Clinical value of predictive models based on liver stiffness measurement in predicting liver reserve function of compensated chronic liver disease
2022-11-21RuiMinLaiMiaoMiaoWangXiaoYuLinQiZhengJingChen
Rui-Min Lai,Miao-Miao Wang, Xiao-Yu Lin,Qi Zheng, Jing Chen
Abstract
Key Words: Liver stiffness measurement; Chronic liver disease; Liver reserve function; Indocyanine green clearance test; Predictive model
INTRODUCTION
The high prevalence of chronic liver disease (CLD) in China has become a severe public health problem.Cirrhosis, hepatocellular carcinoma (HCC), hepatic encephalopathy and other decompensated complications are the leading causes of mortality in CLD patients without treatment. Liver reserve function(LRF) is defined as the compensated ability of the liver to maintain normal physiological functions in the presence of injury, which mainly depends on the quality and quantity of hepatocytes in the remnant liver[1,2]. There are no obvious clinical symptoms in CLD patients in the early stage, but their LRF may be impaired. Early evaluation of LRF is of great help in identifying disease progression, timely implementation of interventions and appropriate treatment strategies in CLD patients. Several scoring systems, including the Child-Turcotte-Pugh (CTP), model for end-stage liver disease (MELD), albuminbilirubin (ALBI) and APRI, can be used to evaluate LRF[1,3-5]. Although the CTP score is widely used to assess LRF, it includes subjective criteria, such as ascites and hepatic encephalopathy. The MELD score is initially used as a standard model to assess the prognosis of patients with decompensated cirrhosis,but its creatinine (Cr) value can be significantly affected by age and gender.
The indocyanine green (ICG) clearance test is commonly used for LRF assessment, which is considered the most valuable method for evaluating LRF. ICGR15 had become a standard dynamic preoperative instrument to evaluate the hepatic functional reserve before liver resection and predict post-hepatectomy liver failure[6,7]. However, the ICG clearance test process is tedious and requires a technical operator; thus, most of these tests can only be carried out in major hospitals. In addition, some patients are allergic to ICG, which can lead to failure of the test. Due to impossible implementation of the ICG clearance test in CLD patients, a new method to accurately assess LRF is needed.
Liver stiffness measurement (LSM) is commonly used to evaluate the degree of liver fibrosis, and due to its non-invasiveness, cost-efficiency and safety, it has been widely applied in clinical treatment.Previous studies have shown that LSM can predict the occurrence of liver failure after HCC resection[8-10]. Therefore, LSM has potential value in evaluating hepatic functional reserve.
The purpose of this study was to analyze the association between LSM and ICGR15 in evaluating LRF. We constructed the predictive models based on LSM and examined their clinical application value in evaluating LRF in compensated CLD patients.
MATERIALS AND METHODS
Research population
All patients with CLD (≥ 18 years old) consecutively observed in the inpatient department of the Hepatology Research Institute of the First Affiliated Hospital, Fujian Medical University, China, from March 2016 to June 2019 were retrospectively analyzed as the training cohort. From September 2019 to August 2020, patients with CLD were prospectively evaluated to validate the new models. Information regarding the patients’ demographics, ICG clearance test, laboratory data and Fibro-scan examination was abstracted from the electronic medical record system of the First Affiliated Hospital of Fujian Medical University. Patients with the following conditions were excluded: (1) Decompensated cirrhosis with CTP grade B and C; (2) insufficient data; and (3) complicated with other tumors, or gestation. After exclusion, 492 patients were identified for study inclusion, comprising 389 chronic hepatitis B patients,35 fatty liver disease patients, 21 autoimmune liver disease patients, 8 hepatitis C virus patients and 39 patients with other etiologies. All enrolled patients were divided into the training cohort (360 patients)and validation cohort (132 patients), including 105 HCC patients who met the diagnostic criteria in the guidelines for diagnosis and treatment of primary liver cancer in China (2019 edition)[11].
Clinical and laboratory parameters
The demographic data collected included age and gender. The clinical laboratory information included prothrombin time (PT), international normalized ratio (INR), total bilirubin (TBIL), aspartate aminotransferase, alanine aminotransferase, albumin (ALB), glomerular filtration rate, alkaline phosphatase, gamma-glutamyltransferase, cholinesterase, platelet count, and hemoglobin. The parameters were detected using an Olympus AU2700 automatic biochemical analyzer. The calculation of CTP score included five items, namely ALB, TBIL, PT, hepatic encephalopathy and ascites[12]. The CTP classifications were defined as grade A (5-6 points), grade B (7-9 points), and grade C (10-15 points). The MELD score was calculated by the formula 3.78 × ln[TBIL (mg/dL)] + 11.2 × ln (INR) + 9.57× ln[Cr (mg/dL)] + 6.43 × etiology (0 for cholestasis and alcohol, and 1 for others)[13]. The prothrombin time international normalized ratio to albumin ratio (PTAR) score was calculated by the formula INR/ALB (g/dL)[14]. The ALBI score was calculated by the formula ln[TBIL (mol/L)] × 0.66 + ln[ALB(g/L)]-0.0852[15].
All patients received the ICG clearance test after overnight fasting, a dose of 0.5 mg/kg of ICG was rapidly injected into patientsviaa peripheral vein in the forearm. An optical probe attached to the patient’s nose was used to monitor plasma ICG concentrations, and the value of ICGR15 was calculated by a Pulse Dye Densito-Graph Analyzer (DDG-3300K, Nihon Kohden, Tokyo, Japan)[16]. The LRF was defined as normal if ICGR15 < 10%, mild impairment if ICGR15 ≥ 10%, and severe impairment if ICGR15 ≥ 20%.
The Fibro-Scan 502 Touch (Echosens, Paris, France) was performed by the same trained operator according to the manufacturer’s instructions. LSM was performed on the right lobe of the liver through the intercostal spaces. Ten successful acquisitions were performed for each patient. The success rate (≥60%) was calculated as the number of successful measurements divided by the total number of measurements recorded[17]. LSM was expressed as the median and IQR [in kilopascals (kPa)] of all valid measurements obtained. A LSM was considered reliable if 10 valid acquisitions were obtained.Patients with poorly reliable measurements (IQR/median ratio > 0.30 with a median LSM > 7.1 kPa)were excluded[18]. This retrospective study was approved by the ethics committee of the First Affiliated Hospital of Fujian Medical University, China.
Statistical analysis
Statistical analyses were performed using SPSS 23.0. The normally distributed continuous variables are presented as mean ± SD, which were further evaluated by Student’st-test in the different groups.Whereas, variables showing skewed distributions were evaluated by the Mann-WhitneyUtest, and are presented as median (interquartile range). Categorical variables are described using frequencies and proportions, and the Pearson’s chi-squared test was used to compare categorical variables.
Multivariable analyses were conducted on variables that reachedP< 0.1 at univariate analysis.Multivariate analysis was performed using the logistic regression analysis, and we established regression prediction models to predict the hepatic functional reserve. The continuous variables (cut-off value of LSM was 12.4 and PTAR was 0.280) were transformed into dichotomous variables. In order to avoid collinearity of some clinical indicators, stepwise forward regression was used in multivariate analysis. The optimal cut-off level of the model was determined by a receiver operator characteristic curve analysis. The areas under the curve (AUCs) were measured and compared to evaluate the discrimination ability of different models. The final predictive model was fitted on an internal validation dataset and on the entire prospective population. A two sidedPvalue less than 0.05 was considered significant.
RESULTS
Summary of baseline clinical and demographic data of chronic liver disease patients
Overall, 492 patients were included in the study, including 103 patients with HCC (Table 1). 350(71.14%) of 492 patients were male, the predominant etiology of liver disease was related to HBV (n=389, 79.07%). Patients in the validation cohort were older than those in the training cohort (mean age,54.84 ± 27.70vs48.71 ± 13.34,P< 0.001), and there was a statistically significant difference in ALB and TBIL levels. However, the two cohorts had a similar level of LSM and MELD (P= 0.066,P= 0.241,respectively).
Construction of the LRF predictive model based on LSM
With ICGR15 ≥ 10% and ICGR15 ≥ 20% as the predictive points, the new models of mildly impaired LRF(mLPaM) and severely impaired LRF (sLPaM) were constructed based on LSM. In the training cohort,360 patient variables were included in the multivariate logistic stepwise regression analysis. LSM (OR =4.357, 95%CI: 2.248-8.445), PTAR (OR = 3.544, 95%CI: 1.838-6.835), age (OR = 1.048, 95%CI: 1.024-1.073)and MELD score (OR = 1.340, 95%CI: 1.150-1.562) were independent influencing factors of ICGR15 ≥10% (Table 2). LSM (OR = 3.120, 95%CI: 1.125-8.656), PTAR (OR = 3.524, 95%CI: 1.267-9.801), age (OR =1.059, 95%CI: 1.024-1.096) and MELD score (OR = 1.377, 95%CI: 1.146-1.655) were independent influencing factors of ICGR15 ≥ 20% (Table 3). The predictive models using the above 4 variables were constructed as follows: mLPaM = 1.472 LSM (LSM ≥ 12.4 = 2, LSM < 12.4 = 1) + 1.265 PTAR (PTAR ≥0.280 = 2, PTAR < 0.280 = 1) + 0.047 age (years) + 0.291 MELD-7.600 and sLPaM = 1.138 LSM (LSM ≥12.4 = 2, LSM < 12.4 = 1) + 1.260 PTAR (PTAR ≥ 0.280 = 2, PTAR < 0.280 = 1) + 0.058 age (years) + 0.320 MELD-9.750.
A comparison of the predictive performance of the constructed model and other methods in the training cohort
The AUC values of the mLPaM model (0.855) and sLPaM model (0.872) were greater than that of MELD score, PTAR and ALBI evaluation tools, and their sensitivity and negative predictive values were better than these evaluation methods (Table 4 and Figure 1).
Internal validation of the new predictive model in the validation cohort
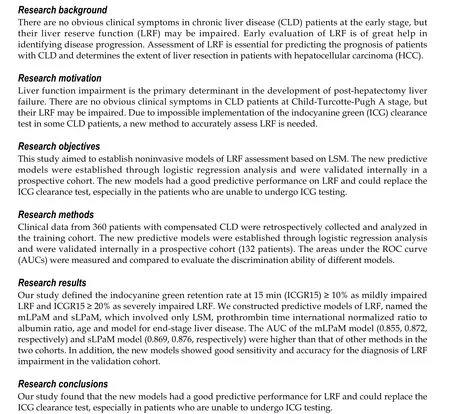
132 CLD patients were prospectively considered for enrollment in the internal validation cohort. The performance of the various methods at predicting LRF is reported in Table 5. The AUC values of the mLPaM model (0.869) and sLPaM model (0.876) were greater than other LRF predictive methods. The mLPaM model showed good sensitivity (89.1%) and optimal accuracy (78.94%) for the diagnosis of mild LRF impairment, and the sLPaM model showed optimal sensitivity (92.9%) for the diagnosis of severe LRF impairment (Table 5 and Figure 2).
DISCUSSION
To date, accurate evaluation of LRF has been a hot topic in national and international research. As classic scoring systems, the CTP score and MELD score have been widely used in clinical practice. The CTP has introduced an element of bias into the scoring system due to the subjective nature of how clinical encephalopathy and ascites variables may be graded[19]. The MELD score is a continuous variable, and each indicator is given a corresponding weight through statistical analysis, which has further accuracy in evaluating LRF. In recent years, the ALBI and PTAR models have been gradually applied in clinical practice, which better evaluated LRF[20,21]. However, the ICG clearance test is currently considered the most valuable test in assessing LRF.
78.80 %的大学生选用“温顺的兔子”“乐观的猴子”来描述自己的性格,其共同点是:性格平和、易相处,属于积极情感隐喻。21.20%的大学生描述自己性格是,强调易怒、难相处的特点,属于消极类情感隐喻。
Although the ICG clearance test is a simple and helpful tool to assess individual LRF, it is an invasive and complex procedure, and the result is influenced by many factors (such as biliary excretion disorder and low proteinemia). In particular, the ICG clearance test is not applicable in pregnant women, patients with a history of iodine allergy or hyperthyroidism[22]. Transient elastography (TE) is a non-invasive and reproducible technique for assessing liver fibrosis, and is even a replacement for liver biopsy[23,24]. The Baveno VII Consensus showed that TE was an accurate tool for the prediction of CSPH[25]. In a previous study, it was found that LSM could predict postoperative liver failure in patients with HCC[26]. Therefore, LSM is considered to have a strong relationship with liver function.
As liver function impairment is the primary determinant of the development of post-hepatectomy liver failure, the vast majority of candidates for liver resection had CTP grade A[27]. According to the CTP classification, the majority of patients with HCC were classified as grade A, but their liver function may vary significantly[15]. A previous study revealed that ICGR15 was more accurate than the CTP score and MELD score in predicting hepatic functional reserve before hepatectomy[3]. The study showed that ICGR15 > 15% was an accurate method of predicting postoperative hepatic decompensation in patients with CTP grade A[28]. In patients with an ICGR15 > 20%, a previous studyrecommended non-anatomical resection rather than anatomical resection for the treatment of a solitary 2–5-cm-diameter HCC without macroscopic vascular invasion[29]. Therefore, it is essential to assess LRF before HCC hepatectomy, thereby assisting clinical decision-making.
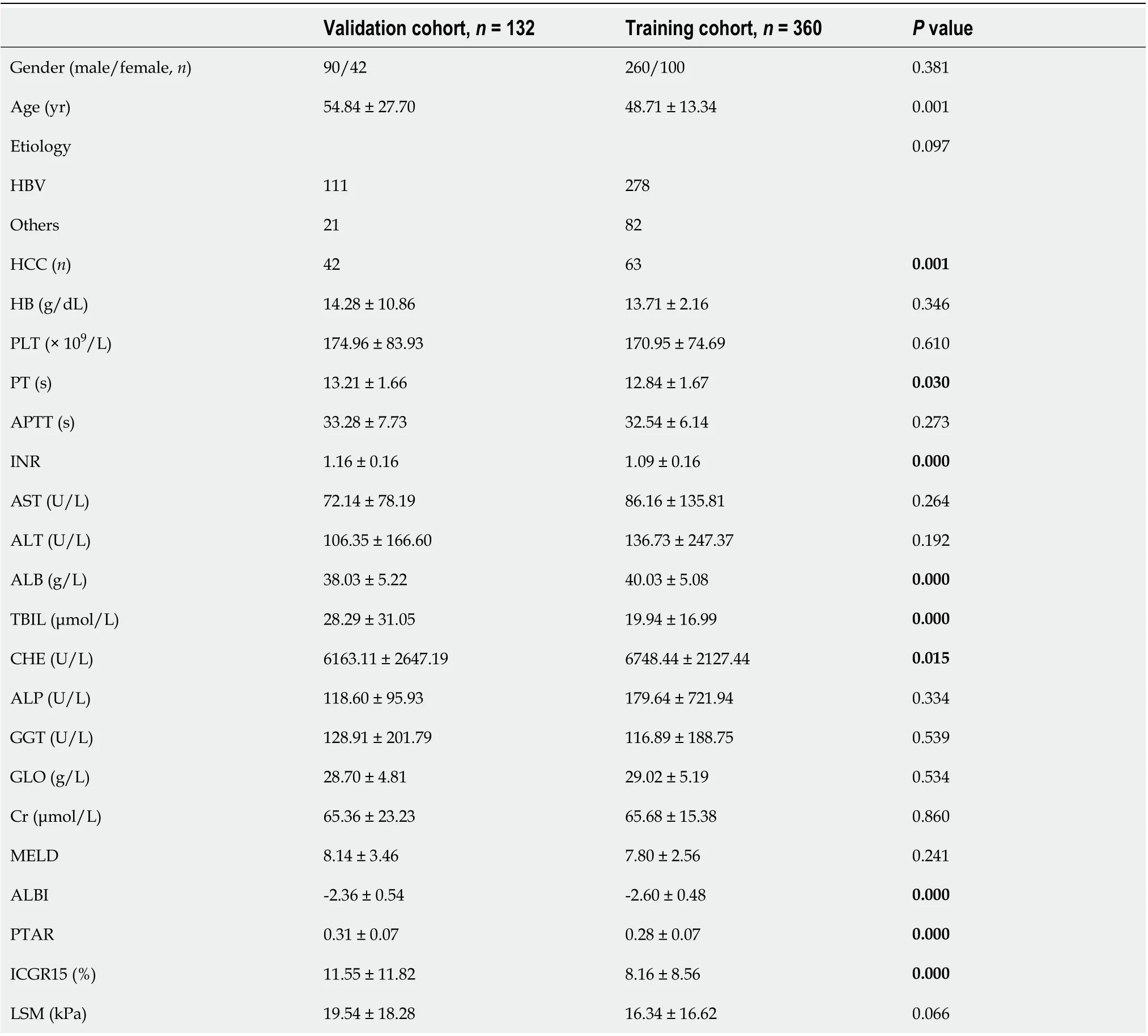
Table 1 Comparison of demographic and clinical characteristics of chronic liver disease patients in the training cohort and validation cohort
Our research constructed new models for clinical prediction of LRF impairment based on LSM, and the models were superior to other existing methods for predicting LRF (Table 4 and Figure 1).Moreover, compared to the other four methods, the models also showed better performance for predicting LRF in the prospective validation cohort (Table 5 and Figure 2). Therefore, based on the analysis of the above research results, these models could be an alternative tool for LRF assessment,especially in evaluating a population almost entirely stratified as CTP grade A.
Limitations of the study
Despite the significant findings in this study, our research also had a few limitations. First, the study was limited by its single-center prospective cohort nature. The patients were recruited from the same medical facility, and not all patients with complete clinical data were obtained from a treatment database. Second, most of the patients in this study were Asians with B viral hepatitis. Therefore, the performance of the model in patients of other ethnicities (e.g., Caucasians, Africans,etc.) still needsfurther investigation. Third, the models were mainly used to evaluate LRF in patients with compensated CLD, and their predictive value in patients with decompensated stage needs further evaluation. Finally,although the formula for the models was relatively complex, a mobile app or web-based calculator could calculate the score easily and rapidly in the current high-tech era. Despite these limitations, this study provided the first accurate models for evaluating LRF based on LSM in China.

Table 2 Multivariate logistic stepwise regression analysis of indocyanine green retention rate at 15 min ≥ 10% in the training cohort
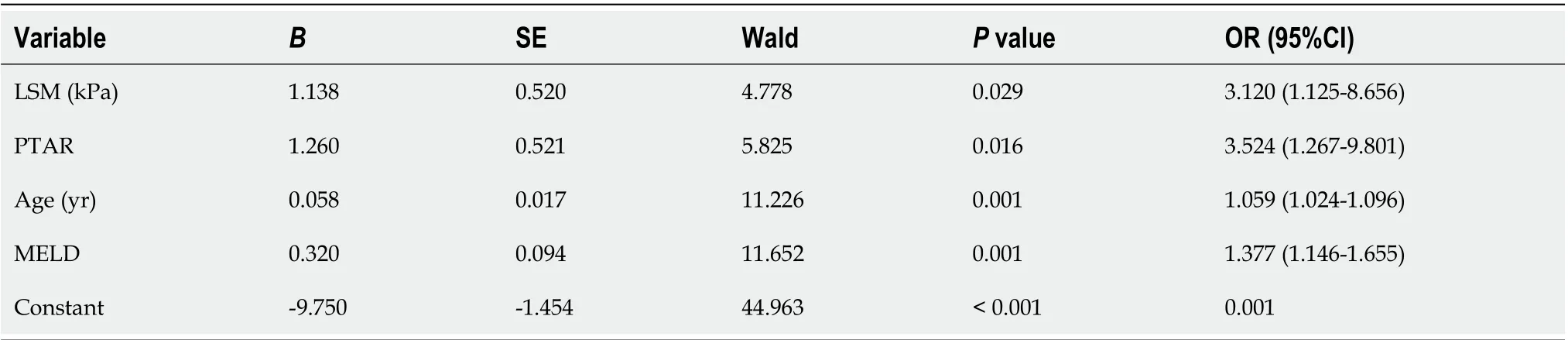
Table 3 Multivariate logistic stepwise regression analysis of indocyanine green retention rate at 15 min ≥ 20% in the training cohort
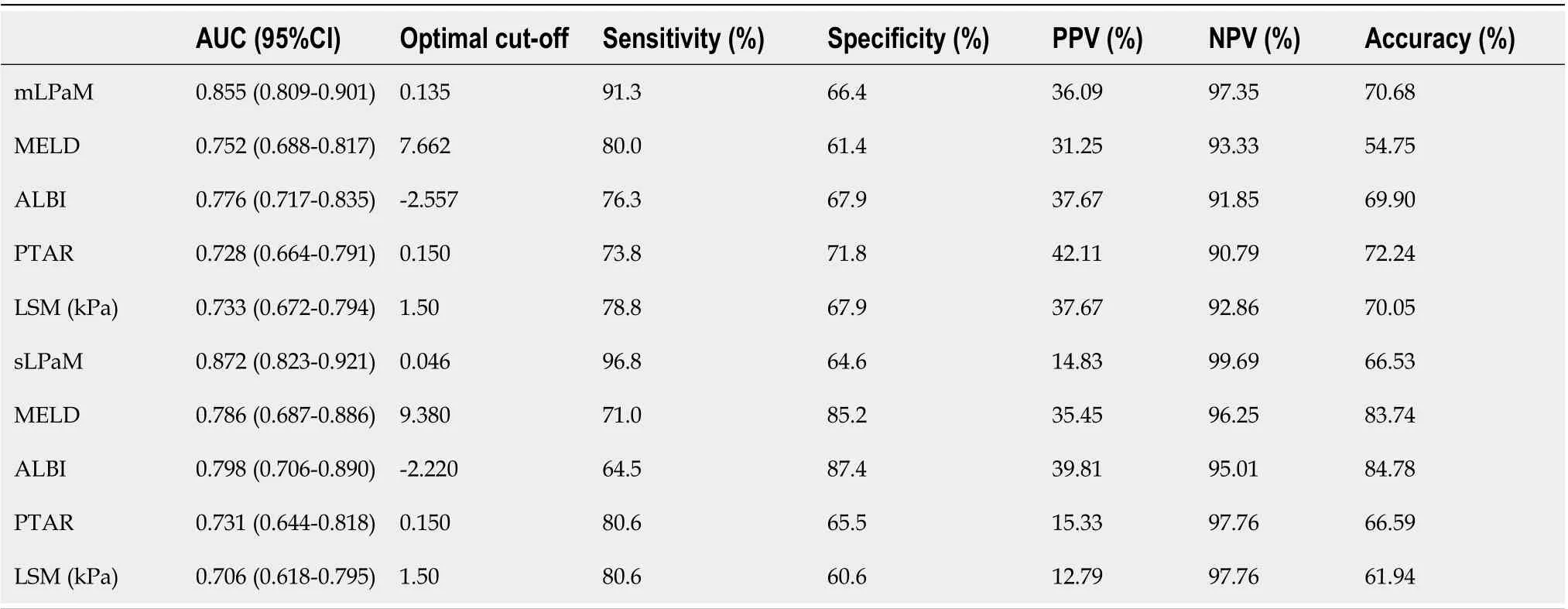
Table 4 Comparison of the predictive performance of the new constructed models (mLPaM and sLPaM) and other models in the assessment of impaired liver reserve function in the training cohort
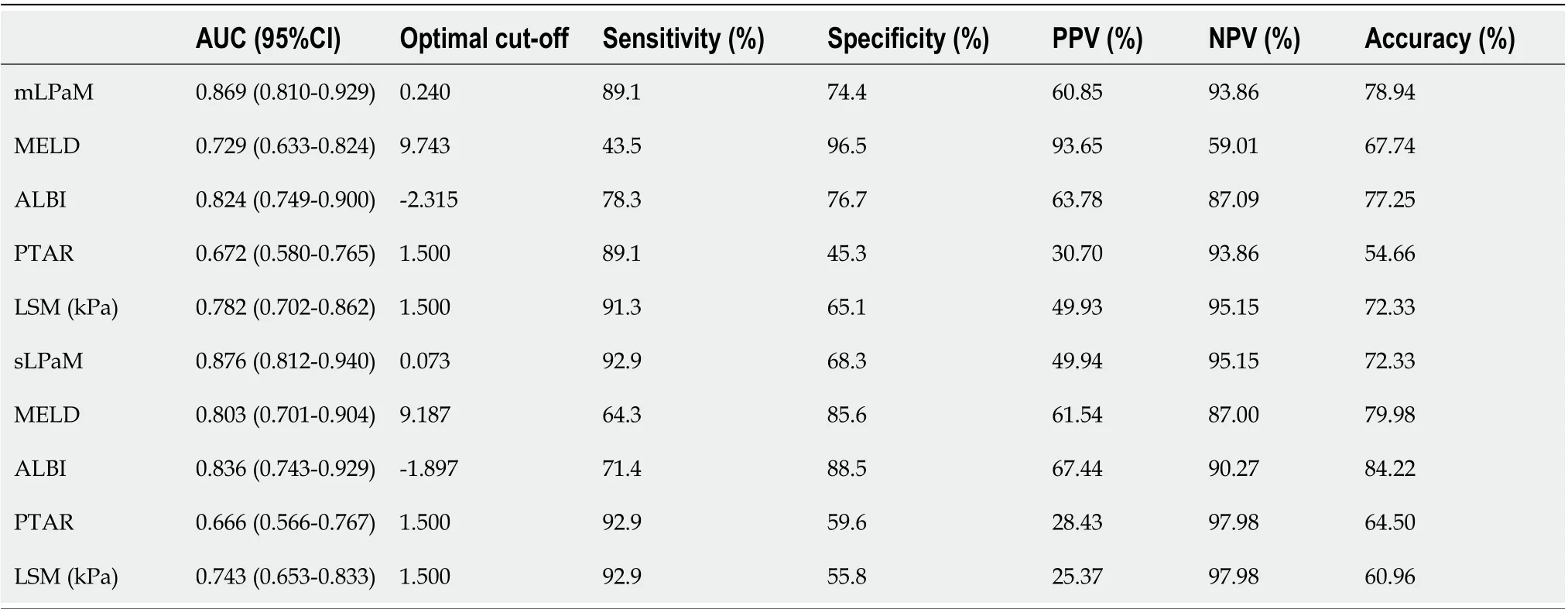
Table 5 Comparison of the predictive performance of the new constructed models (mLPaM and sLPaM) and other models in the assessment of impaired liver reserve function in the prospective validation cohort
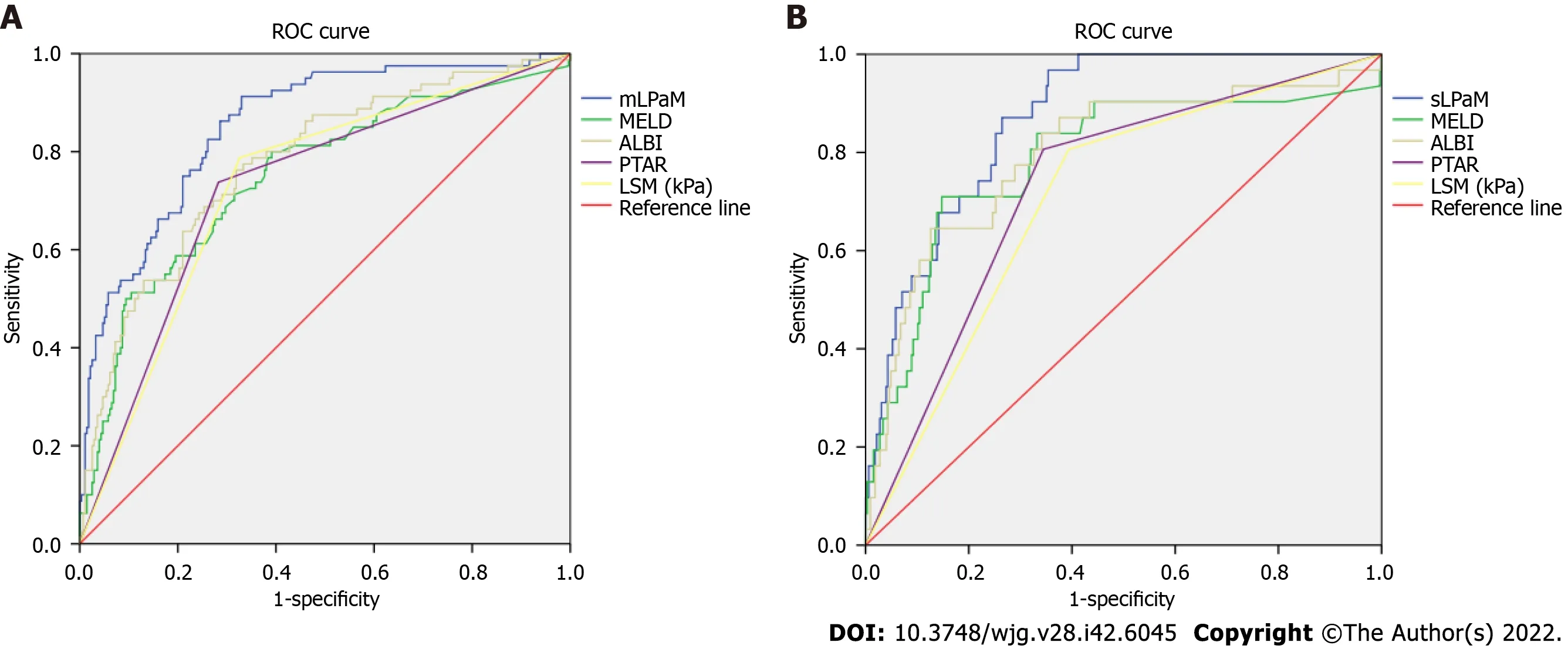
Figure 1 Comparison of different liver reserve function assessment methods by receiver operator characteristic curves in the training cohort. A: mLPaM is indocyanine green retention rate at 15 min (ICGR15) ≥ 10%; B: sLPaM is ICGR15 ≥ 20%. ROC: Receiver operator characteristic; MELD:Model for end-stage liver disease; ALBI: Albumin-bilirubin grade; PTAR: Prothrombin time international normalized ratio to albumin ratio; LSM: Liver stiffness measurement; mLPaM: Mildly impaired liver reserve function model; sLPaM: Severely impaired liver reserve function model.
CONCLUSION
The first predicted models based on LSM could facilitate accurate, reliable and simple-to-use prediction of LRF irrespective of etiology. They are entirely objective based on routine clinical and laboratory parameters. These models would be a useful tool for realizing individualized LRF evaluation to improve the popularity of testing and avoid possible risks during the ICG clearance test, ultimately achieving a clinically feasible and safe LRF test.
Figure 2 Comparison of different liver reserve function assessment methods by area under the curves in the validation cohort. A: mLPaM is indocyanine green retention rate at 15 min (ICGR15) ≥ 10%; B: sLPaM is ICGR15 ≥ 20%. ROC: Receiver operator characteristic; MELD: Model for end-stage liver disease; ALBI: Albumin-bilirubin grade; PTAR: Prothrombin time international normalized ratio to albumin ratio; LSM: Liver stiffness measurement; mLPaM: Mildly impaired liver reserve function model; sLPaM: Severely impaired liver reserve function model.
ARTICLE HIGHLIGHTS
Research perspectives
This was not a multicenter study and most of the CLD patients in this study were Asians. Therefore, a multi-center prospective cohort study could further evaluate the performance of the predictive models,and the models in patients of other ethnicities need further investigation. The predictive value of the models in patients with a decompensated stage need further evaluation.
ACKNOWLEDGEMENTS
We would like to thank the patients who participated in this study.
FOOTNOTES
Author contributions:Lai RM and Zheng Q conceived and designed the study; Wang MM and Lin XY collected clinical data of the patients and contributed to the data analysis; Lai RM and Chen J wrote the manuscript; and all authors approved the final version of the manuscript.
Supported byStartup Fund for Scientific Research of Fujian Medical University, No. 2018QH1052; and Fujian Health Research Talents Training Program, No. 2019-1-42.
Institutional review board statement:This retrospective study was approved by the ethics committee at the First Affiliated Hospital of Fujian Medical University, China.
Informed consent statement:Patients were not required to give informed consent to the study as the analysis used anonymous data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:The original anonymous dataset is available on request from the corresponding author at mykelchen@sina.com.
STROBE statement:The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Rui-Min Lai 0000-0003-2911-0273; Qi Zheng 0000-0001-8006-7069; Jing Chen 0000-0001-5602-1554.
S-Editor:Gong ZM
L-Editor:Webster JR
P-Editor:Gong ZM
杂志排行
World Journal of Gastroenterology的其它文章
- Angiogenesis and immune checkpoint dual blockade: Opportunities and challenges for hepatocellular carcinoma therapy
- Novel management indications for conservative treatment of chylous ascites after gastric cancer surgery
- Computed tomography perfusion in liver and spleen for hepatitis B virus-related portal hypertension: A correlation study with hepatic venous pressure gradient
- Role of radiomics in the diagnosis and treatment of gastrointestinal cancer
- COVID-19 associated liver injury: A general review with special consideration of pregnancy and obstetric outcomes
