妊娠期糖尿病患者的糖化血红蛋白水平和体重指数对妊娠结局的影响
2019-04-23洪小恒邝小玲周燕林小磊林姗姗
洪小恒 邝小玲 周燕 林小磊 林姗姗
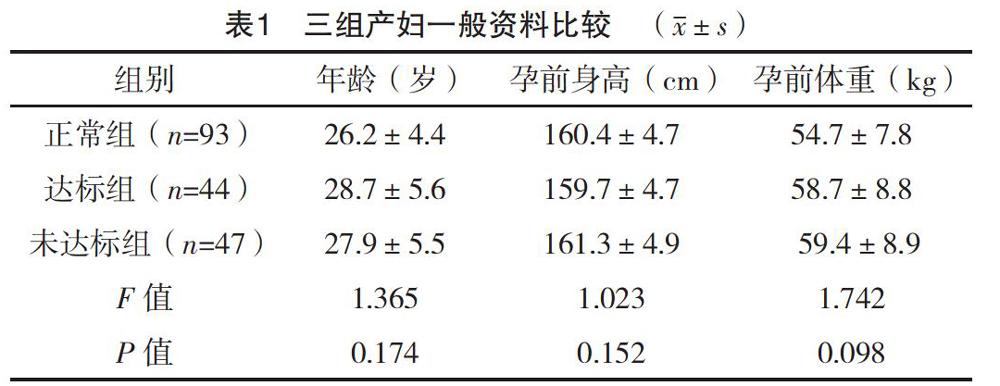
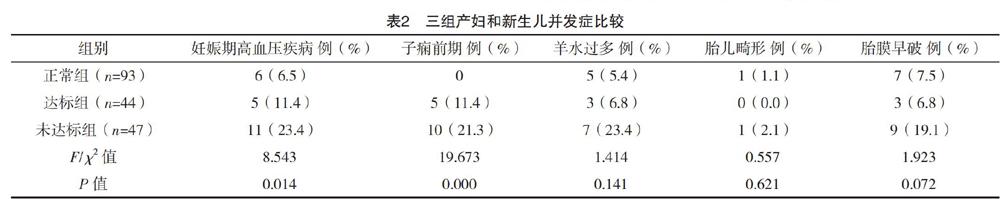
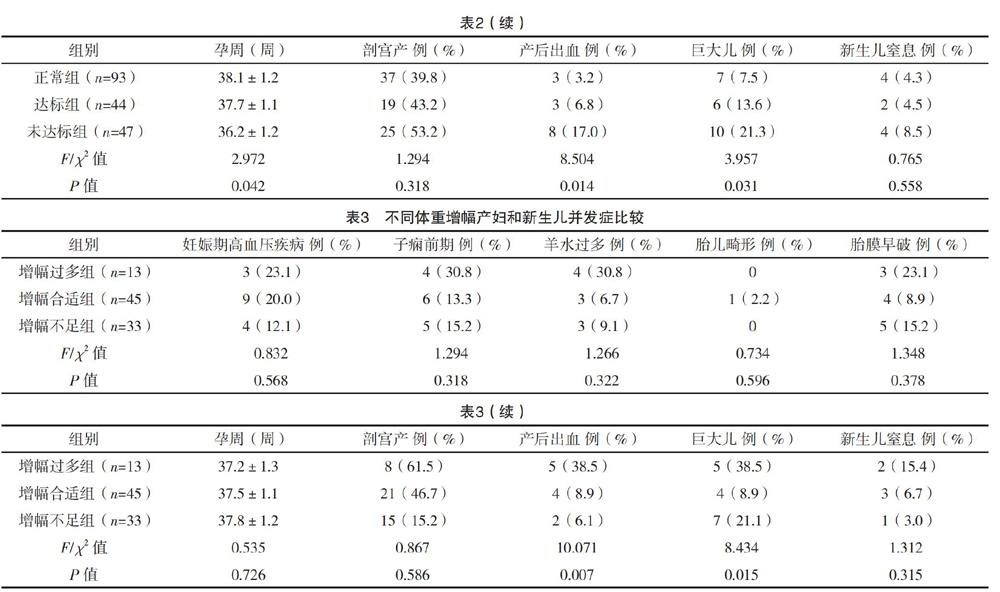
【摘要】 目的:探討产妇在孕期的糖化血红蛋白水平及孕期体重增幅对妊娠期糖尿病患者孕期及产后、胎儿及新生儿的并发症影响。方法:选取2013年1月-2015年12月在笔者所在医院产检及分娩的184例产妇纳入研究。根据妊娠期糖尿病诊断标准将产妇分为正常组93例和妊娠期糖尿病组91例,妊娠期糖尿病产妇再根据分娩前糖化血红蛋白水平分为达标组44例和未达标组47例;根据不同增重标准将91例GDM产妇分为三组,增幅过多组13例、增幅合适组45例和增幅不足组33例。比较不同糖化血红蛋白水平的产妇和不同孕期体重增幅的妊娠期糖尿病产妇妊娠并发症和结局,以探讨糖化血红蛋白水平及孕期体重增幅对妊娠期糖尿病患者孕期及产后和胎儿及新生儿的并发症影响。结果:未达标组妊娠期高血压疾病、子痫前期、产妇产后出血和巨大儿发生率均高于达标组和正常组,胎儿出生时孕周数均短于达标组和正常组,差异均有统计学意义(P<0.05);达标组妊娠期高血压疾病、子痫前期、产妇产后出血和巨大儿发生率高于正常组,差异有统计学意义(P<0.05);三组羊水过多、胎儿畸形、胎膜早破、剖宫产及新生儿窒息发生率比较差异无统计学意义(P>0.05)。体重增幅过多产妇产后出血和巨大儿发生率均高于增幅正常和增幅不足产妇,差异均有统计学意义(P<0.05);不同体重增幅产妇妊娠期高血压疾病、子痫前期、羊水过多、胎儿畸形、胎膜早破、胎儿出生时孕周数、剖宫产及新生儿窒息发生率比较差异无统计学意义(P>0.05)。结论:完善产科检查,尽早筛查和明确诊断妊娠期糖尿病,以便及早进行饮食调整、加强运动以控制其体重增长,并进行血糖监测,必要时调整机体的胰岛素水平,以期减少不良妊娠结局的发生,降低母婴并发症率,保证孕妇及围产儿的生命健康。
【关键词】 妊娠期糖尿病 糖化血红蛋白 体重
[Abstract] Objective: To investigate the influence of glycated hemoglobin level and body mass index on pregnancy outcome in patients with gestational diabetes. Method: A total of 184 puerperae undergoing antenatal examination and delivery from January 2013 to December 2015 in our hospital were included in the study. According to the diagnostic criteria for gestational diabetes, the women were divided into the normal group of 93 cases and the gestational diabetes group of 91 cases. The gestational diabetes mellitus puerperae were divided into the standard group of 44 cases and the substandard group of 47 cases according to the level of glycosylated hemoglobin before delivery. According to different weight gain standards, 91 puerperae with GDM were divided into the excessive increase group of 13 cases, the appropriate increase group of 45 cases and the insufficient increase group of 33 cases. To compare the pregnancy complications and outcomes of pregnant women with different glycosylated hemoglobin levels during pregnancy and pregnancy, to explore the effects of glycated hemoglobin levels and weight gain during pregnancy on complications during pregnancy and postpartum and fetal and neonatal conditions in patients with gestational diabetes. The complications and outcomes of pregnancy between puerperae with different glycosylated hemoglobin levels and gestational diabetes mellitus with different weight gain during pregnancy were compared in order to explore the effects of glycosylated hemoglobin level and weight gain during pregnancy on the complications of gestational diabetes mellitus during pregnancy, postpartum, fetus and newborn. Result: The incidence of gestational hypertension, preeclampsia, postpartum hemorrhage and macrosomia in the substandard group was higher than that in the standard group and the normal group, the number of gestational weeks at birth was shorter than that in the standard group and the normal group, the differences were statistically significant (P<0.05). The incidence of hypertension during pregnancy, preeclampsia, postpartum hemorrhage and macrosomia in the reaching standard group was significantly higher than that in the normal group (P<0.05), but there were no significant differences in the incidence of amniotic fluid, fetal malformation, premature rupture of membranes, caesarean section and neonatal asphyxia among the three groups (P>0.05). The incidence of postpartum hemorrhage and macrosomia was higher than that in the normal and undergrowth, the differences were statistically significant (P<0.05). There were no significant differences in pregnancy hypertension, preeclampsia, amniotic fluid, fetal malformation, premature rupture of membranes, gestational weeks at birth, caesarean section and neonatal asphyxia among different weight gain puerperae (P>0.05). Conclusion: Improve obstetric screening, early screening and diagnosis of gestational diabetes, so that early dietary adjustment, exercise to control their weight gain, and blood glucose monitoring, if necessary, adjust the bodys insulin level, with a view to reducing the incidence of adverse pregnancy outcomes, reducing the incidence of maternal and infant complications, and ensuring the health of pregnant women and perinatal children.
3 讨论
GDM多发生在妊娠中、晚期,原因如下:在妊娠早、中期,胎儿通过胎盘从母体获取葡萄糖的量会随孕周的增加而增加;部分孕妇孕期排糖量会增加,主要由于肾血浆流量及肾小球滤过率增加,而肾小管对糖的再吸收率不变;大量合成分泌的孕、雌激素有利于母体更好地利用葡萄糖,以上三点均可增强孕妇空腹时清除葡萄糖的能力,导致孕妇的空腹血糖约降低10%,甚至发生低血糖或酮症酸中毒。为维持正常糖代谢水平,到妊娠中、晚期,孕妇机体会自动调节,大量合成分泌雌激素、孕酮、胎盘生乳素、皮质醇和胎盘胰岛素酶等抗胰岛素样物质,使孕妇对胰岛素的敏感性随孕周增加而下降[3]。Tomazic等[4]研究结果表明,GDM孕妇胰岛素受体酪氨酸激酶和胰岛素受体-1磷酸化水平下降,导致细胞膜蛋白浓度明显增加,且有比较明显的胰岛素信号通路的受体后缺陷,这些提示她们存在胰岛素抵抗。进而孕妇机体对胰岛素需求量也会相应增加,对于不能代偿胰岛素高需求的孕妇,妊娠期血糖升高,使原有糖尿病加重或出现GDM[5-6]。
本研究结果提示,HbA1c>6%的未达标组产妇妊娠期高血压疾病、子痫前期、产妇产后出血和巨大儿发生率均高于达标组和无妊娠期糖尿病的产妇,而胎儿出生时孕周数均短于达标组和正常组(P<0.05)。在GDM产妇中,体重增幅过多的产妇产后出血和巨大儿发生率高于增幅正常和增幅不足的产妇。
HbA1c>6%的未达标组产妇妊娠期高血压发生率高的原因有:妊娠期糖尿病孕妇,在妊娠中、晚期,机体内含有的胰岛素较正常孕妇多,高水平的胰岛素促使血管平滑肌细胞分裂增生,导致血管直径变小,增大血管阻力;其次会刺激毛细血管使交感神经兴奋性增强,使血压升高,第三增强肾脏对钠的重吸收,血容量增加,导致妊娠期糖尿病的孕妇更易发生妊娠期高血压病[7]。子痫前期发生率高的原因:妊娠期糖尿病孕妇糖化血红蛋白>6%时,子痫前期发生率高可能与糖代谢和脂代谢异常有关,但具体的机制还不明确。
而HbA1c未达标组和体重增幅过多产妇的巨大儿发生率高的原因可能为:GDM孕妇血糖长期处于较高水平,胎儿长期处于母体高血糖环境,而母体的胰岛素较难透过胎盘进入胎儿体内,刺激胎儿胰岛β细胞的增生,所以胎儿自身合成分泌了大量胰岛素,导致胎儿出现高胰岛素血症,氨基酸转移系统被激活,胎儿机体蛋白质、脂肪合成增强和脂解作用被抑制,胎儿组织内大量脂肪沉积,导致躯干过度发育。糖尿病母亲所生新生儿的特点是肩背部皮下脂肪的堆积,肩部容易受到产道的阻力而发生难产,肥厚的肩部及巨大儿均会延长产程,增大对母体产道的损伤;同时,母体长期处于高血糖状态,有利于各种组织的蛋白质分子在非酶催化条件下被糖基化,被糖基化的蛋白质分子与未被糖基化的分子相互结合交联,进一步形成大分子的糖基化终产物,早期这一过程是可逆的,一旦生成是不可逆的,这些产物不会被代谢而不断积累,沉积于血管壁的半衰期较长的蛋白质上,造成微血管通透性增加[8-9],极易引发产妇在生产过程中的大出血以及产后出血等[10-11]。妊娠期糖尿病导致早产的原因有专家认为与孕妇的血糖水平过高,导致羊膜产生刺激,羊水分泌过多有关[12-13]。
综上所述,完善产科检查,尽早筛查和明确诊断妊娠期糖尿病,以便及早进行饮食调整、加强运动以控制其体重增长,并进行血糖监测,必要时调整机体的胰岛素水平,以期减少不良妊娠结局的发生,降低母婴并发症率,保证孕妇及圍产儿的生命健康。
参考文献
[1] Shaat N,Groop L.Genetics of gestational diabetes mellitus[J].Curr Med Chem,2007,14(5):569-583.
[2] Pettitt D J,Ospina P,Kolaczynski J W,et al.Comparison of an insulin analogue, insulin aspart, and regular human insulin with no insulin in gestational diabetes mellitus[J].Diabetes Care,2003,26(1):183-186.
[3]邱先桃,丘媛媛,代玉梅,等.妊娠期糖尿病孕晚期血清尿酸与产后糖代谢异常的相关性分析[J].中国糖尿病杂志,2014,22(5):395-397.
[4] Tomazic M,Janez A,Sketelj A,et al.Comparison of alterations in insulin signaling pathway in adipocytes from type 2 diabetic pregnant women and women with gestational diabetes mellitus[J].Diabet Ologia,2002,45(4):502-508.
[5]张扬子,吴红花.妊娠期糖尿病产后糖代谢转归的研究进展[J].中华糖尿病杂志,2016,8(5):304-306.
[6]代明甫,李倩,钟思燕,等.妊娠期糖代谢异常的相关危险因素分析[J].河北医学,2015,21(7):1067-1070.
[7]刘春娟.妊娠期糖代谢异常和妊娠期高血压的相关性探讨[J].现代诊断与治疗,2014,25(16):3744-3745.
[8]狄英波.妊娠期糖代谢异常患者糖化血红蛋白、血脂测定和尿微量白蛋白的临床意义[J].中国妇幼保健,2014,29(10):1535-1536.
[9] Sacks D B,Bruns D E,Goldstein D E,et al.Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus[J].Clin Chem,2002,48(3):436-472.
[10]郑再娟,吴秋英.孕期体重规划干预及健康教育对妊娠的影响[J].现代预防医学,2012,39(12):3035-3036.
[11]孟国花,周玲.孕前体质指数及孕期体重的增加对妊娠结局的影响[J].安徽医药,2012,16(6):778-780.
[12]张静,王小华.孕前体重指数及孕期体重增长与妊娠结局的关系[J].中国社区医师:医学专业,2013,15(8):136,138.
[13]史伟,马秀华.孕前超重及孕期增重对妊娠期糖尿病孕妇妊娠结局的影响[J].中国医学创新,2018,15(15):20-23.
(收稿日期:2019-06-13) (本文编辑:马竹君)
