Clinical profile, etiology, management and outcome of empyema thoracis associated with COVID-19 infection: A systematic review of published case reports
2023-10-10YasserAliKamalSehamAbdelwakeelAbdelGaber
Yasser Ali Kamal, Seham Abdelwakeel Abdel-Gaber
1Department of Cardiothoracic Surgery, Faculty of Medicine, Minia University, El-Minya, Egypt
2Department of Medical Pharmacology, Faculty of Medicine, Minia University, El-Minya, Egypt
ABSTRACT
Objective: To explore the clinical features, diagnosis, etiology,treatment, and outcomes of COVID-19 related empyema.
Methods: Using PRISMA statement, a systematic search of relevant case reports published between December 2019 and April 2023 was performed through seven databases.The collected data included demographics, clinical manifestations, diagnostic findings,treatment, and outcomes.
Results: Thirty-six case reports were identified with 43 cases of empyema.The included cases had a median age of 55 years (range:12-78 years) and 79.1% (34/43) were males.The majority of cases presented during hospitalization for management of acute COVID-19 infection (29/43, 67.4%) and Charlson comorbidity index <3 (40/43,93.0%).Pseudomonas aeruginosa was the most commonly isolated microorganism from the pleural fluid (9/43, 20.9%) and 16.3% of the cases (7/43) had polymicrobial infections.Chest drainage was performed in all cases while surgery was indicated in 24 cases(55.8%).The most common complication of COVID-19-related empyema was broncho-pleural fistula (2/43, 4.7%).The mortality rate was 23.3% (10/43).Sepsis and/or multi-organ failure were the most commonly reported causes of death.On univariate analysis, no statistically significant risk factor for mortality was identified.
Conclusions: COVID-19-associated empyema has a variety of predisposing factors, time of presentation, clinical features, and causative organisms.Invasive or minimally invasive surgical procedures are performed more frequently than isolated chest drainage.Empyema in COVID-19 patients worsens their prognosis and can lead to serious complications.
KEYWORDS: COVID-19; SARS-CoV-2; Empyema;Microbiology; Thoracic surgery
Significance
This review addressed the question of whether the coexistence of COVID-19 pneumonia and empyema could affect treatment and outcome.Although rare, pleural empyema can complicate COVID-19, particularly in patients with diabetes mellitus,bronchopleural fistula, persistent air leak, or prolonged ICU stay.Hospital-acquired bacterial co-infection was the most common cause.Death was reported in more than a fifth of cases.In more than half of the cases, surgical decortication was performed.Empyema in COVID-19 patients reflects serious bacterial or fungal co-infection with severe illness.Early management of pleural complications is essential in viral respiratory infections.
1.Introduction
As of May 2023, there have been 687384719 confirmed cases of novel coronavirus disease of 2019 (COVID-19) worldwide,including 6868536 deaths, since the first reported case[1].
Clinically, COVID-19 is associated with a variety of symptoms due to viral immune dysfunction and tissue damage[2,3].Pleural complications such as pneumothorax, pleural effusion, and pleural empyema are rarely seen in COVID-19 pneumonia[4].All patients with pneumonia or sepsis of unknown cause should be evaluated for pleural effusion[5,6].A parapneumonic pleural effusion may be complicated by bacterial invasion of the pleura or develop into empyema, which is associated with high morbidity and mortality[7].Initial treatment of pleural empyema with antimicrobial therapy depends on the results of pleural fluid culture and the etiology of the empyema, whether acquired in the community or in the hospital.Successful treatment is usually achieved by early drainage and, if necessary, surgical decortication[8].
The incidence of pleural effusions in patients with COVID-19 pneumonia is approximately 7% and it is common in critically ill patients[9].Parapneumonic pleural effusion can be complicated by the invasion of microorganisms into the pleural fluid, followed by empyema, a life-threatening condition that occurs in three progressive stages: exudative, fibrino-purulent, and organizing.Complicated pleural effusions and empyema can exacerbate the unfavorable consequences of pneumonia[10].The aim of this systematic review was to explore the published case reports of COVID-19 related empyema in terms of their clinical features,diagnosis, etiology, treatment, complications, and mortality.
2.Materials and methods
2.1.Search strategy
This study was designed in accordance with the PRISMA 2020 statement for reporting systematic reviews[11].We conducted a systematic search on 18th April 2023, in PubMed, Ovid, Web of Science, and Scopus databases.Additional search in COVID-19 literature was carried out using iSearch COVID-19 portfolio, WHO COVID-19 Research Database, and LitCovid.The search terms were “COVID-19”, “Coronavirus disease”, "severe acute respiratory syndrome coronavirus 2", "2019 ncov", "sars cov 2", and "empyema"(Supplementary S1).
2.2.Eligibility criteria and assessment of quality
Case reports/series in English language which reported patient information, clinical features, diagnostic findings, treatment modalities and outcomes of empyema thoracis during hospitalization or recovery phase of COVID-19 infection were included.Cases of COVID-19 without empyema, autopsy studies, animal studies, poorquality case reports, commentaries, and cases of chronic empyema prior to the COVID-19 pandemic were excluded.To estimate the quality of the included case reports, Joanna Briggs Institute' (JBI)critical appraisal checklist for case reports was used.
2.3.Data extraction
The authors performed data extraction independently.The extracted data included article information, patient demographics, clinical manifestations, past medical history, co-morbid conditions, results of laboratory tests, findings on physical examination, relevant findings of imaging studies, results of cultures (pleural, blood, urine,tissue, or bronchoalveolar lavage), mode of treatment, reported cause of empyema, complications of empyema, complications after surgical treatment of empyema, and in-hospital outcome.Charlson comorbidity index (CCI) was calculated by the authors from the reported comorbidities as previously described[12].Early presentation of empyema was considered when it was diagnosed during hospitalization for treatment of acute COVID-19 infection.Delayed presentation of empyema refers to identification of empyema after resolution of COVID-19 pneumonia or negativity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) at time of diagnosis.
2.4.Statistical analysis
Data analysis was performed using IBM SPSS Statistical Software Version 25.0 (IBM Corp., Armonk, NY) and R Version 4.1.3 (R Foundation for Statistical Computing, Vienna, Austria).Categorical variables were expressed as counts and percentages, while continuous variables were expressed as mean, standard deviation,median and range.Categorical data were compared using theChisquare (χ2) test or Fisher's exact test, and continuous variables were compared using t-test or Mann-Whitney test as proper.A P-value≤0.05 was statistically significant.
3.Results
An initial database search identified 1052 articles, of which 36 case reports with 43 cases[13-48] were included in the final analysis(Figure 1).
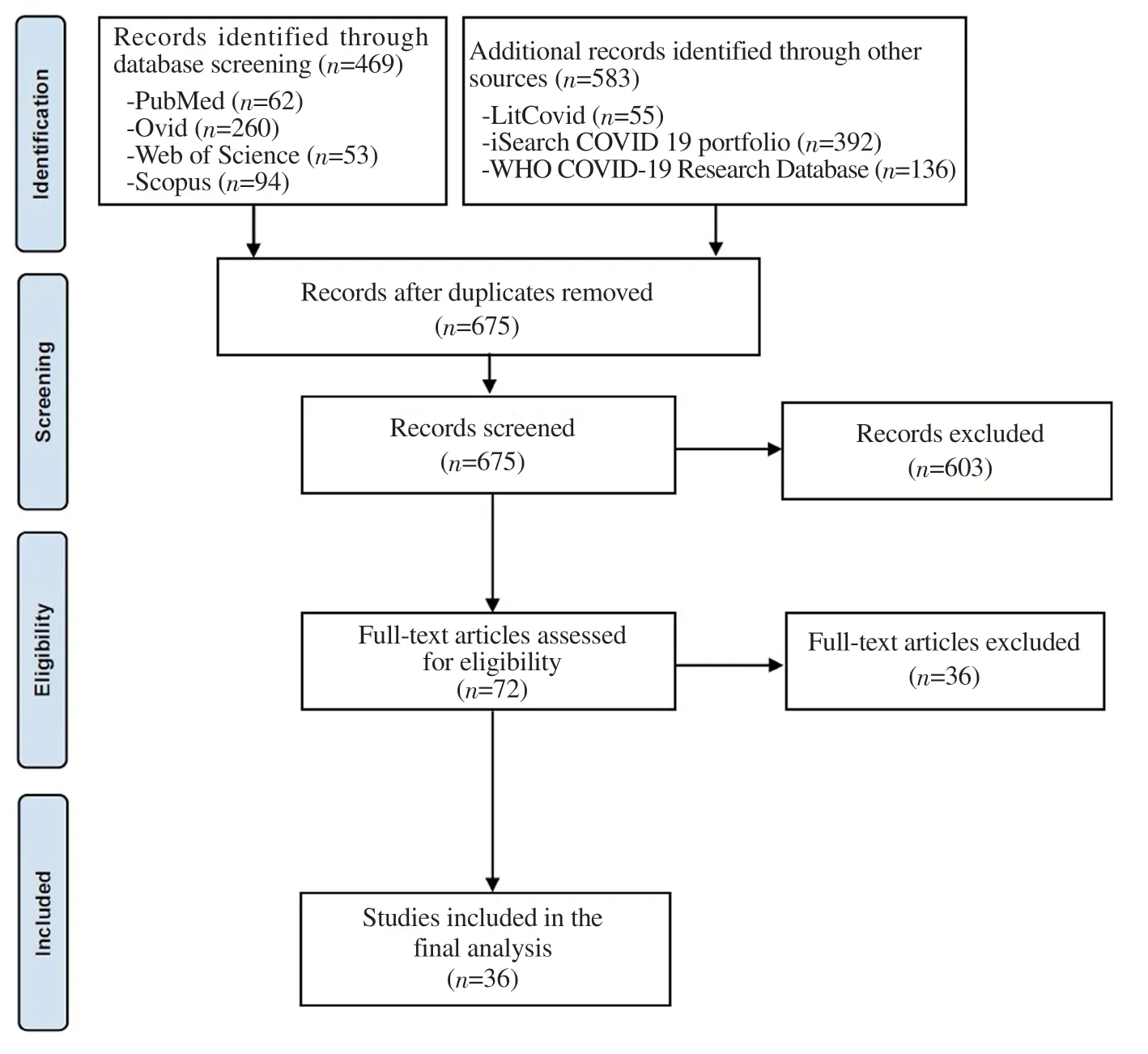
Figure 1.PRISMA checklist flow diagram of the included studies.
3.1.Patient characteristics and co-morbid conditions
Demographic and clinical characteristics are summarized in Table 1.The median age was 55 years (range: 12-78) and 60.5% (26/43) of cases were over 50 years old.The patients were mostly men (34/43;79.1%).Comorbidities were reported in 24 patients (55.8%) and 16 patients (37.2%) had two or more comorbidities.Diabetes mellitus was the most frequent comorbidity (17/43; 39.5%).

Table 1.Demographic and clinical characteristics of 43 cases with COVID-19 related empyema and its corresponding prognosis [n (%)].
3.2.Clinical presentation
Respiratory distress (dyspnea, shortness or difficulty of breathing)was the most common initial clinical manifestation (15/43; 34.9%).Bronchopleural fistula (BPF) was associated with empyema in 5 cases (11.6%).Three of the reported cases (7.0%) had empyemaafter removal of extracorporeal membrane oxygenation (ECMO).Most of the reported cases had unilateral empyema (90.7%).Most cases developed empyema during the acute phase of COVID-19 infection (29/43; 67.4%).
3.3.Diagnostic workup
Diagnosis of empyema was based mainly on the results of pleural fluid analysis and culture in addition to imaging studies or operative findings.Imaging of pleural empyema included chest computed tomography (CT) in 38 cases (88.4%) and chest ultrasound in 5 cases (11.6%).Early inflammatory markers of COVID-19 infection were outside the reference range in most reported cases (Table 2).

Table 2.Reported initial inflammatory markers in cases with COVID-19 related empyema.
3.4.Etiology of empyema
The underlying causes and isolated causative organisms from the pleural fluid are presented in Figure 2.Bacterial empyema had the highest frequency (17/43, 39.5%), followed by fungal (10/43,23.3%) and culture-negative empyema (6/43, 14.0%).Aside from microbiological causes, the reported underlying causes of COVID-19-related empyema included infected hydropneumothorax (1/43,2.3%), infected hemothorax (1/43, 2.3%), ruptured splenic tubercular abscess (1/43, 2.3%), ruptured pneumatocele (1/43, 2.3%), aspiration(1/43, 2.3%), bronchopleural fistula (3/43, 7.0%), and alvelopleural fistula (3/43, 7.0%).
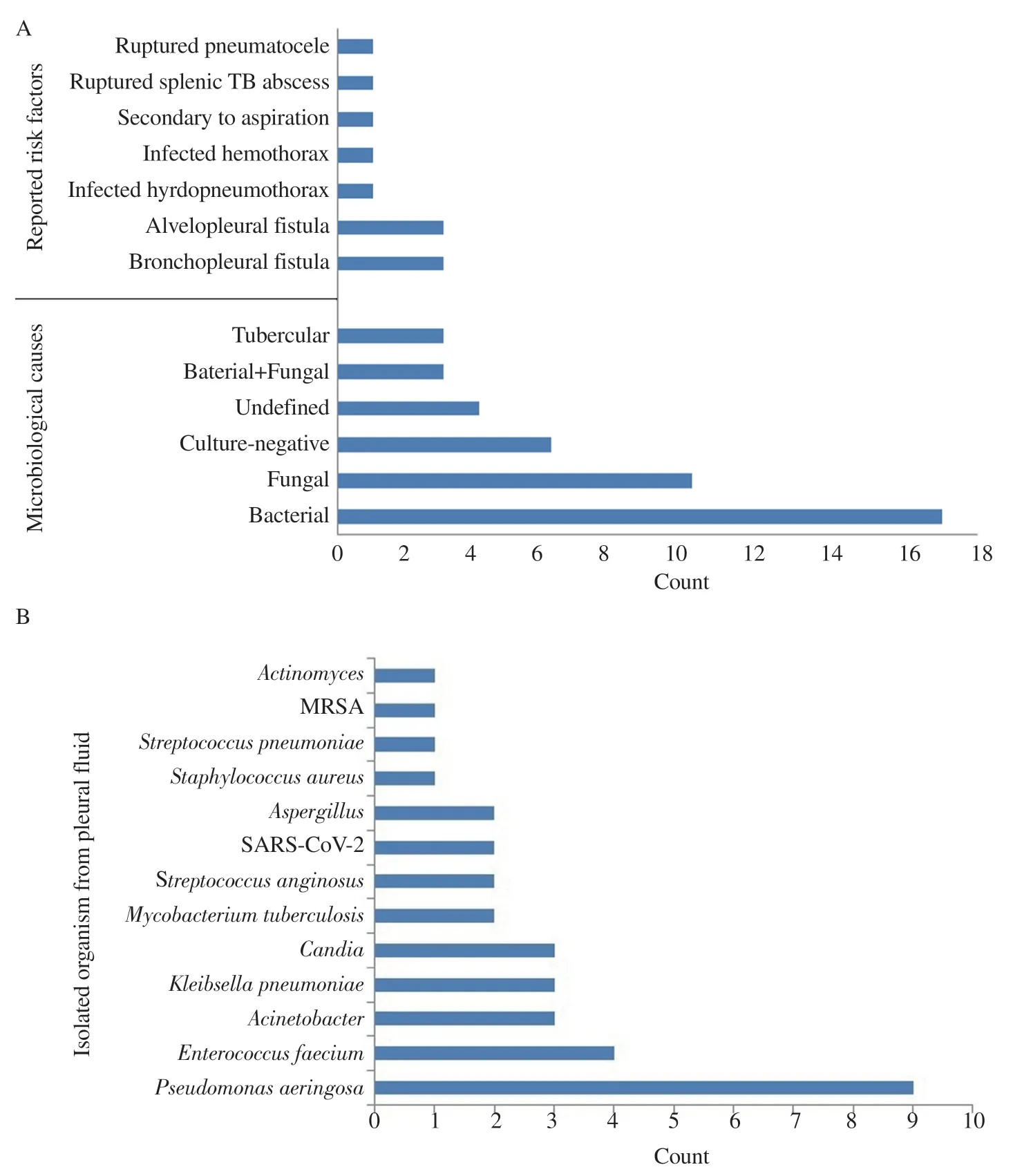
Figure 2.Reported underlying causes (A) and isolated microorganisms from the pleural fluid (B) in cases with COVID-19 related empyema.MRSA:Methicillin-resistant Staphylococcus aureus.TB: tuberculosis; MRSA: methicillin-resistant Staphylococcus aureus; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2.
The most frequently isolated microorganisms from the pleural fluid were Pseudomonas (P.) aeruginosa (9/43; 20.9%), followed by Enterococcus faecium (4/43; 9.3%), Acinetobacter species (3/43;7.0%),Klebsiella pneumoniae(3/43; 7.0%), andCandidaspecies(3/43; 7.0%).Mycobacterium, SARS-CoV-2,Streptococcus anginosus,and Aspergillus were isolated in 2 cases (4.7%) for each organism.Staphylococcus aureus, Streptococcus pneumoniae, methicillin-resistantStaphylococcus aureus(MRSA), andActinomycesare isolated in one case only (2.3%).The results of tissue/wound culture were reported in 6 cases (14.0%) including in 5 cases (11.6%) positive for Mucor which was isolated from lung tissue/wound cultures and Rhizopus species in one case (2.3%).
3.5.Treatment
In addition to the standard treatment of COVID-19 pneumonia,specific antimicrobial therapies were reported.Different therapies for empyema are presented in Table 3.The most commonly prescribed antibiotic was vancomycin (10/43; 23.3%) and meropenem (10/43;23.3%).Amphotericin B was the most commonly prescribed antifungal drug (3/43; 7.0%).Chest drainage was performed in all cases.It was the only mode of non-medical treatment in 15 cases(34.9%).Other non-medical interventions included debridement/decortication (21/43; 48.8%), lung resection (9/43; 20.9%),intrapleural fibrinolysis (4/43; 9.3%), repair of BPF (3/43; 7.0%),open window thoracostomy (1/43; 2.3%), and thoracoplasty (1/43;2.3%).Video-assisted thoracoscopic surgery was reported for debridement/decortication in 6 cases (14.0%).
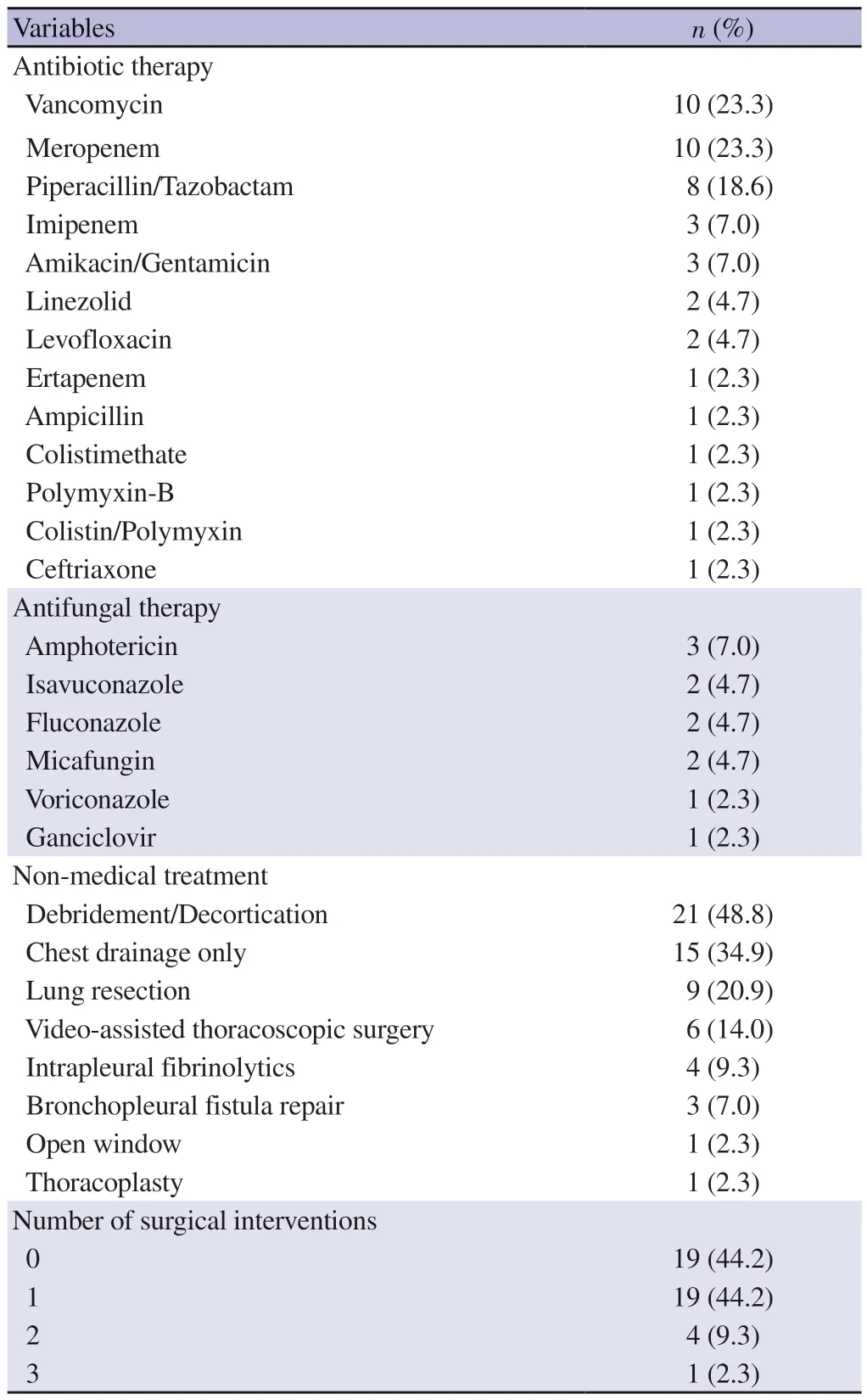
Table 3.Medical and non-medical treatment of 43 cases with COVID-19 related empyema.
3.6.Outcomes
Adverse outcomes in cases with COVID-19 related empyema are listed in Table 4.The mortality rate in this systematic review of case reports is 23.3% (10/43).On univariate analysis, we did not determine a statistically significant risk factor for mortality (Table 5).Further multivariate analysis of the predictors of mortality is limited by the small number of reported cases.
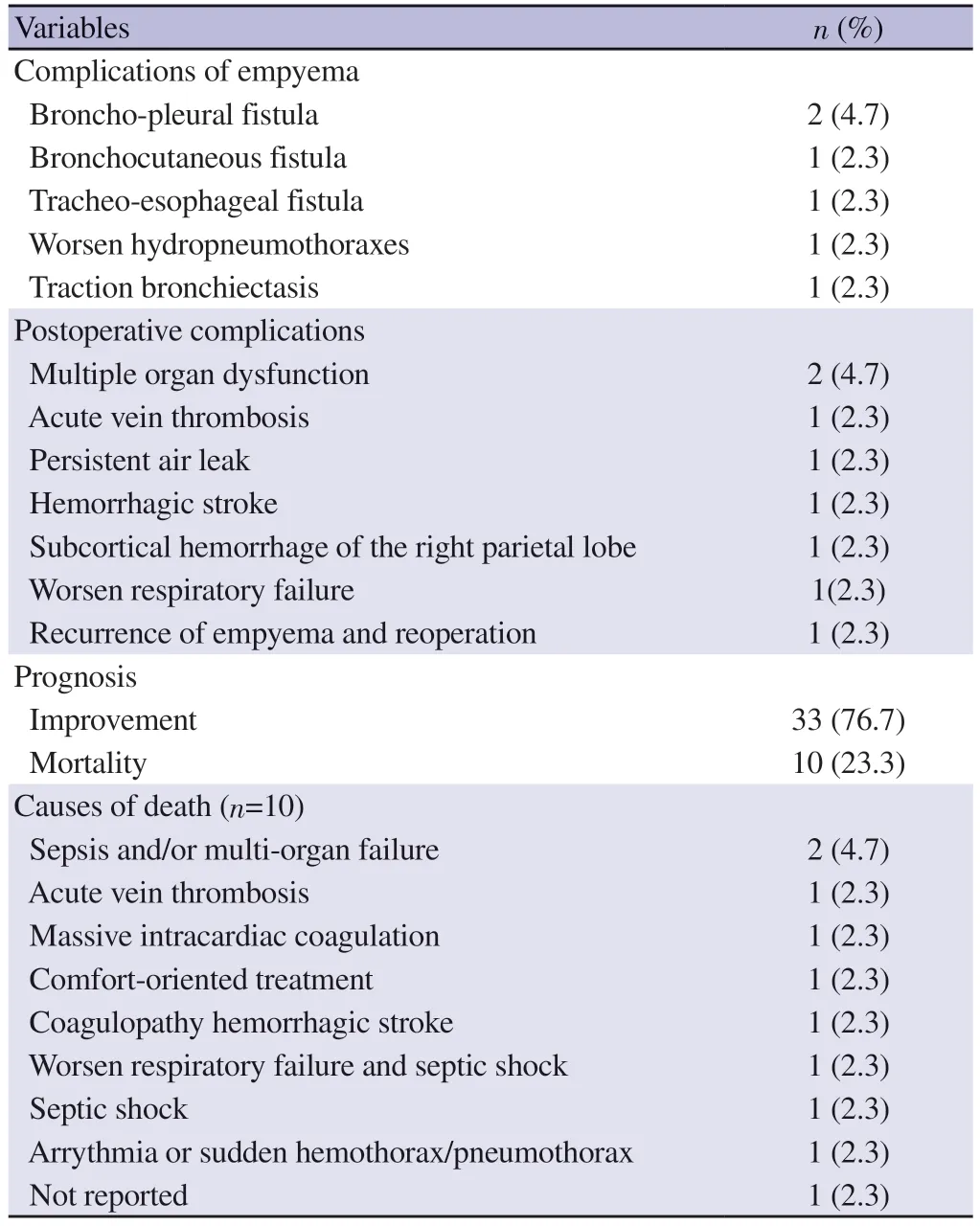
Table 4.Adverse outcomes in 43 cases with COVID-19 related empyema.

Table 5.Results of univariate analysis of risk factors for mortality [n (%)].
4.Discussion
This systematic review demonstrates that empyema thoracis is a rare but serious complication during the early or late phases of COVID-19 infection.Empyema, defined by the presence of pus or microorganism in the pleural fluid, is a well-known complication of pneumonia with a mortality rate approximating one-fifth of the affected cases[49].Empyema in COVID-19 patients has been documented only in case reports except for one retrospective study reporting an incidence of 4.2% for empyema with COVID-19 in the same episode[50].
4.1.Patient characteristics and co-morbid conditions
The reported age (12-78 years) is consistent with the age of patients with COVID-19 and pleural effusion (7.9 to 70 years).In addition,pleural effusions are more common in patients with COVID-19 who are older than 50 years[9].Most of the reported cases were male patients (79.1%).It has been previously reported that empyemais twice as common in males[8].Additionally, the high proportion of male patients with empyema was similar in the pre- and post-COVID periods[50].
The most common comorbidity was diabetes mellitus.Diabetes mellitus is considered as one of the most important risk factors for severe COVID-19 disease, as diabetic patients usually have other comorbidities[51].
4.2.Clinical presentation
The lack of specific clinical features for empyema with COVID-19 may lead to a difficult or missed diagnosis.Moreover, the similarity in the clinical manifestations increased the possibility of serious empyema complications, clinical deterioration, delayed surgical management, and death.The presence of BPF has an important clinical association with pleural empyema especially in patients with lung resection, necrotizing pulmonary infection, or persistent spontaneous pneumothorax.
The underlying causes of BPF and empyema in COVID-19 patients were necrotizing pulmonary infection in the presence of mucormycosis[14,39], prior pneumonectomy[21], or air cysts[22].Interestingly, ECMO is another important risk factor for the development of empyema.Patients with ECMO had prolonged intensive care unit (ICU) stay for management of acute respiratory distress syndrome with unusual causative organisms of empyema includingEnterococcus faeciumandShewanella[18,44,45].Thus,bloodstream infections during ECMO in COVID-19 patients should be considered, especially with clinical deterioration despite adequate treatment.
The majority of cases had unilateral empyema, consistent with the finding that most pleural effusions in COVID-19 patients are unilateral[52].Bilateral empyema is a rare entity in COVID-19 patients (9.3%) but it can occur secondary to bilateral infected hydropneumothorax related to lung cavitation, obstruction of the small airways by inflammatory exudate[30], or infiltration of bilateral peripheral lung opacities to the pleura[17].These cases indicate early treatment of COVID-19 related air leak or pneumothrax and reflect that both SARS-CoV-2 and nosocomial pathogens are initial causes of increasing the risk of hydopneumotharx and complicated pleural effusions.
The delayed presentation of empyema (34.2%) demonstrates the importance of continuous monitoring of COVID-19 patients who do not experience clinical improvement during hospitalization[26].Treatment of empyema during the early acute phase of COVID-19 is challenging due to the similar clinical features of both entities.Empyema also increases the medical challenge because it requires a combination of medical treatment, ventilation, and surgery.
4.3.Etiology of empyema
This review showed high frequency of bacterial empyema that can be explained by high incidence rate of secondary bacterial infection in COVID-19 patients, ranging from 3.7% to 41.9%[53],which has been reported as an additional risk factor for mortality[54].Bacterial empyema in COVID-19 patients may be related to the disease process or antimicrobial resistance due to over-prescription of antibiotics[46].Interestingly, culture-negative has been reported in 14.0% of the included cases in this review particularly in autoimmune or immunocompromised patients, and those with previous extensive antibiotic exposure[25].
Unusual underlying causes of COVID-19-related empyema in this review included infected hydropneumothorax, infected hemothorax, ruptured pneumatocele, and alvelopleural fistula.The pathogenesis of these causes may be related to the pathogenic mechanisms or therapy of COVID-19 including: 1) thrombosis of interstitial blood vessels, followed by parenchymal necrosis, loss of tissue elasticity and pneumothorax[30]; 2) infected hemothorax related to anticoagulant use as a part of COVID-19 treatment such as Dabigatran[20]; 3) long-term corticosteroid use; 4) rupture of pneumatocele associated with bacterial co-infection[38]; 5) persistent air leaks caused by alveolopleural fistulas[43].
The isolated organisms from the pleural fluid includedPseudomonas,Klebsiella,Acinetobacter,Enterococci,Staphylococcusaureus, and MRSA which commonly account for hospital-acquired empyema, while Streptococcus species account for most of the isolates from community-acquired empyema[8].P.aeruginosais a leading cause of hospital-acquired pneumonia, particularly due to prolonged endotracheal intubation, previous broad-spectrum antibiotic therapy, and immunocompromised status[24].In addition,both P.aeruginosa and COVID-19 infections can cause cavitary lung lesions, so the combination of both infections increases the risk of empyema subsequent to lung cavitation[55].
Empyema due to Enterococcus species is uncommon entity and it has been primarily linked with intra-abdominal infections and often found in patients with impaired immune system.Moreover, the natural resistance of Enterococcus to several types of antibiotics can lead to unusual cases of empyema[56].In this review, enterococcal empyema was not correlated with intra-abdominal infection in patients with COVID-19 and it was reported after ECMO in patients initially treated with interleukin-6 (IL-6) antagonists and tocilizumab[18,45].
Acinetobacter baumannii is a Gram-negative organism that causes nosocomial infections in ICU patients and is highly resistant to antibiotics, particularly in those with immunocompromised status, immunosuppressant therapy, respiratory failure, and sepsis.These risk factors with bacterial coinfection and subsequent pyopneumothorax increase the risk of mortality in COVID-19 patients[48].Klebsiella pneumoniae is the second most common respiratory pathogen isolated from COVID-19 patients particularly in those with invasive infections.Co-infection ofKlebsiella pneumoniae,Cytomegalovirus, Aspergillus, and Zygomycete has been reported in a patient with COVID-19 and empyema[40].
Candidaspecies have been reported as causes of empyema in COVID-19 patients, including Candida albicans and Candida glabrata.Generally, Candida and other causes of fungal empyema are commonly seen in patients with immunocompromised status, severe underlying illnesses or malignancies, underlying comorbidities, sepsis, ICU stay, prolonged antibiotic therapy, and intra-abdominal diseases[17,31,42].Concomitant bacterial empyema is common in patients with fungal empyema[42].Tubercular empyema was reported in 2 cases of COVID-19.One case had a lung abscess and fungal infection[23] and another case had a ruptured splenic tuberculosis abscess[35].Although it is unlikely that a patient with tuberculosis will get COVID-19, tuberculosis and COVID-19 can co-exist.
Detection of SARS-CoV-2 in pleural fluid in 2 cases with COVID-19, bacterial co-infection, and superimposed empyema highlights the increased risk of self-quarantine and delayed treatment for the management of high-risk patients[16].Interestingly, a rare case of non-nosocomial MRSA infection in an outpatient with COVID-19 highlights the importance of early diagnosis and treatment of COVID-19 and its variants, which can serve as a preventive measure against its complications[32].
Mucorwas isolated in 11.6% of the reported cases.Mucormycosis is an angioinvasive fungal infection that can infect humans through inhalation which transmits spores to the lung or paranasal sinuses.Mucormycosis has been found in less than 1% of hospitalized COVID-19 patients with an increased risk in immunocompromised patients[33,39].In addition, mucormycosis can lead to necrotic infection with subsequent development of bronchopulmonary fistula and empyema[14].
4.4.Treatment
Regarding medical treatment, the shift from empiric antibiotic therapy to organism-specific antimicrobial therapy was reported after confirmation of the causative organism.The high percentage of prescribed vancomycin and meropenem may be related to their empiric use for suspected hospital-acquired infections.
Antifungal therapies were less commonly prescribed than antibiotics.There is no evidence favoring one antifungal agent for the treatment of fungal empyema.Despite the better penetration of azoles (voriconazole and fluconazole) to the pleural fluid than echinocandin or amphotericin B, some species associated with resistance to fluconazole[42].The choice of antifungal drug is also influenced by the causative organism and the spread of the fungal infection.Fluconazole is used as an adjunct to pleural drainage to treatCandidaempyema, echinocandin has been recommended as the drug of choice for treating candidemia[57], and liposomal amphotericin B has been used in combination with surgery to treatMucor[33].
Chest drainage was performed in all cases while surgery was indicated in 55.8% of cases.According to the American Association of Thoracic Surgeons, if empyema is diagnosed, a tube thoracostomy should be performed followed by surgery if necessary[5].Surgical decortication is indicated in advanced stages of empyema because of the high risk of mortality with non-surgical treatment[19].Early Video-assisted thoracoscopic surgery may lead to better outcomes[36]and should be the first-line approach for all patients with acute stage II empyema[5].Clinical stability is required to allow single-lung ventilation and to minimize worse postoperative outcomes[24].
Open-window thoracostomy and thoracoplasty are rarely indicated for the treatment of empyema.Konagayaet al.used minimally invasive open window thoracostomy with vacuum closure therapy to control refractory persistent air leaks in patients with COVID-19-related persistent air leaks and empyema complicated by pleurocutaneous fistula[43].Management of air leak with empyema and COVID-19 is challenging.Surgery is necessary in case of fistulas, whether or not associated with infection of the pleural cavity.The indication for surgical approach at the time of greater clinical stability facilitated the functional recovery of patients[24].Endotracheal valves are used to seal the broncho-pleural fistula or alveolo-pleural fistula when surgery is contraindicated[58].Successful endobronchial closure of a bronchial fistula in a patient with COVID-19 and empyema has been reported.Air leakage secondary to COVID-19 pneumonia with a limited number of air cysts may be a good indicator of endobronchial obstruction[22].
4.5.Outcomes
The mortality rate of 23.3% in the reviewed case reports of empyema with COVID-19 is consistent with the reported mortality rate of 23.8% (5/21) in a recently published retrospective study by Chanet al[50].Pleural infections associated with pneumonia have a poor outcome, with a mortality rate of approximately 20%[10].Comorbidities and patient factors may increase the risk of parapneumonic effusion/empyema and mortality.The causes of death in this review are not attributed only to COVID-19 infection,but also to atypical/unusual pathogens (Candida or mucormycosis),persistent air leak, and severe necrotic empyema that can aggregate severe COVID-19 disease[14,21,29,31,33,36,39,42,47,48].
Reported complications of COVID-19-related empyema included bronchopleural fistula, bronchocutaneous fistula, tracheoesophageal fistula, aggravated hydropneumothorax, and traction bronchiectasis.In general, the main causes of complications in patients with empyema are predisposing medical factors, delayed diagnosis, and irreversible anatomical damage[59].
This review is limited by: (1) the small sample size of the published cases that may limit the use of meta-analysis and meta-regression to draw further conclusions; (2) the included cases came from a variety of institutions with different diagnostic, therapeutic, and surgical capabilities; (3) the review is based on case reports/case series which have the risk of publication, selection, and overinterpretation bias.Case reports/series are often considered a weak source of evidence and tend to yield rather positive results.However, the final included cases contained valuable data regarding the diagnosis and management of COVID-19-associated empyema; (4) Although we have identified high-quality case reports through a comprehensive database search using a systematic strategy including high-quality case reports published in conferences, we cannot prove that we did not miss other reports.
In conclusion, empyema is a rare but serious complication of COVID-19.It can occur early or late in association with other microbial infections, especially in immunocompromised states,immunosuppressive therapy, or persistent air leaks.The predisposing factors, clinical manifestations, and causative organisms are diverse.Treatment could be done only by chest tube drainage and antimicrobial coverage.In the majority of cases, open or Videoassisted thoracoscopic surgery debridement/decortication and other major surgical procedures were performed.Empyema increases the risk of death, especially in patients with atypical pathogens.We recommend further large-scale studies and an updated review.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Funding
The authors received no extramural funding for the study.
Authors’ contributions
All authors have contributed to concept and design of review,literature search, acquisition of data, analysis and interpretation of data, drafting the article, revising the manuscript, and final approval of the version to be published.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Clinical characteristics and outcomes of nosocomial COVID-19 in Turkey: A retrospective multicenter study
- Diversity and species composition of microbiota associated with dengue mosquito breeding habitats: A cross-sectional study from selected areas in Udapalatha MOH division, Sri Lanka
- Molecular evidence and phylogenetic delineation of spotted fever group Rickettsia species in Amblyomma ticks from cattle in Gauteng and Limpopo Provinces, South Africa
- Cutaneous anthrax associated with facial palsy: A case report
- Healthcare-associated Staphylococcus aureus infections in children in Turkey: A sixyear retrospective, single-center study