Clinical observation on herb-partitioned spreading moxibustion at Baliao points plus climen for diminished ovarian reserve
2020-08-29ChenLi陈丽WanDan万丹FanZhengpeng范正鹏XiaMin夏敏DuanYating段亚亭
Chen Li (陈丽), Wan Dan (万丹), Fan Zheng-peng (范正鹏), Xia Min (夏敏), Duan Ya-ting (段亚亭)
Chongqing Traditional Chinese Medicine Hospital, Chongqing 400021, China
Abstract
Keywords: Moxibustion Therapy; Indirect Moxibustion; Points, Baliao; Gonadal Steroid Hormones; Diminished Ovarian Reserve; Ovarian Reserve; Women
Ovarian reserve refers to the quantity and quality of follicles that remain in the ovary at any given time, which can reflect the fertility of women[1]. Women at the same age may respond differently to ovarian stimulation. Compared with other women at the same age, women at normal menstrual childbearing age with poor ovarian stimulation or reproductive response are defined as having diminished ovarian reserve (DOR). In infertile women, the prevalence of DOR is about 10%[2]. In recent years, with the opening of the national two-child policy, older women have become more longing to have a second child. However, due to factors such as age, work pressure and environment, some women's ovarian reserve function has significantly decreased, leading to a lack of serum sex hormones and declined reproductive ability. If not treated in time, it can further develop into premature ovarian failure, affecting women's quality of life. Therefore, it is urgent to find a safe and effective treatment to improve ovarian reserve function. In this study, we applied herb-partitioned spreading moxibustion at Baliao points plus climen for 30 patients with DOR, and observed the effects on serum sex hormones and ovarian blood perfusion, so as to provide scientific evidences for integrated traditional Chinese and Western medicine treatment.
1 Clinical Materials
1.1 Diagnostic criteria
There is currently no unified diagnostic standard for DOR. Referring to thePractical Gynecologic Endocrinology[3],Obstetrics and Gynecology[4]and related literatures, the diagnostic criteria for Western medicine in this study were established: had a normal menstruation and/or childbearing history, but presenting with sudden oligomenorrhea or infertility, and symptoms of climacteric syndrome appearing in severe cases such as flushing, tidal fever, sweating, dysphoria, irascible and decreased libido; with serum follicle-stimulating hormone (FSH) range of 8.5-40 IU/L, or estradiol (E2) >85 pg/mL, or FSH/luteinizing hormone (LH) ratio >3.6.
Criteria for syndrome differentiation of traditional Chinese medicine (TCM) referred to the criteria of syndrome of kidney deficiency and blood stasis in theGuiding Principles for Clinical Study of New Chinese Medicines[5]. Primary manifestations included oligomenorrhea, impeded discharge of menses, with or without infertility; secondary manifestations included vaginal dryness, dysphoria, soreness and weakness in the waist and knees, oligo-vaginal discharge, pale or muddy complexion, insomnia and sweating; a dark red tongue body with thin coating, and sunken wiry pulse or fine stagnant pulse. Diagnosis could be confirmed when the primary manifestations plus two or more items of the secondary manifestations were met, with reference to the tongue and pulse.
1.2 Inclusion criteria
Those who met the diagnostic criteria of Western medicine and the syndrome differentiation of TCM; aged 20-40 years; no hormonal drugs were taken within 3 months before the study; agreed to participate in this trial and signed informed consent.
1.3 Exclusion criteria
Patients with DOR due to congenital factor, surgery or medications; combined with severe primary diseases of heart, liver, brain or kidney; with mental diseases; accompanied by cognitive dysfunction.
1.4 Elimination and dropout criteria
Did not meet the inclusion criteria but was included by mistake; presenting with severe adverse reactions or unexpected physiological changes; with poor compliance and unable to cooperate with the treatment or examinations; with incomplete clinical data; participated in other clinical trials at the same time.
1.5 Statistical methods
All data were statistically analyzed by the SPSS version 21.0 statistical software. Chi-square test was applied to the comparisons of counting data. Measurement data in normal distribution and having homogeneous variance were expressed as mean ± standard deviation (±s), pairedt-test was used for intra-group comparisons, and groupt-test was used for comparisons between the groups. If data did not meet the normal distribution or homogeneous variance, rank-sum test was applied. The rank-sum test was used for the comparisons of ranked data.P<0.05 was considered to indicate a statistically significant difference.
1.6 General data
A total of 60 DOR patients were enrolled from Chongqing Traditional Chinese Medicine Hospital between March 2018 and March 2019. All the patients were randomly divided into a spreading moxibustion group and a Western medicine group by the random number table method, with 30 cases in each group. The patients in the spreading moxibustion group were aged between 21 and 40 years old, with the shortest duration of 5 months and the longest of 33 months. The patients in the Western medicine group were aged between 24 and 40 years old, with the shortest duration of 3 months and the longest of 34 months. There were no significant differences in the data of average age and average duration of disease between the two groups (bothP>0.05), indicating that the two groups were comparable (Table 1).

Table 1. Comparison of the general data between the two groups
2 Treatment Methods
2.1 Western medicine group
The Western medicine group received climen tablets (Batch No.: J20130006, Bayer Healthcare Co., Ltd., Germany), starting from the 5th day of menstruation. During the first 1-10 d, estradiol valerate tablets were given, 2 mg/time, once a day; during the next 11-21 d, estradiol valerate and cyproterone acetate tablets were given, 3 mg/time, once a day.
2.2 Spreading moxibustion group
On the basis of the same medications in the Western medicine group, herb-partitioned spreading moxibustion at Baliao points was added in the spreading moxibustion group.
Medicine:Shu Di Huang(Radix Rehmanniae Preparata) 150 g,Sang Ji Sheng(Herba Taxilli) 150 g,Du Zhong(Cortex Eucommiae) 100 g,Tu Si Zi(Semen Cuscutae) 100 g,Gou Qi Zi(Fructus Lycii) 100 g,Shan Zhu Yu(Fructus Corni) 100 g,Dang Gui(Radix Angelicae Sinensis) 100 g,Dan Shen(Radix Salviae Miltiorrhizae) 150 g,Ru Xiang(Olibanum) 100 g,Mo Yao(Myrrh) 100 g, andBing Pian(Borneolum Syntheticum) 100 g.
Moxibustion location: The area of Baliao points.
Methods: All the Chinese herbs were bought from Sichuan Neautus Traditional Chinese Medicine Co., Ltd., China. The above ingredients were ground into fine powder, and bottled for later use after sifted through 200 mesh sieves. The patient took a prone position with lumbosacral area exposed thoroughly. The physician first smeared the ginger juice to the Baliao area (about 12 cm×8 cm), then evenly spread the Chinese herbal powder on the part coated with ginger juice (about 2 mm in thickness), (Figure 1). Then the physician laid a layer of aseptic sterile gauze on the Chinese herbal powder, and then spread a layer of ginger powder (about 1 mm in thickness) on the gauze to cover the moxibustion area (Figure 2). Next, the moxa floss was made into a long moxa stick with the length × width × height of about 10 cm×3 cm×3 cm and a triangular cross-section, and laid in the center of ginger powder, slightly shorter than the ginger powder (Figure 3). Then the physician ignited the whole moxa stick from above to apply moxibustion, and waited till it burned out, which was considered as one moxa-cone (Figure 4). After burnt out, the moxa ash was replaced with a new moxa stick to continue moxibustion. The moxibustion took 3 moxa cones in total, which lasted for about 1 h. The moxibustion was performed once every 7 d, and stopped during menstruation.
Both groups were treated for 1 month, which was considered as one treatment course, for 3 courses in total. The clinical efficacy was evaluated at the end of whole treatment courses.
Figure 1. Smearing ginger juice and spreading the herbal powder

Figure 2. Placing the gauze and ginger powder

Figure 3. Spreading the moxa floss

Figure 4. Igniting the moxa-cone and applying moxibustion
3 Observation of Curative Efficacy
3.1 Observation items
Evaluations were conducted before treatment and on the 2nd day of the menstrual cycle after 3 treatment courses, respectively.
3.1.1 TCM symptom score
According to the TCM symptom grading and quantification table in theGuiding Principles for Clinical Study of New Chinese Medicines[5], the scoring criteria of TCM symptom score in this study was established: the primary manifestations were scored 0, 2, 4, and 6 points respectively, representing the degree of none, mild, moderate, and severe. The secondary manifestations were scored 0, 1, 2, and 3 points respectively, representing the degree of none, mild, moderate, and severe. The tongue and pulse were not scored. The sum of all the item scores was the total score. The integral reduction rate was calculated according to the total score. The clinical symptom score reduction rate = (Total TCM symptom score before treatment – Total TCM symptom score after treatment) ÷ Total TCM symptom score before treatment × 100%. was basically normal. The clinical symptom score reduction rate was ≥70%, but <95%.
Improved: The levels of serum FSH, E2and FSH/LH ratio were improved, with intermittent menstruation. The clinical symptom score reduction rate was ≥30%, but <70%.
Invalid: The levels of serum FSH, E2and FSH/LH ratio had no obvious changes, and menstruation did not come after treatment. The clinical symptom score reduction rate was <30%.
3.3 Results
3.3.1 Comparison of clinical efficacy
The total effective rate was 93.3% in the spreading moxibustion group and 80.0% in the Western medicine group. The therapeutic effect of the spreading moxibustion group was superior to the Western medicine group. The difference between the two groups was statistically significant (P<0.05), (Table 2).

Table 2. Comparison of clinical efficacy between the two groups (case)
3.1.2 Serum sex hormone levels
Serum FSH and LH levels were detected by electronic chemiluminescence method. The serum E2level was detected by enzyme-linked immunoassay (ELISA).
3.1.3 Ovarian artery blood flow signal
Peak systolic velocity (PSV) and resistance index (RI) were measured by color Doppler ultrasound.
3.2 Criteria of curative efficacy
According to thePracticalGynecologic Endocrinology[3],Obstetrics and Gynecology[4]andGuiding Principles for Clinical Study of New Chinese Medicines[5], the criteria of curative efficacy in this study were developed.
Cured: The levels of serum FSH, E2and FSH/LH ratio were normal, and menstruation became normal. The clinical symptom score reduction rate was ≥95%.
Markedly effective: The levels of serum FSH, E2and FSH/LH ratio were close to normal, and menstruation
3.3.2 Comparison of the TCM symptom score
There was no significant difference in the TCM symptom score between the two groups before treatment (P>0.05), indicating that the two groups were comparable. After treatment, the TCM symptom scores in both groups decreased, and the intra-group differences were statistically significant (bothP<0.05). The TCM symptom score in the spreading moxibustion group was lower than that in the Western medicine group, and the difference between the groups was statistically significant (P<0.05), (Table 3).
3.3.3 Comparisons of the serum FSH level, FSH/LH ratio and E2level between the two groups
There were no significant differences in the serum FSH level, FSH/LH ratio and E2level between the two groups before treatment (allP>0.05), indicating that the two groups were comparable. After treatment, the serum FSH level and FSH/LH ratio in the spreading moxibustion group were lower than those in the Western medicine group, while the serum E2level was higher than that in the Western medicine group, and the differences between the two groups were statistically significant (allP<0.05), (Table 4).and the intra-group differences were statistically significant (allP<0.05). The ovarian artery PSV in the spreading moxibustion group was higher than that in the Western medicine group, while the RI was lower than that in the Western medicine group, and the differences between the groups were statistically significant (bothP<0.05), (Table 5).
Table 3. Comparison of the TCM symptom score between the two groups before and after treatment (±s, point)
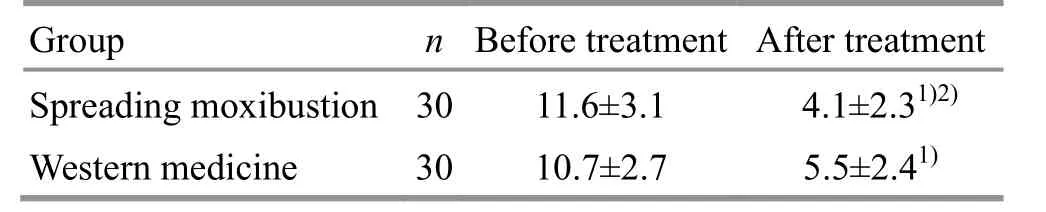
Table 3. Comparison of the TCM symptom score between the two groups before and after treatment (±s, point)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the Western medicine group after treatment, 2) P<0.05
Group n Before treatment After treatment Spreading moxibustion 30 11.6±3.1 4.1±2.31)2) Western medicine 30 10.7±2.7 5.5±2.41)
Table 4. Comparison of the serum FSH level, FSH/LH ratio and E2 level between the two groups before and after treatment (±s)
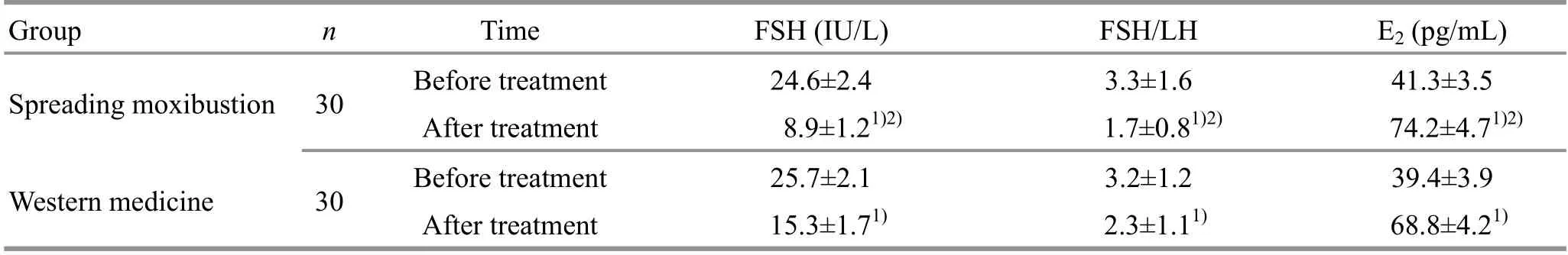
Table 4. Comparison of the serum FSH level, FSH/LH ratio and E2 level between the two groups before and after treatment (±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the Western medicine group after treatment, 2) P<0.05
Group n Time FSH (IU/L) FSH/LH E2 (pg/mL) Spreading moxibustion 30 Before treatment 24.6±2.4 3.3±1.6 41.3±3.5 After treatment 8.9±1.21)2) 1.7±0.81)2) 74.2±4.71)2) Western medicine 30 Before treatment 25.7±2.1 3.2±1.2 39.4±3.9 After treatment 15.3±1.71) 2.3±1.11) 68.8±4.21)
3.3.4 Comparisons of the ovarian artery PSV and RI between the two groups
There were no significant differences in the ovarian artery PSV and RI between the two groups before treatment (bothP>0.05), indicating that the two groups were comparable. After treatment, the ovarian artery PSV in both groups increased, while the RI decreased,
Table 5. Comparisons of the ovarian artery PSV and RI between the two groups before and after treatment (±s)

Table 5. Comparisons of the ovarian artery PSV and RI between the two groups before and after treatment (±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the Western medicine group after treatment, 2) P<0.05
Group n PSV (cm/s) RI Before treatment After treatment Before treatment After treatment Spreading moxibustion 30 10.91±1.36 14.46±1.271)2) 0.649±0.020 0.621±0.0161)2) Western medicine 30 10.52±1.31 12.19±1.041) 0.647±0.017 0.638±0.0191)
4 Discussion
Ovarian reserve refers to the primordial follicles contained in the ovarian cortex, whose function can fundamentally reflect women's fertility and is closely related to the pregnancy outcome. The causes of DOR are very complex and difficult to be found. The pathogenesis of DOR is not yet clear. Modern medical research has found that the main causes of DOR are closely related to genetic factors, immunological factors, enzymatic defects, environmental and psychological factors, and iatrogenic factors[6-7]. DOR first manifests as changes of serum sex hormone levels, mainly manifested as an increase in the serum FSH level and FSH/LH ratio. High level of FSH can keep the function of residual follicles in an inhibited state, which further affects fertility potential in women[8]. At the same time, clinically, ovarian reserve can be evaluated by detecting the levels of cytokines such as anti-Mullerian hormone (AMH) and inhibitor B (INHB), or through the examinations of ovarian volume and ovarian blood flow by Doppler ultrasound[9-10]. As for the treatment of DOR, the common treatment methods of modern medicine include hormone replacement therapy, ovulation induction therapy, immunotherapy, antioxidant therapy, gene therapy and assisted reproductive technology therapy. Among them, hormone replacement therapy has a rapid effect and obvious improvement in symptoms, but the long-term use will cause adverse reactions such as vaginal bleeding and distending pain in the breasts; assisted reproductive technology is relatively mature, but has shortcomings such as high cost and possible failure[11-12].
There is no such name for DOR in TCM. According to the clinical manifestations of DOR, it falls under the category of ‘retarded menstruation’, ‘advanced menstruation’, ‘blood depletion’, ‘early stop of menstruation’, ‘amenorrhea’, or ‘infertility’. TCM believes that the basic pathogenesis of DOR is kidney deficiency and blood stasis. Literature search and analysis also showed that DOR patients were mainly characterized by syndrome of kidney deficiency and blood stasis[13]. Therefore, tonifying kidney and activating blood circulation is the basic treatment principle for DOR[14].
Baliao points belong to the Bladder Meridian, which is exteriorly-interiorly related to the Kidney Meridian. The points are located at the lumbosacral region, consisting of Shangliao (BL 31), Ciliao (BL 32), Zhongliao (BL 33) and Xialiao (BL 34), and close to the female genital organs, with effects of tonifying the kidney and strengthening the lumbar, coordinating the Thoroughfare Vessel and the Conception Vessel, activating qi flow and promoting blood circulation. It is clinically applicable to diseases affecting reproductive system and urinary system, especially the sensitive reflex areas in gynecological diseases such as menopathy and pelvic disease. In this study, herb- partitioned spreading moxibustion at Baliao points was to give topical application of Chinese herbal powder above the points. The Chinese herbal powder was modified by Bushen Huoxue (tonifying the kidney and activating blood circulation) decoction. Among them,Shu Di Huang(Radix Rehmanniae Preparata),Sang Ji Sheng(Herba Taxilli),Du Zhong(Cortex Eucommiae),Tu Si Zi(Semen Cuscutae),Gou Qi Zi(Fructus Lycii) andShan Zhu Yu(Fructus Corni) can tonify the kidney and benefit the essence, strengthen the tendons and bones;Dang Gui(Radix Angelicae Sinensis),Dan Shen(Radix Salviae Miltiorrhizae),Ru Xiang(Olibanum) andMo Yao(Myrrh) can promote blood circulation for dispelling stasis, and remove obstruction in collaterals for relieving pain. The combination of all the Chinese herbs just met the pathogenesis of DOR with syndrome of kidney deficiency and blood stasis. The addition ofBing Pian(Borneolum Syntheticum) ushered the Chinese herbs into the body, prompting the transdermal absorption of the drugs[15-16]. Chinese herbal powder covered with ginger mud and moxa floss was to dispel and warmly unblock by their pungent nature, and to open and penetrate into the interstices, further promoting the Chinese herbs to reach the disease location directly. Study had pointed out that herb-partitioned spreading moxibustion could generate special heat signals including infrared rays during moxibustion, which improved the permeability of the body to drugs[17]. The ginger mud and moxa floss could warm the kidney and activate yang, and unblock the meridians and collaterals. The combination of the above all could tonify the kidney and dispel the stasis, which exactly met the pathogenesis of DOR with syndrome of kidney deficiency and blood stasis.
In this study, after 3 treatment courses, the TCM symptom scores in DOR patients in both groups decreased compared with those before treatment, indicating that both interventions could improve the clinical symptoms in DOR patients, which might be related to the regulation effect of climen on serum sex hormone levels that improved various clinical symptoms caused by hormonoprivia. After treatment, the comparison between the groups showed that the TCM symptom score in the spreading moxibustion group was lower than that in the Western medicine group, and the total effective rate in the spreading moxibustion group was higher than that in the Western medicine group, indicating that the clinical efficacy of herb-partitioned spreading moxibustion at Baliao points plus climen for DOR was significant, and superior to the treatment of climen alone. The reason might be that herb-partitioned spreading moxibustion at Baliao points had a synergistic therapeutic effect with climen in many aspects and multiple links through the stimulation of points, medications and moxibustion, resulting in a superimposed effect.
In this study, we further analyzed the effects of herb-partitioned spreading moxibustion at Baliao points plus climen on serum hormone levels and ovarian blood flow signal values. Among them, serum FSH, LH and E2levels are early signals of ovarian reserve function, and are important indicators to evaluate female ovarian reserve function[18]. The FSH, LH and E2levels in DOR patients are higher than those in women with normal ovarian reserve function, indicating that the changes of serum hormone levels are closely related to the decline of ovarian function[19]. PSV and RI are commonly used hemodynamic parameters in color Doppler ultrasound, which can visually reflect the blood flow distribution in ovary and uterus. Through quantitative analysis, they can reflect the functional status of ovarian and uterine blood flow[20]. A study had pointed out that the use of ultrasound combined with female basic hormone detection to evaluate ovarian reserve function had high sensitivity and specificity, which was conducive to guide female pregnancy, and can provide scientific basis for early diagnosis and reasonable treatment protocol for infertility patients[21].
We found that the serum FSH level, FSH/LH ratio and RI in the spreading moxibustion group all decreased after 3 courses of treatment, while the serum E2level and PSV increased, and were significantly different from those in the Western medicine group, indicating that herb-partitioned spreading moxibustion at Baliao points plus climen could improve the ovarian reserve function by increasing ovarian blood perfusion and regulating the serum hormone levels in DOR patients, thus achieving the purpose of treating DOR.
To sum up, the treatment of herb-partitioned spreading moxibustion at Baliao points plus climen for DOR can play a synergistic effect with points, drugs and moxibustion, thereby improving the clinical efficacy and providing a scientific basis for integration treatment of traditional and Western medicine for DOR. Later study should further increase the sample size, and follow up the laboratory indicators and pregnancy rate to further verify the effectiveness and scientificity of this intervention.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgments
This work was supported by Special Project of Performance Motivation and Guidance for Scientific Research Institutions in Chongqing (重庆市科研机构绩效激励引导专项项目, No. cstc2018jxjll30059).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 22 November 2019/Accepted: 26 December 2019
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Effect of electroacupuncture at Lower He-Sea points including Yanglingquan (GB 34) on nuclear factor-κB and interleukin-1β in guinea pigs with acute cholecystitis
- Study on the differences between moxibustion at different points in the effects on the anti-fatigue ability of rats undergoing one-time exhaustive swimming
- Therapeutic efficacy of moxibustion plus medicine in the treatment of infertility due to polycystic ovary syndrome and its effect on serum immune inflammatory factors
- Clinical study on auricular point sticking plus Western medicine for moderate gastric cancer pain
- Clinical observation on filiform fire-needling plus continuous passive motion therapy for frozen shoulder
- Electronic moxibustion apparatus and traditional moxibustion in treating knee osteoarthritis: a randomized controlled trial
