Ultrasound imaging of abdominal sarcoidosis:State of the art
2019-04-16ClaudioTanaCosimaSchiavoneAndreaTicinesiFabrizioRicciMariaAdeleGiamberardinoFrancescoCipolloneMauroSilingardiTizianaMeschiChristophDietrich
Claudio Tana,Cosima Schiavone,Andrea Ticinesi,Fabrizio Ricci,Maria Adele Giamberardino,Francesco Cipollone,Mauro Silingardi,Tiziana Meschi,Christoph F Dietrich
Abstract
Key words: Sarcoidosis;Sarcoid lesions;Granulomatous disorders;Liver;Spleen;Rare diseases;Ultrasound;Contrast-enhanced ultrasound
INTRODUCTION
Since the first evidence in 1899 of sarcoid lesions provided by the Norwegian dermatologist Caesar Boeck[1,2],it has been recognized that sarcoidosis (SA) is not an exclusive disorder of a single organ,but can affect virtually every tissue,manifesting with clinically silent or symptomatic granulomatous lesions[3,4].In this context the term “great chameleon” was created,indicating a non-specific disease with an undefined etiology that mimicks various disorders in the clinical picture or imaging[5-8].
In the last few years,efforts have been made to define imaging criteria for the diagnosis of specific organ involvement,and the concept has been reinforced that the exclusion of alternative causes is important to achieve the correct diagnosis;a thorough clinical and laboratory assessment is therefore suggested before establishing any imaging approach[9-11].Conventional US can reveal some useful imaging findings,and the recent advent of novel US techniques,such as contrast-enhanced ultrasound(CEUS) and endoscopic ultrasound (EUS) elastography,has provided more information about the abdominal involvement in this uncommon disease.
SARCOIDOSIS,A DISORDER NOT EXCLUSIVE TO THE LUNGS
Among all granulomatous disorders,SA most often affects the lungs and intrathoracic lymph nodes by manifesting with restrictive lung disease[12].However,SA can also involve abdominal organs,such as the liver and spleen,in a non-negligible percentage that varies according to the presence or absence of overt symptoms[13].In particular,the symptomatic involvement of liver and spleen is estimated to be around 10%-25 % and 5%-10% of cases,respectively but asymptomatic cases can be higher[14].A computed tomography (CT) analysis conducted by Warshaueret al[15]in 32 patients with abdominal SA documented a high prevalence of organomegaly and adenopathy(76%).Virtually,there is no organ that is spared from SA[16],and the high potential of ubiquitous body involvement raises the problem of the great diagnostic challenge in patients with suspected abdominal SA,whic may occur in a percentage higher than that documented clinically.The issue becomes even more complex because patients with traditional pulmonary SA do not usually undergo extensive imaging evaluation unless they present significant abnormalities at liver tests[17].
ULTRASOUND ASSESSMENT OF HEPATOSPLENIC SARCOIDOSIS
Although the evidence of hepatosplenic SA at imaging can be limited if there is only a microscopic involvement,ultrasound (US) can be useful to detect some macroscopic findings.Low cost,wide availability and no radiation exposure are some of the main advantages of this method,and routine inclusion of this examination in patients with suspected abdominal SA could be useful to screen the involvement of the liver and spleen[17].However,several other disorders can lead to a liver test dysfunction,such as nonalcoholic liver disease and nonalcoholic steatohepatitis[18],and the two disorders can coexist in such a way as to make the imaging distinction even more complicated.Nevertheless,a first imaging evaluation with US should be included in the routine assessment of patients with suspected abdominal SA,in particular if there is clinical evidence of hepatic dysfunction or liver test abnormalities[17].
Second imaging approaches include contrast-enhanced CT,magnetic resonance imaging (MRI) and18F-FDG PET/CT,which have shown a good diagnostic reliability in the assessment of abdominal SA[19]
Liver disease
US can reveal several non-specific findings in patients with SA of the liver,such as hepatomegaly or bright liver appearance,and can document a significant inhomogeneity of the parenchyma with a coarse nodular pattern,suggesting a patchy granulomatous infiltration of the parenchyma[17,20].Given their nonspecific aspect,however,these findings can be easily misdiagnosed with some features that are observed in other very common disorders,such as fatty liver disease and hepatic cirrhosis[20].
The presence of prominent,various-sized nodules can be documented by showing multiple and rounded hypoechoic lesions.Previous US studies have demonstrated that these nodules usually have no specific size and form but are characteristically hypovascular on Doppler US.The features of these lesions have already been discussed and illustrated[15,17,21].A significant number of disorders (both benign and malignant) enter the differential diagnosis with these lesions,including pseudotumours and tuberculosis[22],and US-guided biopsy can be useful to reveal the presence of non-caseating granulomas,which represent a specific hallmark of the disease and are useful for the definitive diagnosis if the clinical picture or imaging is non- specific or inconclusive[23].
Splenic involvement
The involvement of the spleen is similar to that of the liver,manifesting with nonspecific organ enlargement or hypovascular nodules of various size.In contrast,the lesions can show different degrees of echogenecity (hypo,iso or hyper),possibly according to the different degree of fibrosis of the nodules.However,these lesions can be easily misdiagnosed as nodularities from other disorders;in particular,those that are hypoechoic can be wrongly in-terpreted as lesions from splenic lymphoma,a disorder that is characterized by a hypoechoic appearance of their nodules[24-26].Here again,the problem becomes even more challenging when the two disorders coexist[27].Several studies have,in fact,documented a strong correlation between SA and malignancy (the so-called SA-lymphoma syndrome) and the coexistence of sarcoid and lymphomatous tissue can result in great difficulty of differential diagnosis[28].Sometimes a definite diagnosis is reached only through histological examination,a procedure that would inevitably lead to invasive splenectomy.
LYMPH NODE EVALUATION
Another US finding of abdominal SA is the presence of enlarged lymph nodes,which has been described in up to 76% of the cases as inhomogeneous hypoechoic lesions sized generally 1-2 cm and located in periportal,paracaval,paraaortic and celiac sites.They can be interpreted erroneously as the sign of chronic virus hepatitis C[29],primary biliary cirrhosis[30]and primary sclerosing cholangitis[31];a correct interpretation is therefore mandatory to avoid wrong therapeutic approaches[32].Unlike these disorders,lymph nodes enlargement in SA can reach higher sizes (up to 6 cm) and show tumor-like patterns,with no clear evidence of hilar lymph nodes[17,33].
PANCREATIC INVOLVEMENT FROM SARCOID LESIONS
The pancreas is rarely involved in SA (1%-3% of cases),and focal sarcoid lesions have been reported in less than 50 cases in the literature[34].
Main imaging findings are the presence of hypoechoic and hypovascular focal masses within the parenchyma,sometimes associated with focal or global common bile and pancreatic ducts dilatation[35].Size can vary significantly and large hypoechoic masses can be found exceptionally (Figure 1A).
These findings can mimic the imaging features observed in tuberculosis of the pancreas[36].Further imaging techniques (CEUS and EUS elastography) can be useful to reveal some useful patterns (Figure 1B,see below).
RENAL SARCOIDOSIS
Renal involvement from SA is estimated to be around 25%-30% among all cases,and manifests most commonly with granulomatous interstitial nephritis and disturbances in calcium homeostasis with occurrence of nephrolithiasis and nephrocalcinosis[37].The direct involvement of kidney by granulomatous tissue and the presence of solid masses,however,are extremely rare.Pseudotumours raise significant problems of differential diagnosis with malignant nodules such as renal cell carcinoma and lymphoma,because they can manifest with similar imaging findings.Such nodules can present as single or multiple hypoechoic masses,hypovascular on Doppler US[38].They can grow within renal parenchyma (Figure 2) or be characterized by a focal and exophytic growth[39,40].
For the first time,we found a case of ring-like echogenic pattern determined by a sarcoid lesion of the parenchyma (Figure 3).Also this pattern can be misdiagnosed with that observed in focal malignant lesions.
THE DIAGNOSTIC SUPPORT OF CONTRAST-ENHANCED ULTRASOUND
CEUS has demonstrated a high accuracy to detect and characterize the nature of a large amount of liver and splenic nodules[41,42].Despite this,there are few studies aimed at assessing CEUS patterns in granulomatous infiltration such as from SA,and most evidence derives from large but heterogeneous studies including nodules of different histology[43].The use of CEUS in liver SA can reveal a variable nodular enhancement and progressive hypoenhancement in the arterial and portal-venous late phases,respectively (Figure 4)[17,44].Sometimes the nodules can be hyperenhancing for more than 2 min (Figure 5).
For nodular lesions of the spleen,CEUS can show a progressive hypoenhancement pattern in both the arterial and parenchymal phases,with a higher contrast diffusion toward parenchyma in this phase (Figure 6)[45].
Other enhancement patterns have also been documented (e.g.,rim-like,homogeneous,dotted) and,in particular cases with peripheral or rim-like enhancement in the arterial phase followed by a rapid washout in the parenchymal phase,can mimick the patterns observed for neoplastic lesions,raising great problems of differential diagnosis with solid cancers and hematologic disorders[46,47].
Stanget al[48]have previously reported two cases of splenic SA with diffuse and homogeneous arterial enhancement followed by a progressive hypoenhancement in the parenchymal phase.In this context,the exclusive use of CEUS to confirm the presence of isolated splenic SA can fail,making histopathological examination necessary[49,50].
Lymph nodes enlargement can also be detected by CEUS,by showing a progressive homogeneous enhancement.This pattern can be useful to confirm the benign nature of the lymph node involvement[51].
In contrast,focal lesions of the pancreas show a rapid and transitory enhancement followed by progressive hypoenhancement;a histological examination is thus important to confirm the benign nature of the lesion and to exclude the presence of malignant tissue[35].There is low evidence instead about the CEUS patterns of kidney SA[40].
In this complex scenario,a useful diagnostic algorithm can involve the integration of clinical,laboratory and imaging findings if the abdominal involvement from SA is associated with other clinical manifestations (e.g.,lung disease).The additional diagnostic support of CEUS could be useful to confirm the presence of the lesions.In the case of suspected isolated hepatosplenic or pancreatic SA,however,the additional use of biopsy is strongly advisable to achieve the correct diagnosis,because many common (and also harmful) conditions can be easily misdiagnosed with SA.
There is a great need for studies aimed at evaluating patients with isolated abdominal SA,because,given the pleomorphic nature of SA,it is not difficult to hypothesize other CEUS patterns.

Figure 1 Nodular hypoechoic lesion of the pancreas.
FINDINGS ON ENDOSCOPIC ULTRASOUND ELASTOGRAPHY
Although the evidence derives from single case reports or small case series,the greater diffusion of EUS elastography has provided additional information about the tissue rigidity of sarcoid lesions in abdominal SA.
Liver lesions can show a diffuse blue hard pattern within and around the single masses that correlates well with the granulomatous tissue at biopsy[52].
Lymph node enlargement,instead,shows a mixed,predominantly green pattern at EUS elastography,with a 3-point score (range 1-5 softvshard/solid,respectively)[53].
Similar patterns of rigidity are observed for pancreatic lesions,and both soft and hard tissues are documented on EUS elastography (Figure 1B).These findings suggest the co-existence of mixed tissue components,which are peculiar to disorders such as SA that show both fibrotic tissue and non-caseating granulomas[53].Table 1 shows the main US,CEUS and EUS findings of abdominal SA.
ADVANTAGES AND LIMITS OF US VERSUS OTHER IMAGING METHODS
US is an inexpensive and rapidly available method that can be performed at patient’s bedside.The use of ultrasound contrast agents (UCAs) can improve the detection rate of suspected focal lesions,with a lower risk of hypersensitivity reactions than that associated with X-ray contrast agents,and similar to that encountered with MRI contrast agents[49].The safer profile of UCAs allows repeating the evaluation of the nodules also more than one time for session,giving more opportunities to study the characteristics of the lesions.However,conventional sonographic methods are operator-dependent and have generally lower specificity and sensitivity than other imaging methods such as CT.This is a great limit of the B-mode US evaluation in cases of suspected abdominal SA,because some lesions can be missed at a first imaging evaluation.
CONCLUSION
The involvement of abdominal organs by SA is a possible occurrence that should be taken into consideration in patients with a diagnosis of SA.An increase in US examinations as the screening test in asymptomatic patients could be useful to detect asymptomatic nodules,particularly if there are blood test abnormalities indicating for instance liver dysfunction.The challenge remains in the case of isolated hepatosplenic SA,which is often found by chance and is associated with a significant risk of misdiagnosis with other conditions if an appropriate diagnostic approach is not performed.

Figure 2 Hypoechoic lesion of the kidney that was revealed as focal nodule from sarcoidosis (arrow).
Due to the limited number of cases of abdominal SA that have been investigated with CEUS and elastography,definite conclusions and recommendations are not possible so far.The wider diffusion of these techniques and the increasing evidence about the diagnostic accuracy for nodular lesions have led to a great need also to assess patients with rare conditions such as SA.In the future,we expect more tailored studies in these patients,also to evaluate the diagnostic accuracy of CEUS and elastography in order to give a presumptive characterization of the nature of nodules,which could be useful to guide (or sometimes avoid) invasive approaches,such as histological examination.

Table 1 Main ultrasound and endoscopic ultrasound findings of abdominal sarcoidosis

Figure 3 Ring-like echogenic pattern determined by a sarcoid lesion of the renal parenchyma (markers).
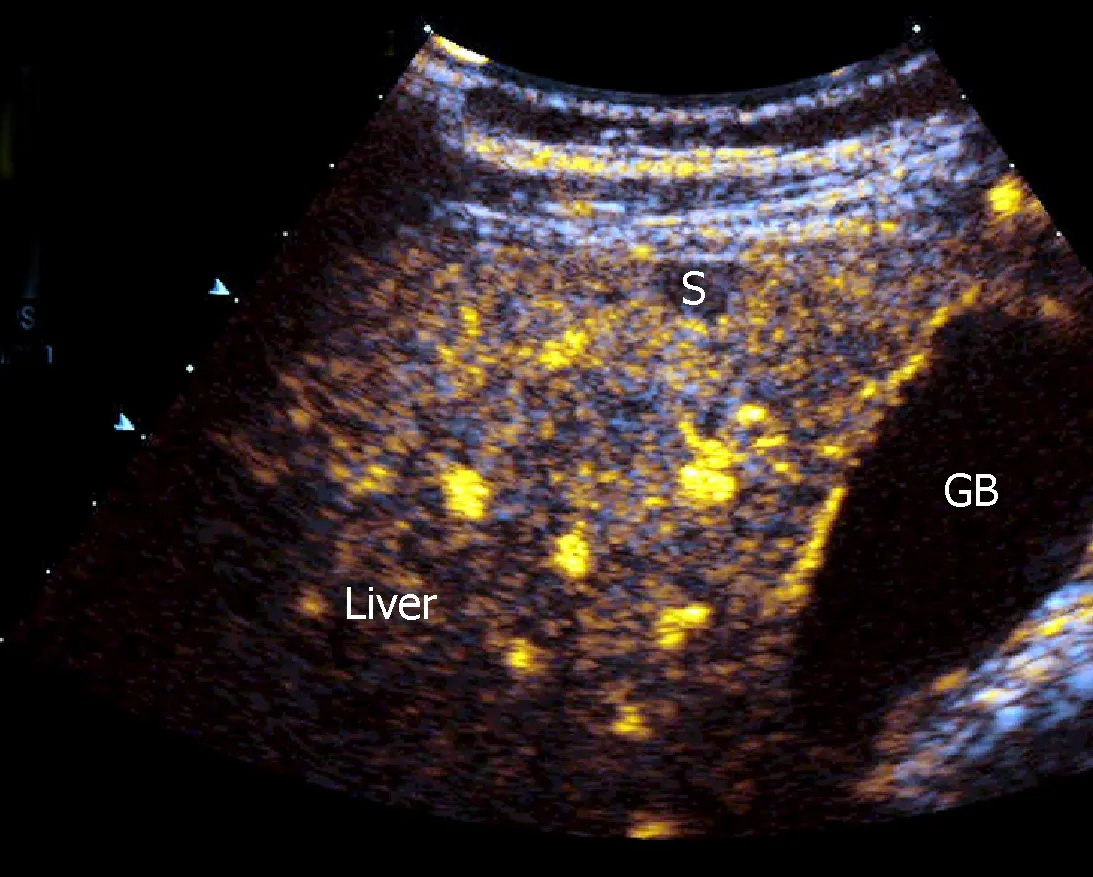
Figure 4 Progressive hypoenhancement in the arterial and portal-venous late phases,respectively,of a nodular sarcoid lesion of the liver.

Figure 5 A rare case of hyperenhancing lesion in arterial,portal-venous and late phase.
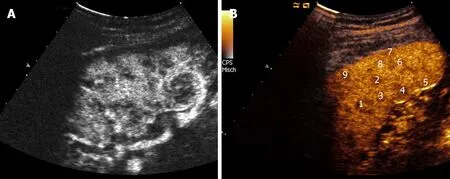
Figure 6 Two different cases of hypoenhancing nodules from sarcoidosis of the spleen.
杂志排行
World Journal of Clinical Cases的其它文章
- Porphyromonas gingivalis and digestive system cancers
- Clinical evaluation of endoscopic resection for treatment of large gastric stromal tumors
- Value of superb micro-vascular imaging in predicting ischemic stroke in patients with carotid atherosclerotic plaques
- Open anterior glenohumeral dislocation with associated supraspinatus avulsion:A case report
- Vein of Galen aneurismal malformations - clinical characteristics,treatment and presentation:Three cases report
- Non-lnvasive management of invasive cervical resorption associated with periodontal pocket:A case report
