神经外科术后脑脊液PCT影响因素及价值研究
2023-11-13王华军付晔周成杰欧阳礼枝
王华军,付晔,周成杰,欧阳礼枝
神经外科术后脑脊液PCT影响因素及价值研究
王华军,付晔,周成杰,欧阳礼枝
宁波大学附属人民医院重症医学科,浙江宁波 315040
探讨神经外科术后脑脊液降钙素原(procalcitonin,PCT)的影响因素及临床价值。收集2021年1月至2022年5月宁波大学附属人民医院神经外科术后所有怀疑颅内感染患者腰椎穿刺或脑室引流的脑脊液及血清样本。Logistic多因素分析神经外科术后脑脊液PCT升高的影响因素。所有研究对象根据颅内感染诊断标准分为颅内感染组和无菌性脑膜炎组。非参数检验比较颅内感染组和无菌性脑膜炎组各指标差异。采用受试者操作特征曲线(receiver operating characteristic curve,ROC曲线)评价各指标对颅内感染的诊断效能。本研究共入组139例患者,其中109例患者脑脊液PCT升高(78.4%),其中颅内感染患者59例(54.1%),无菌性脑膜炎患者50例(45.9%)。Logistic多因素分析结果表明,颅内感染和血性脑脊液是神经外科术后脑脊液PCT增高的独立危险因素;颅内感染组与无菌性脑膜炎组的脑脊液PCT和血清PCT水平差异无统计学意义。两组患者的脑脊液乳酸水平和脑脊液PCT/血清PCT差异有统计学意义。脑脊液PCT、血清PCT、脑脊液乳酸、脑脊液PCT/血清PCT、脑脊液PCT和乳酸联合诊断ROC曲线下面积分别为0.56、0.58、0.82、0.85、0.83。颅内感染和血性脑脊液是神经外科术后脑脊液PCT升高的独立因素。单纯以脑脊液PCT增高诊断神经外科术后颅内感染价值有限,需通过联合其他指标提高诊断效能。
颅内感染;降钙素原;血清;脑脊液;乳酸;影响因素;神经外科术后
神经外科术后颅内感染是临床常见的并发症,发生率达19.3%,但颅内感染的诊断目前缺少特异性症状和体征,实验室检查缺乏特异性生物学标志物,难以和无菌性脑膜炎相鉴别[1]。颅内感染一旦诊断延误,治疗不及时,将导致不可逆的后果,因而早期诊断和鉴别极为重要。降钙素原(procalcitonin,PCT)作为诊断颅内感染的潜在生物标志物目前尚有争论,因此探讨神经外科术后患者脑脊液中PCT的影响因素将有助于阐明其临床应用价值。
1 资料与方法
1.1 一般资料
收集2021年1月至2022年5月在宁波大学附属人民医院重症监护室住院的所有神经外科术后被怀疑颅内感染患者的脑脊液和血清样本。纳入标准:①神经外科术后入住重症监护室,且年龄>18岁; ②体温>38.5℃,出现意识改变或其他疑似颅内感染的症状;③具有腰椎穿刺或脑室外引流适应证。排除标准:①合并脓毒症;②肾衰竭;③术前发热或确诊颅内感染;④孕妇;⑤年龄<18岁;⑥有颅内高压等腰椎穿刺禁忌证。所有研究对象参照美国医院感染定义关于颅内感染诊断标准分为颅内感染组和无菌性脑膜炎组[2]。本研究经宁波大学附属人民医院医学伦理委员会批准[伦理审批号:2021(预)042],患者均签署书面知情同意书。
1.2 颅内感染的诊断标准
①患者有术后发热、头痛、颈部僵硬、意识改变等临床表现;②脑脊液葡萄糖水平<2.5mmol/L或脑脊液/血清葡萄糖比值<0.4;③脑脊液白细胞(white blood cell,WBC)计数≥1000个/μl,多核细胞百分比≥75%;④脑脊液培养阳性。符合④即诊断为颅内感染;脑脊液培养阴性,但符合①②③三项也诊断为颅内感染。
1.3 PCT检测方法
所有患者均行腰椎穿刺或脑室引流管收集脑脊液标本。使用自动化学分析仪检测蛋白质、氯和葡萄糖水平。采用酶联免疫吸附试验(enzyme linked immunosorbent assay,ELISA)检测PCT。阳性下限为0.01pg/ml。乳酸使用血气分析仪进行检测。无菌条件下采集外周静脉血,同一患者脑脊液标本与采血间隔<0.5h。
1.4 统计学方法

2 结果
2.1 脑脊液PCT结果
颅内感染63例,男25例,女38例,年龄38~81岁,平均(62.6±13.2)岁,共有20例患者检出病原菌25株,其中革兰阳性菌13株(52%),包括凝固酶阴性葡萄球菌4株、表皮葡萄球菌5株、金黄色葡萄球菌2株、溶血葡萄球菌1株、屎肠球菌 1株;革兰阴性菌12株(48%),包括肺炎克雷伯菌3株、大肠埃希菌1株、鲍曼不动杆菌4株、铜绿假单胞菌2株、嗜麦芽窄食单胞菌1株、锯齿放线菌1株。无菌性脑膜炎组76例,男33例,女43例,年龄42~85岁,平均(62.8±12.8)岁。本研究根据脑脊液PCT值分为PCT升高组(PCT>0.05ng/ml)和PCT正常组(PCT≤0.05ng/ml)。结果显示PCT升高组109例患者,其中颅内感染59例,无菌性脑膜炎50例。
2.2 脑脊液PCT升高的多因素分析
将颅内感染、血性脑脊液、年龄、性别、癫痫、颅内肿瘤、创伤进行单因素分析后,把<0.20的因素行Logistic多因素分析,提示颅内感染,血性脑脊液是神经外科术后脑脊液PCT升高的独立危险因素(<0.05),见表1、表2。
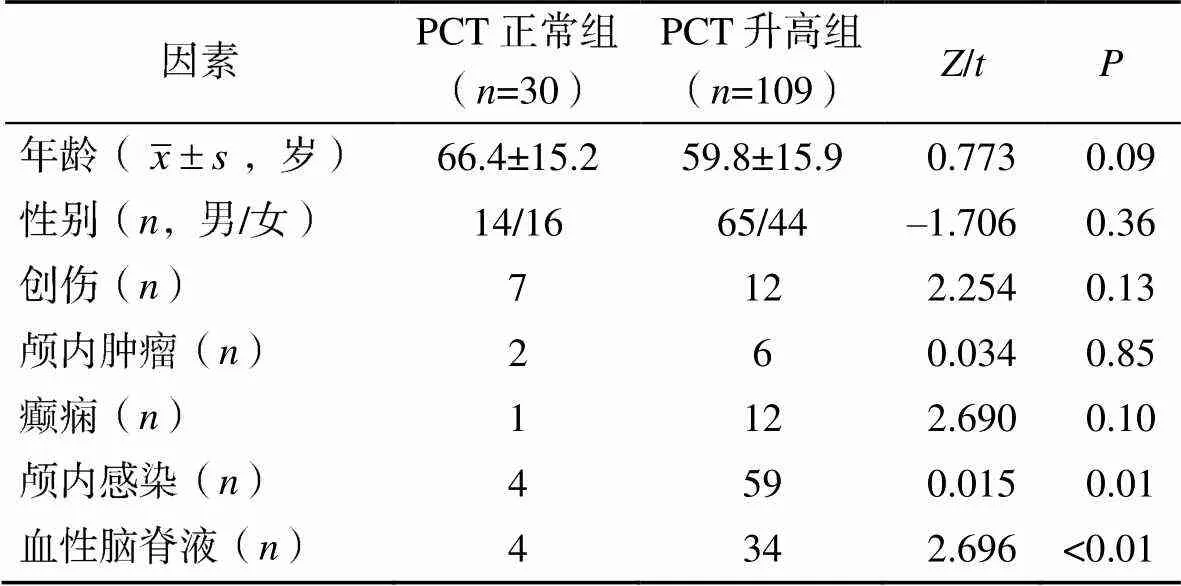
表1 脑脊液PCT升高的单因素分析

表2 脑脊液PCT的多因素分析
2.3 颅内感染组和无菌性脑膜炎组患者的脑脊液PCT及血清PCT比较
颅内感染组和无菌性脑膜炎组患者的脑脊液PCT中位数分别为0.14(0.09,0.25)ng/ml和0.12(0.05,0.23)ng/ml,差异无统计学意义(>0.05),见图1。颅内感染组和无菌性脑膜炎组患者的血清PCT中位数分别为0.10(0.06,0.28)ng/ml和0.19(0.08,0.53)ng/ml,差异无统计学意义(>0.05),见图2。颅内感染组和无菌性脑膜炎组患者的脑脊液乳酸水平中位数分别为6.45(4.48,8.33)mmol/L和3.20(2.02,4.20)mmol/L,差异有统计学意义(<0.05),见图3。颅内感染组和无菌性脑膜炎组患者的脑脊液PCT/血清PCT分别为1.61(1.00,2.76)和0.65(0.42,0.85),差异有统计学意义(<0.05),见图4。

图1 颅内感染组和无菌性脑膜炎组患者的脑脊液PCT比较
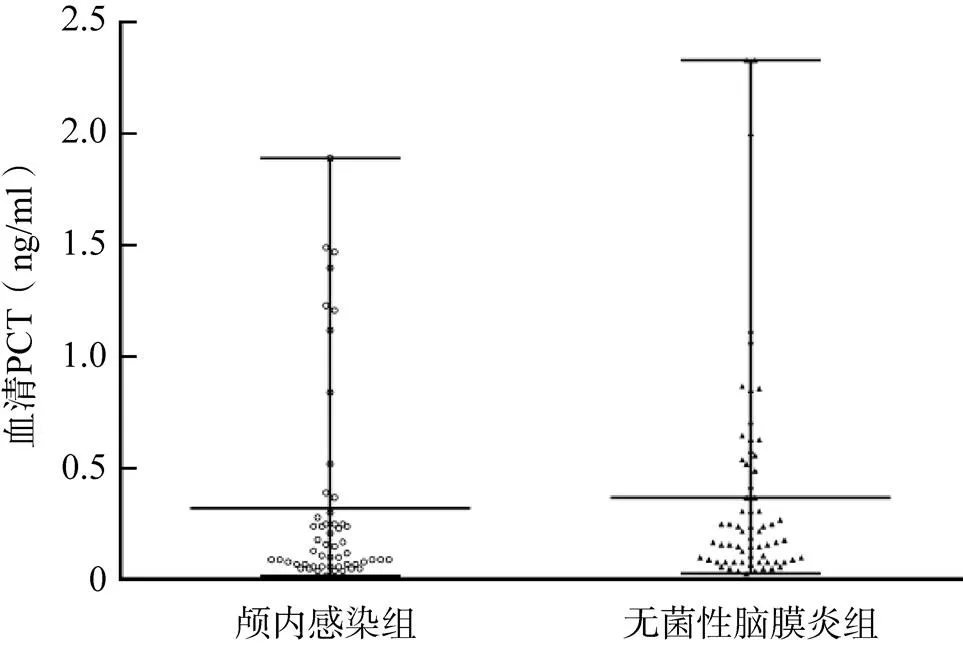
图2 颅内感染组和无菌性脑膜炎组患者的血清PCT比较
2.4 颅内感染诊断的效能分析
脑脊液PCT、血清PCT、脑脊液乳酸、脑脊液PCT/血清PCT、脑脊液PCT联合乳酸检测的ROC曲线下面积分别为0.56、0.58、0.82、0.85、0.83,提示脑脊液PCT联合乳酸或采取脑脊液PCT/血清PCT有良好的诊断效能,见图5。

图3 颅内感染组和无菌性脑膜炎组患者的脑脊液乳酸比较
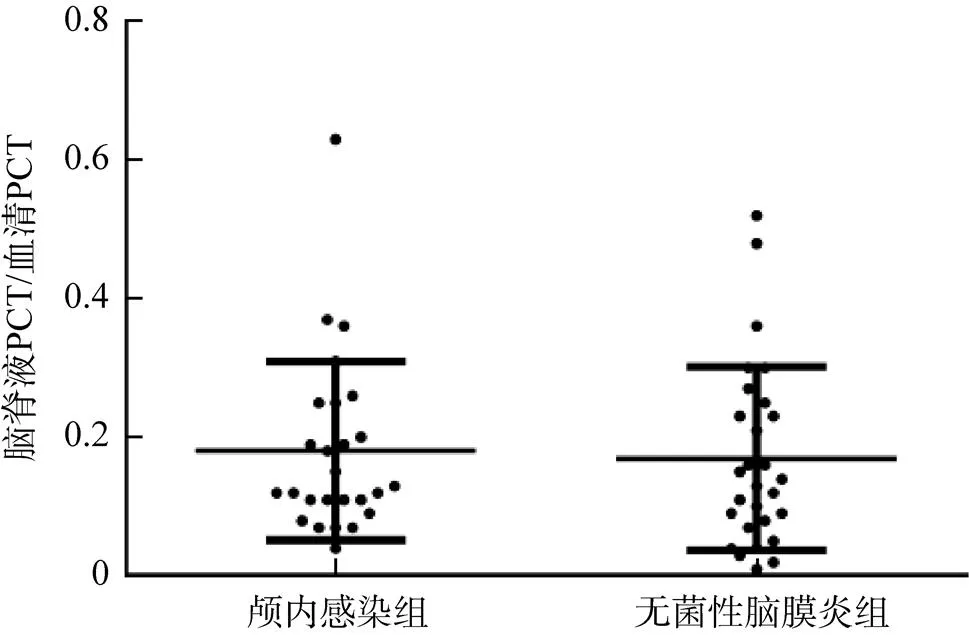
图4 颅内感染组和无菌性脑膜炎组患者的脑脊液PCT/血清PCT比较

图5 各指标诊断颅内感染的ROC曲线
3 讨论
PCT作为炎症指标,在机体严重感染时显著增加,被广泛应用于细菌感染的诊断和治疗效果评估[3-4]。有研究认为脑脊液PCT升高可用于颅内感染的诊断[5-8];也有研究认为脑组织本身并不分泌PCT,而大分子的PCT也难通过血-脑脊液屏障,但手术破坏血-脑脊液屏障后,血清PCT可能对脑脊液PCT产生影响[9-10]。此外,有研究显示脑脊液PCT在创伤、手术、蛛网膜下腔出血等非颅内感染患者中升高,表明脑脊液PCT增高缺乏特异性[11-12]。脑脊液PCT在神经外科术后颅内感染的诊断价值存在争议,因此,进一步研究脑脊液PCT的来源及影响因素有助于明确其对神经外科术后颅内感染的诊断价值[13-14]。
本研究中神经外科术后颅内感染检出的病原菌以革兰阳性菌为主,与既往报道类似,但研究显示革兰阴性菌比例有升高趋势,提示在神经外科颅内感染治疗中除关注革兰阳性菌外,也需高度警惕革兰阴性菌[15-16]。本研究显示除颅内感染患者外,大部分无菌性脑膜炎患者脑脊液PCT也增高,通过多因素分析,发现除颅内感染外,血性脑脊液也是脑脊液PCT升高的独立危险因素,与Gautam-Goyal等[11]研究结果一致,而年龄、性别、癫痫、创伤、颅内肿瘤对脑脊液PCT升高无影响。血性脑脊液导致脑脊液PCT增高的机制尚不明确,有研究认为可能与血性脑脊液激活免疫细胞进而释放PCT相关[17]。有研究通过联合检查脑脊液PCT与乳酸、肝素结合蛋白、C反应蛋白、神经烯醇化酶等指标,结果显示可提高诊断的敏感度和准确性[18-20];另一项研究发现,联合检测脑脊液PCT、乳酸、蛋白浓度与血糖比值可对术后脑膜炎进行诊断,且缩短诊断时间,提高治疗成功率[21]。本研究结果显示联合检测脑脊液PCT和乳酸,或使用脑脊液PCT/血清PCT比值诊断颅内感染,可明显提高诊断效能。
综上所述,脑脊液PCT增高呈非特异性,除颅内感染外,血性脑脊液也是脑脊液PCT增高的独立危险因素,单纯以脑脊液PCT增高诊断颅内感染价值有限,但联合乳酸、肝素结合蛋白等指标可提高其对神经外科术后颅内感染的诊断效能。由于本研究的样本量较小,还需更大规模的研究进一步验证。
[1] SALMANOV A G, SHCHEHLOV D V, SVYRYDIUK O, et al. Pastushyn surgical site infections after neurosurgical procedures in Ukraine: Results of a multicenter study (2018–2020)[J]. Wiad Lek, 2022, 75(1): 27–33.
[2] KARVOUNIARIS M, BROTIS A, TSIAKOS K, et al. Current perspectives on the diagnosis and management of healthcare-associated ventriculitis and meningitis[J]. Infect Drug Resist, 2022, 28(15): 697–721.
[3] LEE C C, KWA A L H, APISARNTHANARAK A, et al. Procalcitonin (PCT)-guided antibiotic stewardship in Asia-pacific countries: Adaptation based on an expert consensus meeting[J]. Clin Chem Lab Med, 2020, 58(12): 1983–1991.
[4] HARTWELL J L, ZIMMERS T A. What’s new in shock, July 2019?[J]. Shock, 2019, 52(1): 1–4.
[5] WEI T T, HU Z D, QIN B D, et al. Diagnostic accuracy of procalcitonin in bacterial meningitis versus nonbacterial meningitis: A systematic review and Meta-analysis[J]. Medicine (Baltimore), 2016, 95(11): e3079.
[6] LIU D B, ZHANG H P, YU K, et al. A study on correlations of procalcitonin and interleukin-6 with viral meningitis[J]. Eur Rev Med Pharmacol Sci, 2018, 22(11): 3474–3478.
[7] ZHU L, DONG L, LI Y, et al. The diagnostic and antibiotic reference values of procalcitonin for intracranial infection after craniotomy[J]. World Neurosurg, 2019, 126: e1–e7.
[8] 王华军, 王慧晓, 李纪鹏, 等.降钙素原在神经外科术后颅内感染评估中的应用价值[J]. 浙江医学, 2020, 42(13): 1391–1395.
[9] HALVORSON K, SHAH S, FEHNEL C, et al. Procalcitonin is a poor predictor of non-infectious fever in the neurocritical care unit[J]. Neurocrit Care, 2017, 27(2): 237–241.
[10] DUTTA S, SACHDEVA N, PAL A, et al. Cerebrospinal fluid and plasma procalcitonin for the diagnosis of neonatal bacterial meningitis[J]. J Paediatr Child Health, 2022, 58(8): 1425–1430.
[11] GAUTAM-GOYAL P, MALHOTRA P, EPSTEIN M, et al. Can procalcitonin be used as a reliable marker for infectious fever in patients with intracranial hemorrhage?[J]. World Neurosurg, 2018, 116: e968–e974.
[12] ALRAWAHI A N, ALHINAI F A, DOIG C J, et al. The prognostic value of serum procalcitonin measurements in critically injured patients: A systematic review[J]. Crit Care, 2019, 23(1): 390.
[13] TUNKEL A R, HASBUN R, BHIMRAJ A, et al. 2017 infectious diseases society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis[J]. Clin Infect Dis, 2017, 64(6): e34–e65.
[14] VAN DE BEEK D, CABELLOS C, DZUPOVA O, et al. ESCMID guideline: Diagnosis and treatment of acute bacterial meningitis[J]. Clin Microbiol Infect, 2016, 22(3): S37–S62.
[15] YANG W, WU X, LI Z, et al. Trends of intra-cranial bacterial infection in patients requiring emergency neurosurgery[J]. Surg Infect (Larchmt), 2020, 21(8): 677–683.
[16] CHANG J B, WU H, WANG H, et al. Prevalence and antibiotic resistance of bacteria isolated from the cerebrospinal fluid of neurosurgical patients at Peking Union Medical College Hospital[J]. Antimicrob Resist Infect Control, 2018, 7(1): 1–6.
[17] ZHANG L, MA L, ZHOU X, et al. Diagnostic value of procalcitonin for bacterial meningitis in children: A comparison analysis between serum and cerebrospinal fluid procalcitonin levels[J]. Clin Pediatr(Phila), 2019, 58(2): 159–165.
[18] JULIÁN-JIMÉNEZ A, MORALES-CASADO M I. Usefulness of blood and cerebrospinal fluid laboratory testing to predict bacterial meningitis in the emergency department[J]. Neurologia (Engl Ed), 2019, 34(2): 105–113.
[19] 刘辉, 杜文杰, 符会涛, 等. 脑脊液降钙素、超敏C反应蛋白、神经元特异性烯醇化酶水平在脑膜炎预后预测及感染类型鉴别中的作用[J]. 国际神经病学神经外科学杂志, 2022, 49(1): 46–50.
[20] 李晓亮, 张小章, 何震. 脑脊液PCT、CD64、HBP联合检测对神经外科术后细菌性脑膜炎的诊断价值[J]. 重庆医学, 2021, 50(22): 3871–3873.
[21] 郑光辉, 张艳, 李方强, 等. 脑脊液降钙素原、乳酸联合常规生物标志物在神经外科术后细菌性脑膜炎诊断中的价值[J]. 中华临床感染病杂志, 2019, 12(2): 101–106.
Influencing factors and value of cerebrospinal fluid PCT after neurosurgery
Department of Critical Care Medicine, Affiliated People’s Hospital of Ningbo University, Ningbo 315040, Zhejiang, China
To explore the influence factors and clinical value of postoperative procalcitonin (PCT) in cerebrospinal fluidamong patients after neurosurgery.Cerebrospinal fluid and serum samples were collected from patients had been suspected of intracranial infection after craniotomy in Affiliated People’s Hospital of Ningbo University from January 2021 to May 2022 by lumbar puncture or ventricular drainage tube. Logistics multivariate analysis was performed to identify factors associated with elevated cerebrospinal fluid PCT levels after neurosurgery. Based on the diagnostic criteria for intracranial infection, the study subjects were divided into two groups: The intracranial infection group and the aseptic meningitis group. Nonparametric test was conducted to compare the differences in various indicators between the intracranial infection group and the aseptic meningitis group. The diagnostic efficacy of each index was assessed using receiver operating characteristic (ROC) curve.A total of 139 cases of cerebrospinal fluidwere collected in this study, 109 cases of cerebrospinal fluid PCT increased (78.4%), including 59 cases of intracranial infection (54.1%), 50 cases of aseptic meningitis (45.9%). Logistics multivariate analysis showed that intracranial infection and bloody cerebrospinal fluidwere the influencing factors for the increase of cerebrospinal fluid PCT. There was no statistically significant difference in cerebrospinal fluid PCT and serum PCT levels between the intracranial infection group and the aseptic meningitis group. Significant differences were observed in cerebrospinal fluid lactate levels and cerebrospinal fluid PCT/serum PCT ratio between the two groups. The area under the ROC of cerebrospinal fluid PCT, serum PCT, cerebrospinal fluidlactate, cerebrospinal fluid PCT/serum PCT, cerebrospinal fluid PCT and lactatewere 0.56, 0.58, 0.82, 0.85, 0.83, respectively.Intracranial infection and bloody cerebrospinal fluid are independent factors for the elevation of cerebrospinal fluid PCT after neurosurgery. The diagnostic value of PCT elevation in cerebrospinal fluid alone for intracranial infection after neurosurgery is limited, and it is necessary to improve the diagnostic efficacy by combining other indicators.
Intracranial infection; Procalcitonin; Serum; Cerebrospinal fluid; Lactate; Influencing factors; Postoperative neurosurgery
R63
A
10.3969/j.issn.1673-9701.2023.30.004
浙江省宁波市医学科技计划项目(2020Y44);浙江省医药卫生科技计划项目(2022KY1183)
王华军,电子信箱:whj269696@163.com
(2022–11–16)
(2023–09–28)
