Clinical characteristics and outcomes of nosocomial COVID-19 in Turkey: A retrospective multicenter study
2023-10-10leymanldCelalettinlmazlruPolatSerapArgunBarislknurBayiitlknurKayaCeydaAnarMihribanBozkurtsnBaykalHulyaDirolGamzenurOzbeyEmineOzsariEmelCireliAliKadrirakDursunTatarMineGayafSelenKaraoglanogluYenerAydinAtillaErogluld
Süleyman Yıldırım, Celalettin Yılmaz, Gülru Polat, Serap Argun Baris, İlknur Bayiit, İlknur Kaya, Ceyda Anar, Mihriban Bozkurt, Hüsnü Baykal, Hulya Dirol, Gamzenur Ozbey, Emine Ozsari, Emel Cireli, Ali Kadri ırak, Dursun Tatar, Mine Gayaf, Selen Karaoglanoglu, Yener Aydin, Atilla Eroglu, Yıldız Olar, Berna Botan Yıldırım, Bengül Gürsoy, Deniz Demir Yılmaz, Elif Yelda Ozgun Niksarlioglu, Ramazan Eren, Ayegül Tomruk Erdem, Müge Meltem Tor, Fusun Fakili, Mustafa Çolak, Merve Erelik, Ali Tabaru, Özlem Ediboglu
1Intensive Care Unit, Dr.Suat Seren Chest Disease and Surgery Training and Research Hospital, University of Health Sciences Turkey, İzmir, Turkey
2Department of Pulmonology, Dr.Suat Seren Chest Disease and Surgery Training and Research Hospital, University of Health Sciences Turkey, İzmir, Turkey
3Department of Pulmonary Medicine, School of Medicine, Kocaeli University, Kocaeli, Turkey
4Department of Pulmonology, Kütahya Health Sciences University, Kütahya, Turkey
5Department of Pulmonology, Atatürk Training and Research Hospital, İzmir Katip Çelebi University, İzmir, Turkey
6Department of Pulmonology, Ankara Atatürk Sanatory Training and Research Hospital, University of Health Sciences, Ankara, Turkey
7Department of Pulmonology, Faculty of Medicine, Akdeniz University, Antalya, Turkey
8Department of Pulmonology, Bolu Abant İzzet Baysal University Training and Research Hospital, Bolu, Turkey
9Department of Pulmonology, Ordu University Training and Research Hospital, Ordu, Turkey
10Department of Thoracic Surgery, Medical Faculty, Erzurum, Ataturk University, Turkey
11Department of Infectious Disease and Clinical Microbiology, Kastamonu Training and Research Hospital, Kastamonu, Turkey
12Department of Pulmonology, Başkent University Hospital Konya, Konya, Turkey
13Department of Pulmonology, İstanbul Sancaktepe Şehit Prof.Dr.İlhan Varank Training and Research Hospital, İstanbul, Turkey
14Department of Chest Diseases, Yedikule Chest Diseases and Thoracic Surgery Training and Research Hospital, Health Science University, İstanbul, Turkey
15Department of Pulmonology, Faculty of Medicine, Zonguldak Bülent Ecevit University, Zonguldak, Turkey
16Department of Pulmonary Medicine, Gaziantep, Faculty of Medicine, Şahinbey Research Hospital, Gaziantep University, Turkey
17Department of Pulmonology, Balıkesir, Health Practice and Research Hospital, Balıkesir University, Turkey
18Department of Pulmonology, Afyonkarahisar Dinar State Hospital, Afyon, Turkey
19Department of Pulmonology, Söke Fehime Faik Kocagöz State Hospital, Aydın, Turkey
ABSTRACT
Objective: To identify the clinical characteristics and outcomes of hospital-acquired SARS-CoV-2 infection during the vaccination period nationwide in Turkey.
Methods: COVID-19 patients followed in the pandemic services across Turkey between January 1, 2021, and March 31, 2022 were investigated retrospectively.Nosocomial COVID-19 was defined as a patient neither diagnosed with COVID-19 nor suspected COVID-19 at the hospital admission and was confirmed COVID-19≥5 days after hospital admission.The primary outcome of this study was in-hospital mortality; demographic features and vaccination status was compared between survivors and nonsurvivors.
Results: During the study period, 15573 COVID-19 patients were followed in 18 centers and 543 (3.5%) patients were nosocomial COVID-19.Most patients with nosocomial COVID-19 (80.4%)were transferred from medical wards.162 (29.8%) of the patients with nosocomial COVID-19 admitted to the intensive care unit due to disease severity and 138 (25.4%) of the patients died during hospital stay.Advanced age (≥65 years) and number of comorbid diseases (≥2) was found to be associated with mortality in nosocomial COVID-19 (OR 1.74, 95% CI 1.11-2.74 and OR 1.60,95% CI 1.02-2.56, respectively).Vaccination was associated with survival in nosocomial COVID-19 (OR 0.25, 95% CI 0.16-0.38).
Conclusions: Patients with nosocomial COVID-19 had increased admission to intensive care units and higher mortality rate.Vaccination can decrease the in-hospital mortality rate.
KEYWORDS: COVID-19; Nosocomial infection; Vaccination;Intensive care unit
Significance
Nosocomial COVID-19 patients had a higher rate of mortality than community-acquired cases.Vaccination against SARSCoV-2 decreases the need for intensive care unit admission and in-hospital mortality in patients with nosocomial COVID-19.
1.Introduction
The coronavirus disease-19 (COVID-19) spread rapidly and turned into an outbreak over the last two years.The virus can be transmitted from a person to others via respiratory droplets and close contact increases the risk of transmission[1].
Closed, crowded, and poorly ventilated places are especially risky for transmission.Unfortunately, hospitals are one of the most highrisk places for spreading COVID-19.In multicenter studies, 12.5% to 17.3% of patients with COVID-19 who followed up in hospital were defined as having nosocomial COVID-19[2,3].The incidence of nosocomial COVID-19 varies from 0% to 65%[4,5].Dialysis centers and long-term care facilities had higher nosocomial COVID-19 rates while surgical wards had lower nosocomial COVID-19 rates[6].
Nosocomial COVID-19 patients had a higher rate of mortality than community-acquired cases.Advanced age and comorbid conditions such as cancer were associated with mortality in nosocomial COVID-19, and the mortality rate was 1.3 times greater in nosocomial COVID-19 than in community-acquired cases[2,7,8].
This study aimed to determine the clinical characteristics and outcomes of hospital-acquired SARS-CoV-2 infection during the vaccination period nationwide in Turkey.
2.Subjects and methods
2.1.Study population
This is a retrospective study carried out in eighteen hospitals in Turkey between January 1, 2021, and March 31, 2022.Patients(18 years and older) diagnosed with nosocomial COVID-19 and transferred to pandemic services were included in the study.Nosocomial COVID-19 was defined as a patient neither diagnosed with COVID-19 nor suspected COVID-19 at the hospital admission and a confirmed COVID-19 by reverse-transcription polymerase chain reaction (RT-PCR) after ≥5 days after hospital admission[9](Figure 1).

Figure 1.Flow chart of patient selection process.*Nosocomial COVID-19 was defined as a patient neither diagnosed with COVID-19 nor suspected COVID-19 at the hospital admission and a confirmed COVID-19 by reverse-transcription polymerase chain reaction (RT-PCR) after ≥5 days after hospital admission.
2.2.Data collection
Patients’ demographic features, comorbidities, smoking status,vaccination status and ward which patient was followed before transferred pandemic ward were obtained from medical records of each center.
2.3.Statistical analysis
Continuous variables were shown as mean±standard deviation(SD) if they were normally disturbed, and they were presented as median and interquartile range (IQR) if they were not normally disturbed.Nomimal variables were shown as n (%).Continuous variables were compared with thet-test or Mann-WhitneyUtest and nominal variables were compared with Chi-square test.Among 543 patients with nosocomial COVID-19, 3 of them were transferred to other health care centers so their survivor status was unknown.The remaining 540 patients were compared for mortality.A multivariate regression analysis was performed to detect risk factors for mortality.Pvalue <0.05 was considered as statistically significant.
2.4.Ethical statement
The study was conducted after the approval of the local ethic committee (IRB number: 2022/21-23).The study was carried out in accordance with Declaration of Helsinki 2013.
3.Results
A total of 543 patients were included in the final analysis with the mean age of (65.1±15.7) years, and 333 (61.3%) patients were male.The most common comorbidities were hypertension (n=259,47.7%), diabetes mellitus (n=158, 29.1%), and 64.1% of patients had at least two comorbidities.We summarized the demographic features of patients in Table 1.
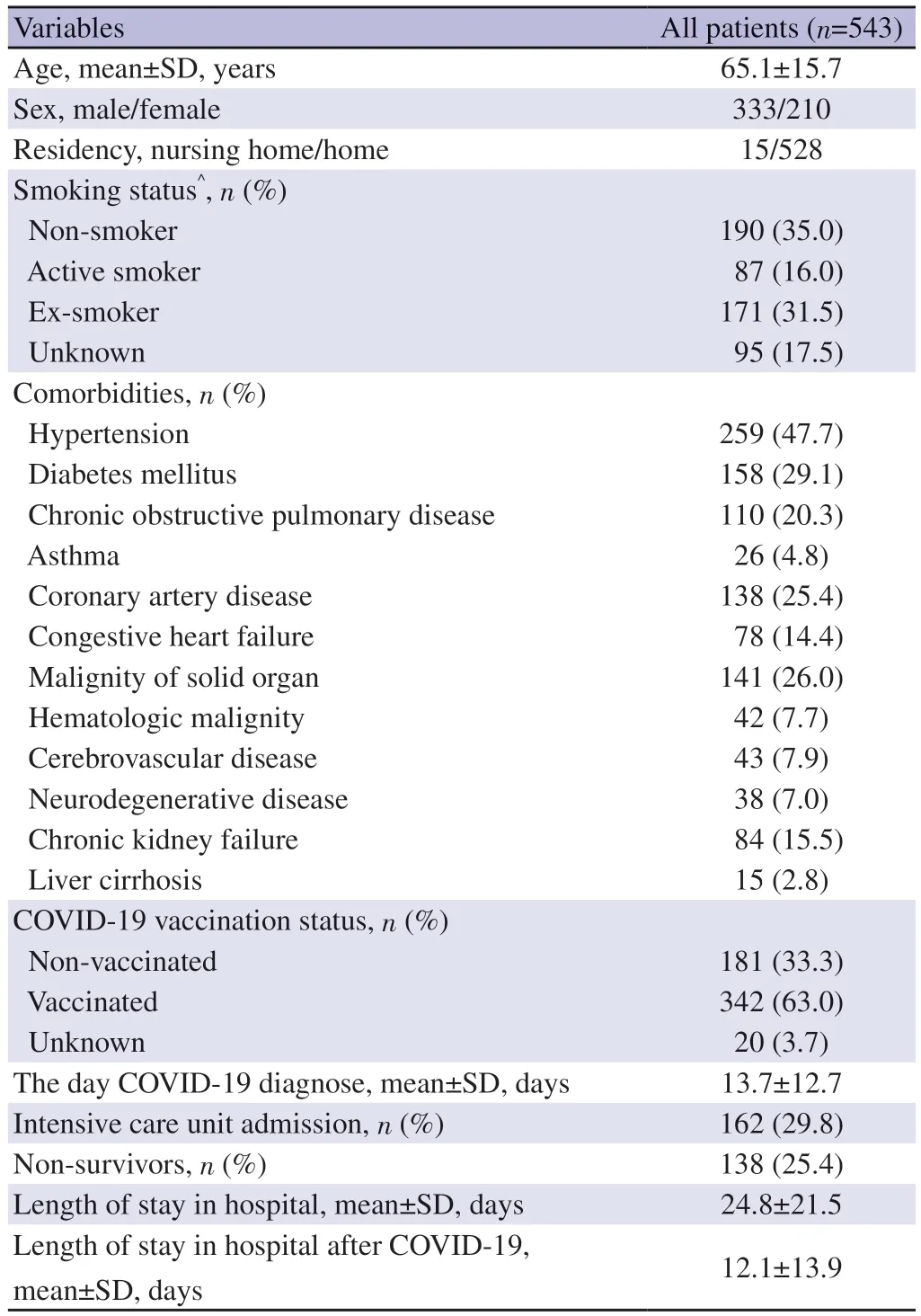
Table 1.Demographic characteristics of patients with nosocomial COVID-19.
Among the 543 nosocomial COVID-19 patients who followed pandemic services, 106 (19.5%) patients transferred from surgical wards and 437 (80.5%) patients were transferred from medical wards.Most patients transferred to pandemic services were from pulmonology wards (n=183, 33.7%) and internal medicine wards(n=176, 32.94%).Nosocomial COVID-19 patients from medical wards were older and had more comorbid diseases than surgical patients (mean ages were 66vs.60 years,P=0.001).The time from admission to PCR positivity was longer in medical ward patients than in surgical patients (median 14vs.10 days,P=0.023) (Table 2).
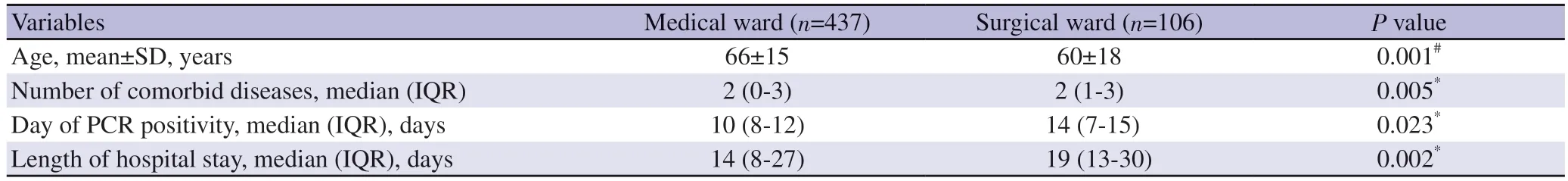
Table 2.Comparison of surgical and medical patients with nosocomial COVID-19.
A total of 342 (63.0%) patients were vaccinated, 181 (33.3%)patients were non-vaccinated, and the vaccination status of 18(3.3%) patients was unknown.The demographic and clinical characteristics of vaccinated and non-vaccinated patients were similar, except that the vaccinated patients were older.Intensive care unit (ICU) admission and mortality rates were lower in vaccinated patients (24.9% vs.42.5%, P<0.001 and 17% vs.43.1%, P<0.001,respectively), despite the fact that vaccinated patients were older than non-vaccinated patients [mean age (65±14) years vs.(60±18)years, respectively,P=0.008] (Table 3).
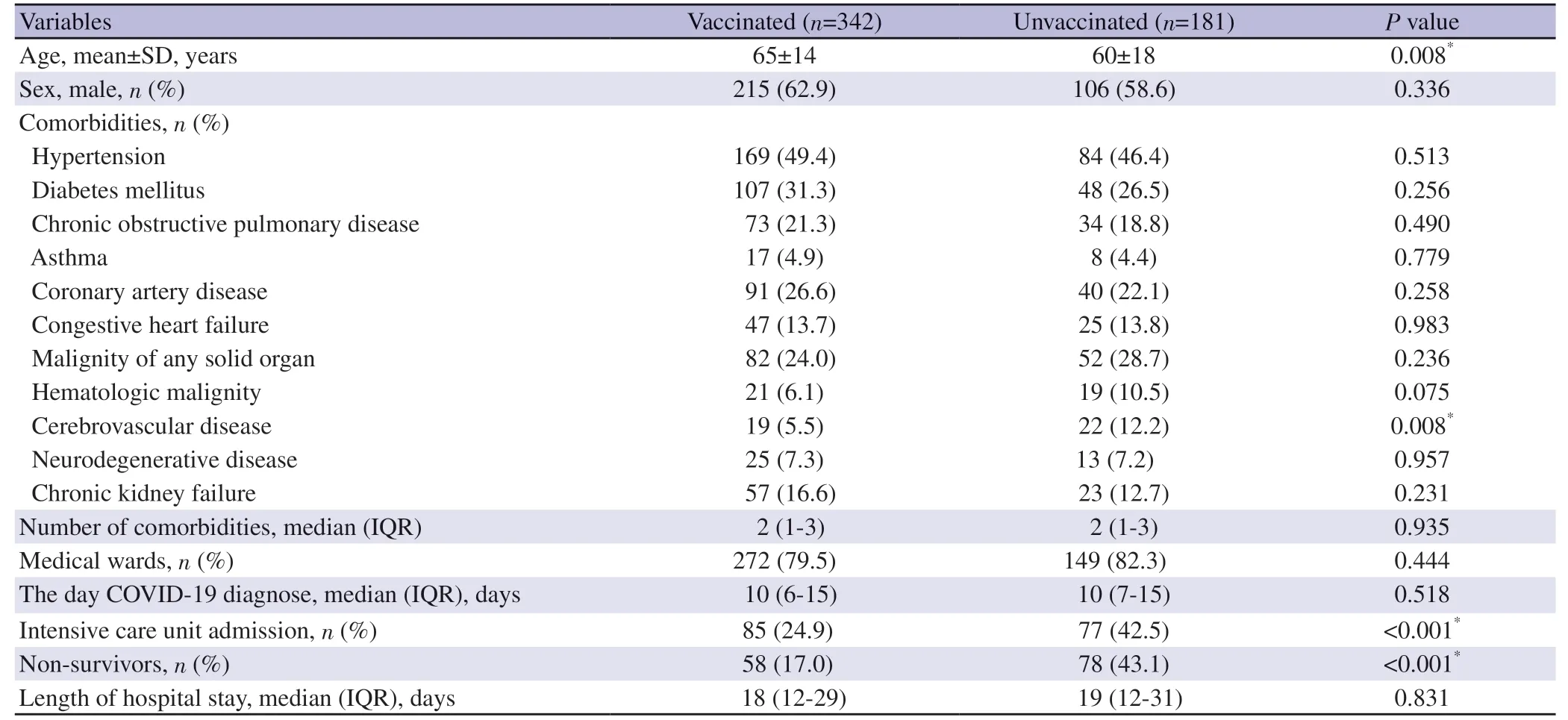
Table 3.Comparison of vaccinated and unvaccinated nosocomial COVID-19 patients.
The mean length of hospital stay was (24.8±21.5) days, and the mean length of pandemic service was (12.2±13.9) days.162(29.8%) nosocomial COVID-19 patients admitted to ICU due to disease severity and 138 (25.4%) dead during hospital stay.
Advanced age (≥65 years), vaccination status, and comorbid conditions such as cerebrovascular disease, neurodegenerative disease, and chronic kidney failure were associated with higher mortality (Table 4).
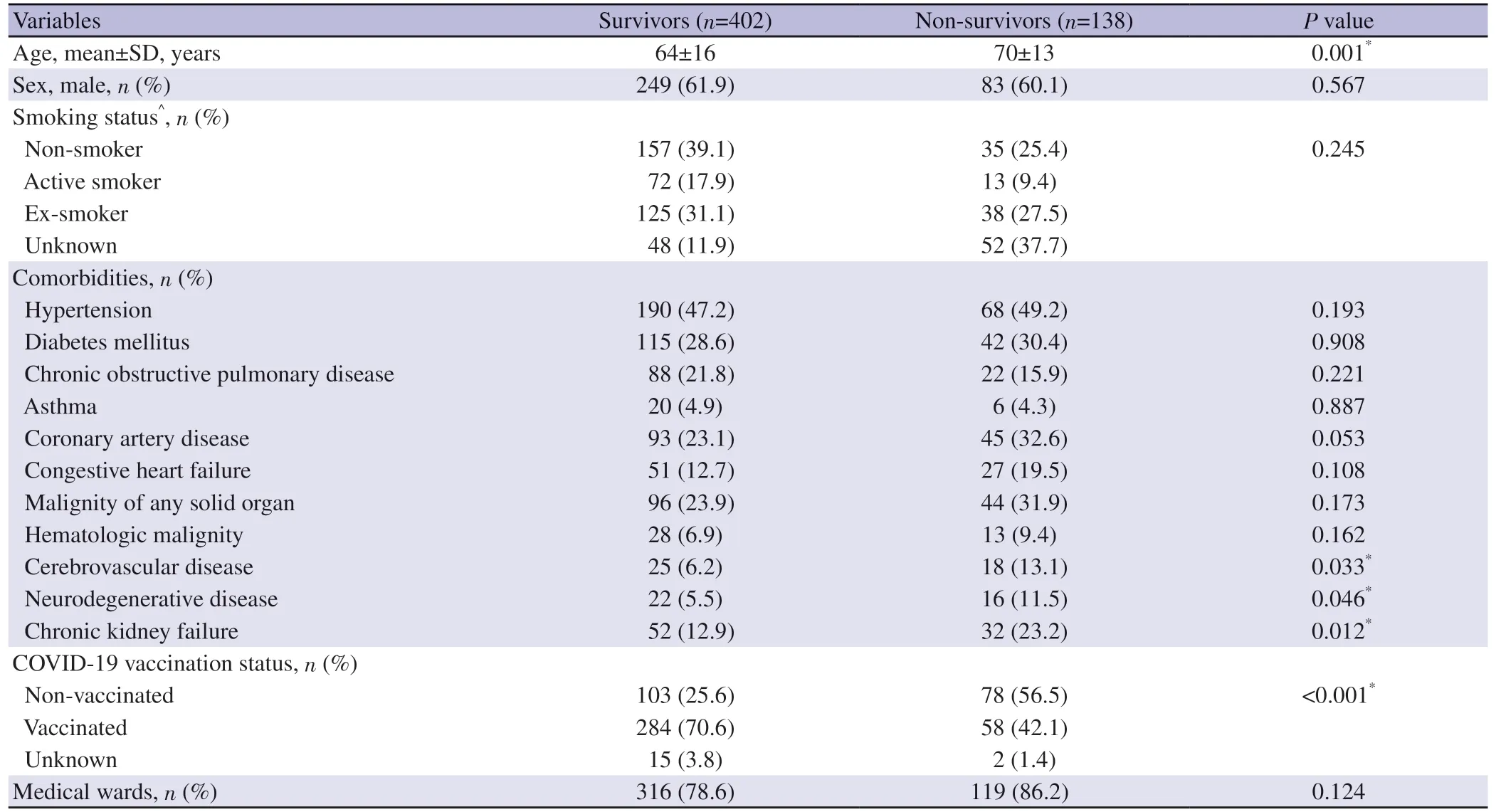
Table 4.Comparison of survivors and non-survivors with nosocomial COVID-19.
Advanced age (≥65 years) and the number of comorbid diseases(≥2) were found to be independent risk factors for mortality in multivariate regression analysis (OR1.74, 95%CI1.11-2.74 andOR1.60, 95% CI 1.02-2.56, respectively).Vaccination decreased the risk of mortality in nosocomial COVID-19 patients (OR0.25, 95% CI 0.16-0.38, P<0.001) (Table 5).
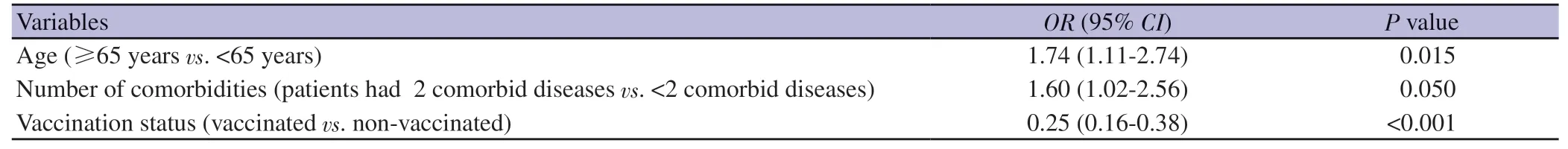
Table 5.Multivariate regression analysis for mortality.
4.Discussion
COVID-19 is a contagious disease that can be transmitted quickly from one person to another.Hospitals are one of the most susceptible places to infection, despite all preventive measures to limit disease spread.During the study period, 15573 COVID-19 patients were followed in 18 centers, and 543 (3.5%) were nosocomial COVID-19 patients.The majority of nosocomial COVID-19 patients (80.4%) were from medical wards.One-third of nosocomial COVID-19 patients required ICU admission, and 138(25.4%) of them died during their hospital stay.Vaccination against COVID-19 was associated with fewer intensive care requirements and decreased mortality.
The incidence of hospital-acquired SARS-CoV-2 infection varies widely from 0% to 65%[5,10].Readet al.reported that 11.6% of COVID-19 patients became infected after hospital admission in the United Kingdom[11].In a study conducted in the UK and Italy, 12.5% of hospitalized COVID-19 patients were hospitalacquired SARS-CoV-2 infection[3].In a meta-analysis that included 8251 COVID-19 patients, 1513 (18.3%) of them were defined as probable or definite nosocomial COVID-19.The rate of nosocomial COVID-19 was lower in our study than in previous studies conducted in the pre-vaccination era; while our study was performed during the mass vaccination era in Turkey.Vaccination may have caused a lower rate of nosocomial COVID-19 in our study.Another reason is that the increased awareness of nosocomial COVID-19 over time and the implementation of prevention measures may have caused the nosocomial COVID-19 rate to be lower.
Lower estimated rates of hospital-acquired SARS-CoV-2 infection were observed in surgical wards, and higher estimated rates of hospital-acquired SARS-CoV-2 infection were observed in longterm care facilities, hemodialysis centers, and general wards[6].Advanced age, number of comorbidities, and length of hospital stay were associated with nosocomial COVID-19[3,12-14].The vast majority of nosocomial COVID-19 patients (80.4%) were from medical wards in the current study.In our study, patients who followed up in the medical wards were older and had more comorbid conditions than patients who followed up in the surgical wards, which was considered the main reason for this situation.
The association between worse outcomes, such as admission to the ICU or mortality, and nosocomial COVID-19 is controversial.Khan et al.reported that there was no significant difference in 30-day mortality between nosocomial COVID-19 and communityacquired COVID-19[15].In a multi-center study conducted in the United Kingdom and Italy, the mortality rate for nosocomial COVID-19 was found to be lower than that of community-acquired COVID-19[3].These two studies were published early-term in the outbreak.In contrast with these studies, the mortality rate was found to be higher in nosocomial cases than in community-acquired cases in studies in the late stages of outbreak[2,8].The risk of mortality was found 1.3 times greater in nosocomial COVID-19 patients than in community-acquired COVID-19 patients in a meta-analysis[7].The mortality rates of hospitalized COVID-19 patients varied from 2.3% to 7.3%, and ICU admission rates varied from 6.3% to 11.5% in Turkey[16-18].In our study, 162 (29.8%) patients with nosocomial COVID-19 were admitted to the ICU, and in-hospital mortality rate was 25.4%.Advanced age (≥65 years) and the number of comorbid diseases (≥2) increased the risk of in-hospital mortality in nosocomial COVID-19 patients.Advance age and the number of comorbidities were well-defined risk factors for mortality in COVID-19 patients[19,20].These factors are also risk factors for nosocomial COVID-19 patients.Therefore, a higher mortality rate in nosocomial COVID-19 patients is expected.
Vaccination was found effective against the development of severe disease in randomized controlled trials and nationwide studies[21-24].Whittaker et al.reported that vaccinated patients also had a lower risk of ICU admission when compared to unvaccinated patients, but there was no difference in in-hospital mortality[25].We found that vaccination against SARS-CoV-2 decreased the risk of mortality in nosocomial COVID-19 patients.The results of our study were consistent with the results of previous studies.In previous studies,vaccination has been shown to reduce mortality in COVID-19 patients requiring hospitalization[26-28].
Our study has several limitations.Firstly, this was a retrospective study, and patients in our cohort were transferred to pandemic services due to nosocomial COVID-19, so we could not determine the true incidence of nosocomial COVID-19 and could not evaluate risk factors for nosocomial COVID-19.Secondly, since we did not compare patients with nosocomial COVID-19 and communityacquired COVID-19 for in-hospital mortality, it is difficult to associate nosocomial COVID-19 with higher mortality.Thirdly,we could not determine whether the source of transmission is from relatives of patients or health workers due to the higher prevalence of COVID-19 during study periods.
Despite the limitations, our study included several centers in the study, so our results can be generalized to Turkey.Our results show that vaccination against SARS-CoV-2 is protective against admission to the ICU and mortality in nosocomial COVID-19.Hospitalized patients are at risk of COVID-19 transmission,especially patients who followed up in medical wards.Vaccination against SARS-CoV-2 decreases the need for ICU admission and inhospital mortality in patients with nosocomial COVID-19.
Conflict of interest statement
The authors declare that they have no conflict of interst.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
We thank the Turkish Thoracic Society for stimulating our interest in this research.
Funding
The authors received no extramural funding for the study.
Authors’ contributions
SY, CY, and ÖE designed the study; CY, GP, SAB, İB, İK, CA,MB, HB, GO, EO, EC, AKÇ, DT, MG, SK, YA, AE, YO, BBY, BG,DDY, EYON, RE, ATE, MMT, FF, MÇ, ME, and AT collected the data; SY, GP and ÖE analyzed the data; SY, and CA, searched the literature and wrote the manuscript; ÖE edited and controlled the final version of the manuscript.All the authors approved the final version of the manuscript.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Clinical profile, etiology, management and outcome of empyema thoracis associated with COVID-19 infection: A systematic review of published case reports
- Diversity and species composition of microbiota associated with dengue mosquito breeding habitats: A cross-sectional study from selected areas in Udapalatha MOH division, Sri Lanka
- Molecular evidence and phylogenetic delineation of spotted fever group Rickettsia species in Amblyomma ticks from cattle in Gauteng and Limpopo Provinces, South Africa
- Cutaneous anthrax associated with facial palsy: A case report
- Healthcare-associated Staphylococcus aureus infections in children in Turkey: A sixyear retrospective, single-center study