Serum IL-1βand IL-18 correlate with ESR and CRP in m ultid rug-resistant tuberculosis patients
2015-02-14YanliWang,ChunmeiHu,ZailiangWang等
Serum IL-1βand IL-18 correlate with ESR and CRP in m ultid rug-resistant tuberculosis patients
Dear Editor:
The emergence of multidrug-resistant tuberculosis (MDR-TB)is bringing new challenges.MDR-TB is caused by Mycobacterium tuberculosis(M.tuberculosis) that is resistant to isoniazid and rifampicin,with or without resistance to other anti-tuberculosis drugs. Approximately 450,000 people developed MDR-TB worldwide in 2012 and an estimated 170,000 people died from the disease[1].Bacterial burden is not strictly correlated with disease progression,and several hallmarks of severe tuberculosis suggest that insufficiently controlled inflammation plays an important role in pathogenesis[2]. It has been reported that nucleotide-binding and oligomerization domain(NOD)like receptor 3(NLRP3)inflammasome and its cytokines IL-1β and IL-18 play a critical role in host defense and immunopathologic process in chronic M.tuberculosis infection in vitro and in animal models[3-5].However,little is known about the role of NLRP3 inflammasome and IL-1β and IL-18 in MDRTB patients.We determined serum IL-1β and IL-18 contents in drug-susceptible tuberculosis(DS-TB)and MDR-TB patients and investigated their relationships with disease severity in tuberculosis.
Written informed consent was obtained from all study participants,and the study was approved by the Research Ethics Committee of Nanjing Medical University(Nanjing,China).TB patients were recruited from Nanjing Thoracic Hospital from January to December 2014 as a subset of a multi-center study.
The baseline characteristics of 30 healthy control subjects,35 DS-TB patients,and 30 MDR-TB patients are summarized inTable 1.MDR-TB patients had more severe radiographic features than DS-TB patients (P=0.01).Serum ESR and CRP levels were significantly higher in TB patients than in healthy controls, and in MDR-TB patients than in DS-TB patients.
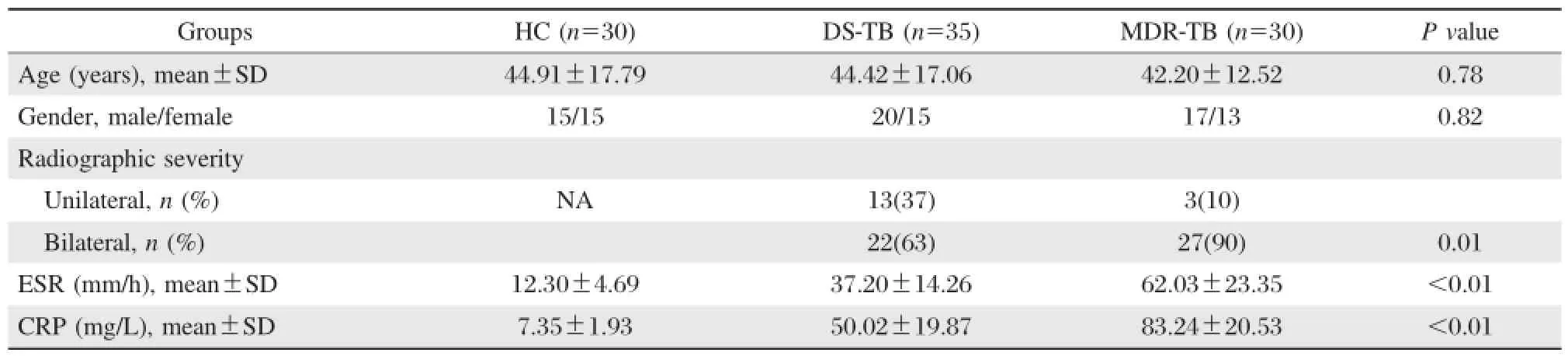
Table 1 Baseline characteristics of the study subjects
ELISA showed(Fig.1A)that the levels of IL-1β in MDR-TB(7.48±3.58)were significantly higher than that in DS-TB patients(3.07±2.26).Meanwhile,serum IL-18 displayed the same trend,which was higher in MDR-TB patients(131.03±94.92)than DS-TB patients (94.28±57.10)and healthy controls(61.66±24.78) (Fig.1B).To investigate whether serum IL-1β and IL-18 are related to radiographic severity,we stratified TB patients according to unilateral and bilateral lesions.In DS-TB patients,IL-1β(Fig.1C)and IL-18(Fig.1D) were significantly higher in patients with bilateral lesionsubgroup than patients with unilateral lesion.No differences were observed in IL-1β or IL-18 between MDRTB patients with bilateral and unilateral lesion.Then, we analyzed the relationships between IL-1β/IL-18 and ESR/CRP.As shown inTable 2,there was no obvious correlation between IL-1β/IL-18 and ESR/CRPin healthy controls.However,both in DS-TB and MDR-TB patients, IL-1β positively correlated with ESR and CRP,and IL-18 also positively correlated with ESR and CRP.
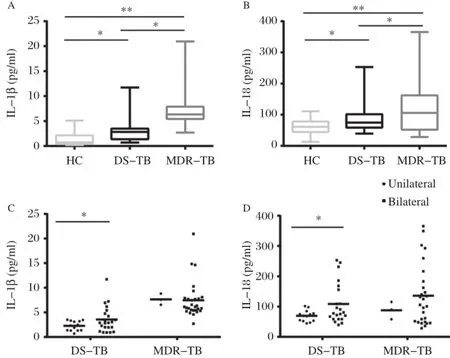
Fig 1.Serum IL-1β and IL-18 levels in tuberculosis patients and healthy controls.A:The levels of serum IL-1β was significant higher in TB patients than in healthy controls,and serum IL-1β was higher in MDR-TB than in DS-TB.B:The levels of serum IL-18 was highest in MDR-TB patients,and serum IL-18 was higher in DS-TB patients than in healthy controls.C:In DS-TB patients,the levels of IL-1β and IL-18 were significant higher in patients with bilateral lesion than those in patients with unilateral lesion.D:In MDR-TB patients,the differences of IL-1β or IL-18 between patients with bilateral lesion and unilateral lesion are not statistically significant.*P<0.05,**P<0.01.DS-TB:drug susceptible tuberculosis;MRDTB:multi drug-resistant tuberculosis.
Mounting evidence shows that NLRP3 inflammasome can be activated by M.tuberculosis in host immune cells.Our results showed that the circulating levels of NLRP3 inflammasome-mediated IL-1β and IL-18 in sera of pulmonary tuberculosis patients,especially in MDR-TB patients,are higher than those in healthy controls and positively correlate with radiographic severity and ESR and CRP.We observed that serum IL-1β is higher in pulmonary tuberculosis patients, especially in MDR-TB patients,than that in healthy controls.The concept that exuberant IL-1β responses are causatively associated with TB progression immunopathology and poor treatment outcome in humans[7]has been receiving more attention.It is reported that higher IL-1β did not suppress the activity of IFN-γ-producing T cells,but correlated with neutrophil accumulation in the lung[7].It is also documented that high-IL-1β expressing genotype was associated with the severity of pulmonary disease[7]which is in accordance with our results.
In our study,IL-18 is also higher in MDR-TB than in DS-TB patients and healthy controls,which corroborates with previously published literatures that IL-18 concentration is significantly increased in TB patients with severe disease[8].
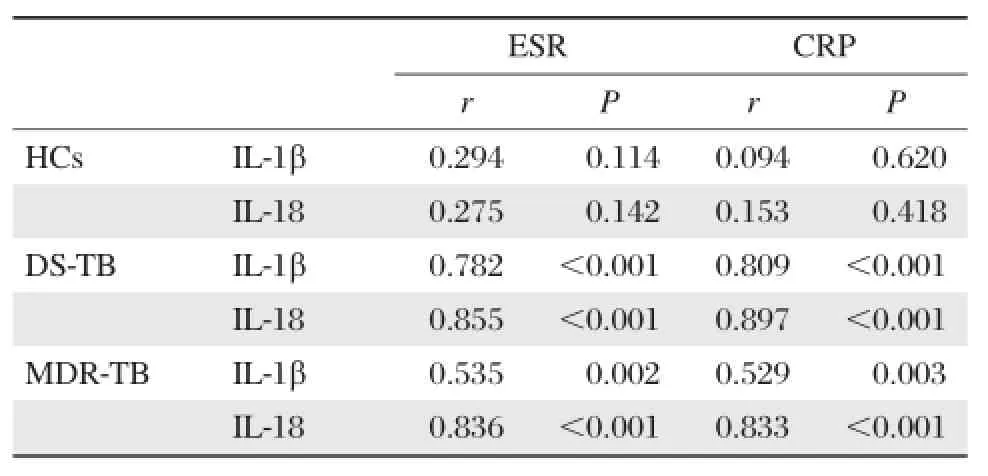
Table 2 Correlations between IL-1β,IL-18 and ESR,CRP
Our results showed that serum IL-1β and IL-18 levels positively correlated with radiographic severity in DS-TB patients.However,in MDR-TB patients,the differences of IL-1β or IL-18 between patients with bilateral lesion and unilateral lesion were not statistically significant.We considered that it was due to that there were only 3 patients with unilateral lesion in MDR-TB group.
Raised ESR and CRP are indicative of infection and have been shown to be increased in TB patients.The plasma levels of ESR and CRP reflect the intensity of the pathological process[6].In our present study,serum IL-1β and IL-18 levels are positively correlated to ESR and CRP in both DS-TB and MDR-TB patients.It suggests that IL-1β and IL-18 are involved in the immunopathologic progression in tuberculosis.
To our knowledge,this is the first study to examine the relationship between inflammasome-associated cytokines and disease severity markers in pulmonary tuberculosis,especially in MDR-TB patients.Our results demonstrate that elevated levels of serum IL-1β and IL-18 are positively correlated to disease severity.IL-1β and IL-18 may be promising therapeutic targets for adjuvant treatment of MDR-TB.
Yours Sincerely,
Yanli Wang,Chunmei Hu,Zailiang Wang,Hui Kong, Weiping Xie,Hong Wang✉
Department of Respiratory Medicine, The First Affiliated Hospital of Nanjing Medical University, Nanjing,Jiangsu 210029, China.
✉Corresponding author:Tel:+86-25-68136426,Fax: +86-25-68136269
E-mail:hongwang@njmu.edu.cn
[1] Pedro HdSP,Nardi SMT,Pereira MIF,et al.Clinical and epidemiological profiles of individuals with drug-resistant tuberculosis[J].Mem Inst Oswaldo Cruz,2015,110(2):235-248.
[2] Mishra BB,Rathinam VA,Martens GW,et al.Nitric oxide controls the immunopathology of tuberculosis by inhibiting NLRP3 inflammasome-dependent processing of IL-1beta[J].Nat Immunol,2013,14(1):52-60.
[3] Wong KW,Jacobs WR Jr.Critical role for NLRP3 in necrotic death triggered by Mycobacterium tuberculosis[J].Cell Microbiol,2011,13(9):1371-1384.
[4] Carlsson F,Kim J,Dumitru C,et al.Host-detrimental role of Esx-1-mediated inflammasome activation in mycobacterial infection[J].PLoS Pathog,2010,6(5):e1000895.
[5] Abdalla H,Srinivasan L,Shah S,et al.Mycobacterium tuberculosis infection of dendritic cells leads to partially caspase-1/11-independent IL-1beta and IL-18 secretion but not to pyroptosis[J].PLoS One,2012,7(7):e40722.
[6] Beatriz Lima Alezio Muller,Daniela Maria de Paula Ramalho,Paula Fernanda Goncalves dos Santos,et al. Inflammatory and immunogenetic markers in correlation with pulmonary tuberculosis[J].J Bras Pneumol,2013, 39(16):719-727.
[7] Zhang G,Zhou B,Li S,et al.Allele-specific induction of IL-1beta expression by C/EBPbeta and PU.1 contributes to increased tuberculosis susceptibility[J].PLoS Pathog, 2014,10(10):e1004426. [8] SantucciN,D’Attilio L,Besedovsky H,et al.A clinical correlate of the dysregulated immunoendocrine response in human tuberculosis[J].Neuroimmunomodulation,2010,17(3):184-187.

Received 05 May 2015,Revised 15 May 2015,Accepted 06 June 2015, Epub 20 July 2015
R183.3,Document code:B
The authors reported no conflict of interests.
©2015 by the Journal of Biomedical Research.All rights reserved.
10.7555/JBR.29.20150077
杂志排行
THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Internal radiation therapy:a neglected aspect of nuclear medicine in the molecular era
- Hypercholesterolemia,low density lipoprotein receptor and proprotein convertase subtilisin/kexin-type 9
- Endothelin-1-induced mini-stroke in the dorsal hippocampus or lateral amygdala results in deficits in learning and memory
- Netrin-1 overexpression in bone marrow mesenchymal stem cells promotes functional recovery in a rat model of peripheral nerve injury
- Acute effect of aspartame-induced oxidative stress in Wistar albino rat brain
- Differential mRNA expression profiling of oral squamous cell carcinoma by high-throughput RNA sequencing
