From precise diagnosis to effective treatment: a case report of atypical Cogan’s syndrome
2023-02-11ChuYuanLouLuLuXueXinLi
Chu-Yuan Lou, Lu Lu, Xue-Xin Li
1Shannxi Eye Hospital, Xi’an People’s Hospital (Xi’an Fourth Hospital), Affiliated People’s Hospital of Northwest University,Xi’an 710004, Shaanxi Province, China
2Department of Ophthalmology, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710004, Shaanxi Province,China
3Department of Ophthalmology, the Fourth Affiliated Hospital of China Medical University, Shenyang 110005, Liaoning Province, China
4Department of Medical Biochemistry and Biophysics (MBB),Karolinska Institutet, Biomedicum, Solnavägen 9, Stockholm SE‐17177, Sweden
Dear Editor,
We present the reported case of a 37‐year‐old male atypical Cogan’s syndrome (CS) patient who was precisely diagnosed and clinically cured under our systematic therapeutic regime. CS is a rare autoimmune disorder involving the eye, characterised by interstitial keratitis (IK)and the auditory‐vestibulo system with vestibular dysfunction.It was first described and named by Cogan[1], an American ophthalmologist in 1945 and confirmed as an autoimmune disease in 1980s[2]. CS consists of typical and atypical subtypes. Typical CS features that the ocular manifestations are limited to the anterior segment (mainly non‐syphilitic IK), with a distinct auditory vestibular impairment usually occurs within 2y. Atypical CS is more complex, and ocular manifestations are diverse, including but not limited to keratitis, scleritis, uveitis, retinitis, papilledema, cataract,and glaucoma. In addition, vestibular auditory symptoms can be two years later[3‐4]. Atypical CS is rarer, and diagnosis is more challenging, in addition, the complexity of atypical CS has caused a higher rate of diagnostic errors and leads to undesirable consequences. The current treatments of CS are consisting of high‐dose glucocorticoid shock therapy and other immunosuppressive agents such as methotrexate and cyclophosphamide. They play important roles in the alleviation and prognosis of the disease collectively. We have obtained the written informed consent from the patient, and this case study is in accordance with the tenets of the Declaration of Helsinki.The patient presented with the eyesight of both eyes gradually decreased with red eyes and photophobia was treated in the Department of Ophthalmology of the Second Affiliated Hospital of Xi’an Jiaotong University on September 30, 2021.The patient was diagnosed with “viral keratitis” in another hospital, but there was no improvement after local antibiotic and antiviral therapy. One month earlier, the patient underwent an “auricle pseudocyst” operation in another hospital.During hospitalization, the patient developed the symptom of hypertension, the highest blood pressure at the time was 170/100 mm Hg. The patient’s blood pressure is relatively stable after taking nifedipine sustained‐release tablets orally.

Figure 1 Before treatment A: Binocular anterior segment. Circular infiltrating foci could be seen in the inferior nasal cornea of the right eye,with ground-glass opacity and slight edema in the stroma. No obvious abnormality was found in the left eye. B: Fundus color photography.The optic disc edema boundary of both eyes was blurred, the veins around the left eye disc were tortuous and dilated, and flame-like bleeding could be seen around. C: Left eye’s OCT. Pigment epithelium detachment could be seen in the macular area. D: Right eye’s anterior segment OCT. High-density reflex areas consistent with the deep matrix lesions and an epithelial bulla could be seen. E: B scan-ultrasound of eyes. The posterior bulbar wall of both eyes was thickened, and the optic disc was locally raised; There was a line gap like an anechoic dark area between the eyeball wall and fat, which was connected with the optic nerve, showing a “T” sign. F: Fundus fluorescein angiography. Fluorescence leakage from both optic discs. OCT: Optical coherence tomography.

Figure 2 After 1wk treatment A: Right anterior segment photography after 1wk of treatment. The ground glass opacity and edema of corneal stroma were significantly improved. B: Color photography of left eye fundus after 1wk of treatment. The flaming hemorrhage around the optic disc of the left eye was absorbed, but the optic disc edema did not improve significantly. C: Left eye OCT after 1wk of treatment. The detachment of pigment epithelium in the macular area has been reset, and no obvious abnormality is found. D: Pure-tone hearing threshold test. The hearing loss of the left ear was mainly medium and high frequency. OCT: Optical coherence tomography.
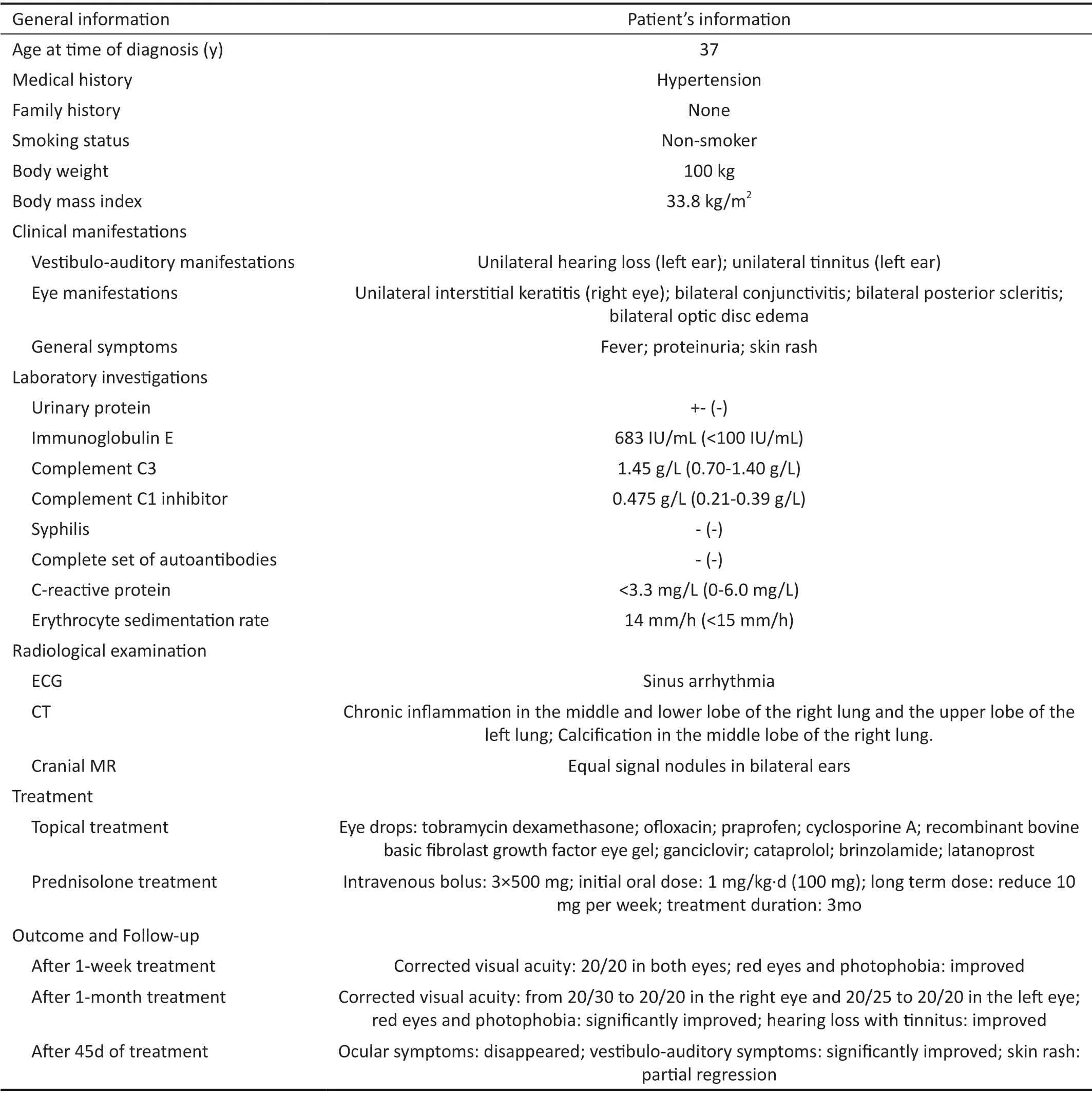
Table 1 Patient’s diagnosis, treatment, and outcome
The patient’s ophthalmologic exam showed: uncorrected visual acuity: 20/30 in the right eye, 20/100 in the left eye;corrected visual acuity: 20/25 in both eyes. Other ophthalmic physical examination and examination results showed in Figure 1. Further systemic examination showed in Table 1.During hospitalization, the patient was given 500 mg of methylprednisolone sodium succinate intravenously.After 3d, it was changed to oral prednisone acetate tablets 1 mg/kg·d (total amount 100 mg), and then 10 mg were reduced every 5d. At the same time, the patient was treated with local antibiotics, hormones, epithelial growth factor eye drops, and local immunosuppressant cyclosporine A eye drops. After 1wk, the corrected visual acuity of both eyes recovered to 20/20, and the symptoms of redness,photophobia, and compression pain were relieved to some extent. The examination results showed in Figure 2. It is worth noting that the patient had rashes on both upper and lower limbs 3d after hospitalization. The intraocular pressure in both eyes increased on day 13 after hospitalization. We considered that the cause of the symptom is hormonal high intraocular pressure, the intraocular pressure was gradually controlled after receiving three kinds of intraocular pressure reducing eye drops (cartelol, brinzolamide, latanoprost). When hospitalized for 20d, the patient said that he had hearing loss in his left ear with tinnitus and had a fever the next day. The blood routine examination showed that the leukocyte was 12.64×109/L,neutrophils 8.21×109/L, monocyte 1.36×109/L. After consulting the specialist in Otolaryngology‐Head and Neck Surgery Department of the Second Affiliated Hospital of Xi’an Jiaotong University, the examination results showed that pure‐tone hearing threshold test: left ear hearing loss (mainly medium and high frequency); Otoendoscopy: bilateral external auditory meatus is unobstructed and tympanic membrane is intact.Inner ear MR: no obvious abnormality was found on the plain scan of the binaural internal auditory canal. Supplementary diagnosis: idiopathic sudden deafness. Therefore, 2000 mg cefathiamidine for injection, 105 mg Ginkgo biloba extract injection, and 30 mg betahistine hydrochloride injection were added for intravenous drip treatment. After 5d of treatment,the fever of the patient was ameliorated and the blood routine has returned to normal, but the left hearing loss and tinnitus symptoms were not relieved. Subsequently, after stopping antibiotics and increasing the dosage of the hormone to 1mg/kg·d for 5d, the patient’s hearing improved slightly. So far, we believe that the correct diagnosis of this case is CS.CS is a rare disease common in young and middle‐aged people. Less than 300 cases have been reported by now thus it is of significant necessity to report the successfully diagnosed and cured cases to the whole research community and share the clinical experiences. The pathological mechanism of the disease remains largely unknown; moreover, lack of the identification of the genetics background has largely impeded the investigation of the disease. Nevertheless, CS has been suggested to be mediated by the hypersensitive responses to infectious agents associated with vasculitis[5]. Furthermore, it has been widely accepted that CS is closely associated with an autoimmune response due to the discovery of autoantibodies to inner ear antigens and corneal structures, as well as the clinical response to immunosuppression[6].
The clinical manifestations of CS are complicated and easily misdiagnosed. In the current case, the patient was misdiagnosed as “viral keratitis” at the first diagnosis.Consequently, there was no significant improvement after 1‐month antiviral treatment. The most significant features of atypical CS are eye symptoms. It should be noted that the prognosis of simple IK is better. The visual impairment caused by scleritis and retinal vasculitis is more serious[6]. Hearing vestibular disorders are often manifested as vertigo, ataxia,tinnitus, hearing loss, nausea, and vomiting. The occurrence of hearing vestibular disorder is usually sudden, and about 22%of patients have recurrent attacks within 1‐13y after the first onset, and eventually resulting in deafness[7]. In addition, some patients will have vascular inflammation which may cause aortic dilation, aortic insufficiency, myocardial infarction, and other diseases. Generally, the patient will have nonspecific systemic symptoms in the first month of onset. In this case,the patient had fever, rash, proteinuria, and other systemic symptoms after admission which is consistent with the clinical manifestations.
Due to the variable onset symptoms of CS and the lack of specific laboratory or radiological examination, the diagnosis of CS is more challenging and diagnostic criteria consensus is lacking . At present, CS is diagnosed mainly based on the clinical diagnosis of auditory vestibular symptoms, ocular inflammation with negative syphilis serological test and vasculitis confirmed by histology[8], as well as the positive response to corticosteroid treatment[9].
At present, the treatment of reported cases mainly depends on the involved organs, systems, and the severity of the disease[10‐12]. Corticosteroids are the cornerstone of CS treatment. For patients with mild eye involvement, local application of glucocorticoids and ciliary muscle paralysis agents (such as atropine) can be selected. Systemic hormone therapy is usually used for patients with posterior segment involvement (such as retinal vasculitis, posterior uveitis,and posterior scleritis): systemic 1‐1.5 mg/kg·d prednisone can generally obtain a good curative effect within 2‐3wk.Subsequently, the Hormone dosage should be gradually reduced, and usually maintained for 2‐6mo. The development of inner ear lesions, severe ocular inflammation, or systemic vasculitis requires immunosuppressive treatment (such as cyclophosphamide, azathioprine, methotrexate, cyclosporine,and tumor necrosis factor‐α blocker). Cochlear implant can be considered for sensorineural deafness with unrecoverable hearing after systemic drug treatment. Severe keratitis can cause corneal ulcer or even corneal perforation. Lamellar keratoplasty or penetrating keratoplasty can be performed according to this situation. Some studies have shown that[13‐14],the occurrence of CS is an autoimmune‐mediated process,and early immunosuppressive treatment is recommended, and some reports show that local application of cyclosporin A has achieved curative effect in the treatment of anterior segment inflammatory diseases. The patient had left ear hearing loss with tinnitus during hospitalization, he received timely otorhinolaryngology head and neck surgical consultation, so the left ear hearing loss was also well relieved. It is worth emphasizing that the early treatment of CS is associated with a higher recovery rate of hearing vestibular impairment[8].But usually, the consequence of hearing impairment with this disease is poor. The timely use of glucocorticoid therapy can prevent hearing loss and the development of systemic manifestations of the disease. In this case, after receiving timely and sufficient systemic glucocorticoid treatment, the hearing impairment and tinnitus were well alleviated.
The diversity of clinical manifestations and the uncertainty of the first symptoms of CS make the diagnosis difficult. CS is a disease requiring multidisciplinary joint diagnosis. At present,due to the limitation of professional cognition of doctors in different specialties and the lack of communication with specialists in other departments, it brings challenges to the early diagnosis of the disease, resulting in a high miss diagnosis rate. Therefore, the correlation between any ocular symptoms and auditory vestibular dysfunction needs to be aware and paid enough attention to. In addition, to provide a better treatment for CS patients, specialists in ophthalmology, otolaryngology,rheumatology, and immunology departments should make a rapid and precise judgment, give systematic intervention in time, and treat patients in time as early as possible.
ACKNOWLEDGEMENTS
Conflicts of Interest: Lou CY, None;Lu L, None;Li XX, None.
杂志排行
International Journal of Ophthalmology的其它文章
- Visual perception alterations in COVID-19: a preliminary study
- COVID-19 pandemic impact on ocular trauma in a tertiary hospital
- Apolipoprotein A1 suppresses the hypoxia-induced angiogenesis of human retinal endothelial cells by targeting PlGF
- Comparison of vegetable oils on the uptake of lutein and zeaxanthin by ARPE-19 cells
- Identifying a novel frameshift pathogenic variant in a Chinese family with neurofibromatosis type 1 and review of literature
- Recurrence risk factors of intravitreal ranibizumab monotherapy in retinopathy of prematurity: a retrospective study at one center
