,可能与本组病理以侵袭性较低的病理类型为主有关。盛二燕等[15]认为,只要发现甲状腺结节内有钙化存在,虽不能盲目判断其恶性,但应引起高度警惕。而本病虽为恶性,但基本无钙化,也需要引起注意。有报道认为,无周围组织侵犯是PTL特点之一[1],但多数学者认为PTL可出现周围组织侵犯,但发生率较低[13,16]。本组研究发现相当部分肿块压迫正常甲状腺组织、气管及颈部血管,突入纵隔内,大部分病灶边界清楚,仅少部分患者出现食管侵犯及颈部血管包绕,可能与淋巴瘤质软、侵袭性低有关[1]。本组患者纵隔淋巴结侵犯(32%)稍高于文献报道(8%~29%[17]),肿大淋巴结密度均匀,均未见钙化及囊变,较其他研究相仿[17]。
PTL需与甲状腺癌、桥本甲状腺炎、慢性淋巴细胞性甲状腺炎及甲状腺腺瘤等相鉴别。甲状腺癌多为年轻女性,明显低于PTL的平均发病年龄,甲状腺癌体积较PTL小[9,17-18],增强中度等强化,内部密度更为混杂,内多见钙化、坏死,周围淋巴结易出现钙化、囊变,肿瘤边界多不规整,边界不清。弥漫型PTL与桥本甲状腺炎、慢性淋巴细胞性甲状腺炎较难鉴别,均表现为弥漫的密度欠均匀的低密度改变,但桥本甲状腺炎及慢性淋巴细胞性甲状腺炎较少颈部出现淋巴结肿大。蔡丽萍等[19]认为,彩色多普勒超声对桥本甲状腺炎诊断正确率高,且方便,可作为桥本甲状腺炎影像学检查的首选方法。结节型PTL因密度多均匀,边界清楚,易误认为良性病变,CT增强腺瘤强化较PTL明显,部分腺瘤易出现甲状腺功能异常,对鉴别有一定提示作用。
本研究样本量较少,无法做统计学分析,回顾性研究易出现主观性偏倚。仅重点分析了PTL的CT表现,未能结合超声等其他影像学对疾病予以评估,观察不够全面,但本研究会让读者对PTL的CT特征有更进一步的认识。
综上所述,PTL好发于老年女性患者,临床症状多表现为无痛性颈前肿块,短期内可进行性增大,部分有压迫症状。如CT扫描出现甲状腺较大等低密度肿块,多呈双侧弥漫性或结节性均匀增大,增强均匀轻中度强化,条状甲状腺组织及周围组织压迫,伴周围轻中度均匀强化的肿大淋巴结,要高度警惕PTL的可能,积极行甲状腺活检并结合免疫组织化学,尽早做出正确诊断,制定有利于患者的治疗方案。
[1] PEDERSEN R K, PEDERSEN N T. Primary non-Hodgkin's lymphoma of the thyroid gland: a population based study[J]. Histopathology, 1996, 28(1): 25-32.
[2] STEIN S A, WARTOFSKY L. Primary thyroid lymphoma: a clinical review[J]. J Clin Endocrinol Metab, 2013, 98(8):3131-3138.
[3] MEYER-ROCHOW G Y, SYWAK M S, REEVE T S, et al. Surgical trends in the management of thyroid lymphoma[J]. Eur J Surg Oncol, 2008, 34(5): 576-580.
[4] 叶智卫, 刘菁华, 高克加, 等. 联合99mTc-MIBI与99mTcO4显像鉴别甲状腺结节的临床价值[J]. 肿瘤影像学, 2014, 23(3): 212-215.
[5] PASIEKA J L. Hasbimoto's disease and thyroid lymphoma:role of the surgeon[J]. World J Surg, 2000, 24(8): 966-970.
[6] KIM H C, HAN M H, KIM K H, et al. Primary thyroid lymphoma: CT findings[J]. Eur J Radiol, 2003, 46(3): 233-239.
[7] SUMI M, OHKI M, NAKAMURA T. Comparison of sonography and CT for differentiating benign from malignant cervical lymph nodes in patients with squamous cell carcinoma of the head and neck[J]. AJR Am J Roentgenol, 2001, 176(4):1019-1024.
[8] TAKASHIMA S, MORIMOTO S, IKEZOE J, et al. CT evaluation of anaplastic thyroid carcinoma[J]. AJR Am J Roentgenol, 1990, 154(5): 1079-1085.
[9] MA B, JIA Y, WANG Q, et al. Ultrasound of primary thyroid non-Hodgkin's lymphoma[J]. Clin Imaging, 2014, 38(5):621-626.
[10] GRAFF-BAKER A, ROMAN S A, THOMAS D C, et al. Prognosis of primary thyroid lymphoma: demographic, clinical, and pathologic predictors of survival in 1 408 cases[J]. Surgery, 2009, 146(6): 1105-1115.
[11] LI X B, YE Z X. Primary thyroid lymphoma: multi-slice computed tomography findings [J]. Asian Pac J Cancer Prev, 2015, 16 (3): 1135-1138.
[12] HWANG Y C, KIM T Y, KIM W B, et al. Clinical characteristics of primary thyroid lymphoma in Koreans[J]. Endocrinol J, 2009, 56(3): 399-405.
[13] 江明祥, 邵国良, 陈 波.原发性甲状腺淋巴瘤的CT表现分析[J]. 影像诊断与介入放射学, 2014, 23(2):151-155.
[14] 关玉宝, 周良平, 曾庆思, 等. 原发性甲状腺恶性淋巴瘤的CT 表现[J]. 临床放射学杂志, 2006, 25(6): 515-517.
[15] 盛二燕, 彭卫军. 甲状腺良恶性病变的CT表现与病理对照分析[J]. 肿瘤影像学, 2014, 23(4): 329-322.
[16] TAKASHIMA S, IKEZOE J, MORIMOTO S, et al. Primary thyroid lymphoma: evaluation with CT[J]. Radiology, 1988, 168(3): 765-768.
[17] BELAL A A, ALLAM A, KANDIL A, et al. Primary thyroid lymphoma: a retrospective analysis of prognostic factors and treatment outcome for localized intermediate and high grade lymphoma[J]. Am J Clin Oncol, 2001, 24(3): 299-305.
[18] MANE M, O'NEILL A C, TIRUMANI S H, et al. Thyroid lymphoma on a background of Hashimoto's thyroiditis: PET/ CT appearances[J]. Clin Imaging, 2014, 38(6): 864-867.
[19] 蔡丽萍, 孙燕双, 刘泽红, 等. 桥本甲状腺炎的超声表现与细针穿刺细胞学检查对照[J].肿瘤影像学, 2014, 23(3):288-230.
Clinical and CT imaging features of primary thyroid lymphoma
CHEN Hong, ZHOU Zhengrong(Department of Radiology, Fudan University Shanghai Cancer Center; Department of Oncology, Shanghai Medical College, Fudan University, Shanghai 200032, China)
ZHOU Zhengrong E-mail: zhouzr-16@163.com
Background and purpose: Primary thyroid lymphoma (PTL) is uncommon in clinic with quite diferent treatment from that of other malignant thyroid tumors. Therefore, to achieve complete understanding of PTL has crucial signifcance. This study aimed to investigate the clinical and computed tomography (CT) characteristics of PTL. Methods: The clinical and imaging data from 22 patients with PTLs confrmed by pathology were collected. The clinical symptoms of patients, the site, size, shape, margin, CT value and enhancement pattern, relation with surrounding tissues of PTLs and cervical lymph nodes were summarized retrospectively. Results: All the 22 patients including 8 males and 14 females had an average age of 60 years (range: 39-77 years). Twelve PTLs rapidly progressed in short term and the rest expanded slowly. The tumors involved bilateral thyroid in 11 cases, unilateral thyroid in 8 cases and both right lobe and isthmus in the remaining 3 cases. The long and short ranges were (12-104) mm and (11-71) mm. The solitary, multiple and difuse nodules distributed in 5, 5 and 12 patients, respectively. In axial plain CT scans, low density appeared in 15 patients, isodensity in 7 patients, calcifcation inside the lesion in 0 patient, and necrosis in 5 patients. Nineteen PTLs manifested slight or moderate enhancement, and 3 marked enhancement in contrast-enhanced axial CT images. Homogeneous density and mixed density were demonstrated in 13 and 9 cases, respectively. Trachea and esophagus was pushed in 17 and 5 cases, tumors were involved into superior mediastinum in 12 cases and enlarged lymph nodes were demonstrated in 8 cases. Conclusion: If a solid thyroidal mass in an old female patient rapidly progresses in short term and CT scans show homogeneous and low density, slight or moderate enhancement, and difusive swelling with compression and invasion of surrounding tissues, it has a high possibility of PTL.
Thyroid; Primary lymphoma; Clinical features; Tomography, X-ray computed
10.19401/j.cnki.1007-3639.2016.09.011
R736.1
A
1007-3639(2016)09-0790-05
2016-03-05
2016-04-19)
周正荣 E-mail: zhouzr-16@163.com