A Systematic Review and Meta-Analysis of Herb-Partitioned Moxibustion in the Treatment of Primary Dysmenorrhea
2018-07-26WangXin王昕andLiuYinghua刘颖华
Wang Xin (王昕) and Liu Yinghua (刘颖华)
Department of Obstetrics and Gynecology, Affiliated Hospital of Liaoning University of Chinese Medicine, Shenyang 110032, China
ABSTRACT OBJECTIVE: To systematically evaluate the clinical effects of herb-partitioned moxibustion on patients with primary dysmenorrhea. METHODS: Randomized controlled trials of herb-partitioned moxibustion for primary dysmenorrhea published from the year the database was established to November, 2017 were searched from CNKI,Wanfang Database, VIP database, CBM, PubMed, Embase, and Cochrane Library. Data extraction and quality evaluation were performed in papers meeting inclusion criteria. The outcomes measurements included clinical effect rate, visual analogue score (VAS), plasma PGF2α , adverse events, recurrence rate, and quality of life. The Rev Man 5.3 software was applied for meta-analysis. RESULTS: (1) A total of 16 studies were eligible and included in the meta-analysis involved 1126 patients. (2) A statistically significant increasing in clinical effective rate was found in HMP group compared with control group [OR=3.49, 95%CI (2.25, 5.39), P<0.00001]. (3) There was significant difference between two groups in visual analogue score [MD=–7.48, 95%CI (–9.93, –5.02), P<0.00001], which suggested the patients who received HPM had lower VAS scales than those who received no HPM. (4) There was significantly difference in serum PGF2α between the groups receiving HPM and the control group [MD=–4.61, 95%CI (–9.19, –0.03), P=0.05]. (5) 2 trials reported followup duration, and all included studies did not mention the recurrence of PD during the follow-up stage, and all included studies did not mention the improvement of quality of life of PD during period of management and follow-up stage.CONCLUSIONS: Herb-partitioned moxibustion is beneficial for primary dysmenorrhea. However, the conclusion is not completely accurate with limitations of the current RCTs. The safety of herb-partitioned moxibustion remains to be defined by future studies. Attention should be paid to long-term effects of herb-partitioned moxibustion in clinical research. High-quality RCTs are required to confirm the effectiveness of herb-partitioned moxibustion for primary dysmenorrhea.
KEY WORDS: Primary dysmenorrhea; Moxibustion; Meta-analysis; Guanyuan (CV 4); Shenque (RN 8)
Primary dysmenorrhea (PD) is the most common gynecologic complaint among adolescent and young adult females, and the prevalence ranges from 70.2% to 85.4%,which is characteristic by crampy, colicky spams of pain in the lower abdomen1,2. PD usually starts before the onset of menstruation and relieves after that. The pathogenesis of PD is not yet fully elucidated, and the initiation of PD has been reported to be primarily related with vasopressin,prostaglandin F2a(PGF2α), and oxytocin3. The production and release of PGF2αin endometrium is excessive,inducing uterine hypercontractility and triggering hypertensive pain fiber4-6. Other study suggested that an increase in the ratio of PGF2ato PGE2was a predictor of dysmenorrhea7. Impact of PD on female health and life quality can be very considerable. Women with PD always suffer from severe physiological and psychological symptoms which greatly in fluence the quality of life1,4,8,9.There is no definite cure in modern medicine at present,and the main treatment of PD included nonsteroidal antiin flammatory drugs (NSAIDs), prostaglandin antagonists,oral contraceptives and anti-spasmodic drugs. However,long-term use of these medications is associated with side and adverse effects, such as gastrointestinal discomfort,nephrotoxic and hepatotoxic effects10-13. Therefore, it is necessary to seek complementary and alternative treatment for PD to relieve pain.
Traditional Chinese Medicine (TCM) has been widely used in China to prevent, diagnose and treat diseases over for 2,000 years. Many Chinese medicines have been used for treating PD and are proved to be effective without obvious side effects, such as herbal decoction, acupuncture, acupoint-stimulation,electroacupuncture, moxibustion, etc14-18. Herbspartitioned moxibustion (HPM) is a combination of herbs and moxibustion, and it has the function of acupoint stimulation, moxibustion and herb formulas,which is commonly used in clinics to treat PD19,20. The antagonism of PGF2α,adjustment of endocrine and stimulation of warming signals were shown to be the possible mechanism for HPM21. HPM, as a treatment strategy that is correlated with physical touch and verbal interactions, undoubtedly has a psychological impact on patients. Though moxibustion has advantages, it still needs evidence to confirm some aspects, such as specific effectiveness, safety, low evidence due to insufficient methodological quality. However, no published systematic review focuses on the effects and safety of herb-partitioned moxibustion for PD. Thus, the purpose of this systematic review and meta-analysis study is to determine the effectiveness and safety of herb-partitioned moxibustion for PD.
METHODS
Database and search strategies
We search the following seven electronic databases:the Chinese National Knowledge Infrastructure Database(CNKI), the Wan-fang Datebase, the Chinese Biochemical Literature Database (VIP), the Chinese Biomedical Literature Database (CBM), PubMed, Embase and Cochrane Library. Primary dysmenorrhea, dysmenorrhea,dysmenorrhoea, menstrual pain, painful menstruation,herb-partitioned moxibustion ware the searching key words. The above terms are searched in the databases.Related literatures published from the year the database was established to November 2017 are collected, of which the language is Chinese and English.
Inclusion criteria and exclusion criteria
Inclusion criteria
The included studies were randomized controlled trials (RCTs). Patients enrolled in included studies must be diagnosed as primary dysmenorrhea: PD is defined as painful menses in women with normal pelvic anatomy.Interventions using herb-partitioned moxibustion alone or having same basic treatment as control group were chosen, no specific restriction on moxibustion intensity was imposed. The main outcomes included: ① clinical effect rate; ② pain intensity measured by visual analogue score(VAS); ③ plasma PGF2α; ④ adverse events; ⑤recurrence rate; ⑥ quality of life.
Exclusion criteria
The exclusion criteria was the following: ①patients with a diagnosis of secondary dysmenorrhea, and some other serious organic diseases, ② unpublished or republished literature, ③ non-RCTs, review, comment,case report, experience summaries and animal experiments,④ studies used HPM in combination with other treatments which differed from interventions of control group.
Document selection and data extraction
Two investigators screened articles independently and extracted data from these eligible articles using a standardized data collection form, which included the first author, year of the publication, intervention, sample size, duration for treatment, outcomes assessment. Any disagreement between the two investigators was resolved through discussion until a consensus was reached.
Risk of bias assessment
The assessment of risk of bias was evaluated using Cochrane Collaboration handbook for systematic reviews Version 5.0.2, which was based on the following elements: random sequence generation, allocation concealment, blinding, incomplete outcome data,selective reporting, and other bias.
Statistics analysis
Meta-analysis was performed using the Rev Man 5.3. Relative risks (RR) were calculated for the dichotomous outcome of the effective rate, and mean differences (MD) were calculated for the continuous outcomes with 95% confidence intervals. Chi Square was used to analyze the heterogeneity which is evaluated by I2. If P value was>0.1 and I2was<50%, the studies were considered to be homogeneous, and a fixed-effect model was used. If I2was>50%, the trials were considered to be heterogeneous, and a random-effect model was used.Forest plots and funnel plots were generated via Rev Man 5.3.
RESULTS
Literature Search
After primary search from the 7 databases, 219 relevant articles were screened including 218 Chinese studies and 1 English article. 147 duplicate documents were removed. By reading the titles and abstracts, 38articles were excluded because they did not meet the inclusion or exclusion criteria. Full texts of 34 studies were retrieved, and 18 articles were excluded. In summary, 16 studies were eligible and included in the meta-analysis finally.
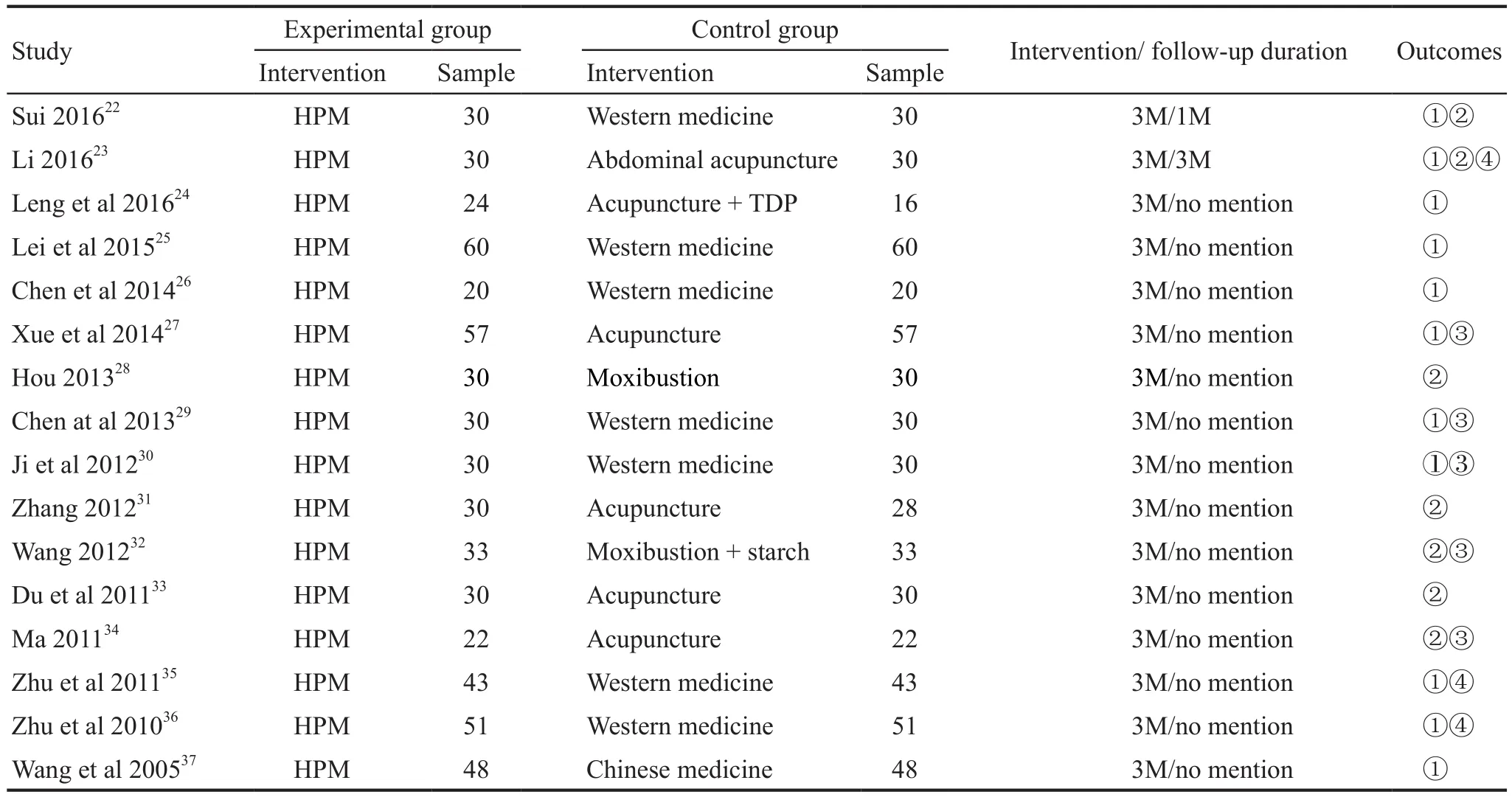
Table 1. Characteristics of the included studies for the treatment of PD
Characteristics of included trials
Sample size
The 16 studies involved 1126 patients. The intervention group included 568 patients and the control group included 558 patients. Participants in one study were of at most 120 or least 40. No study reported the evaluation and calculation method of sample size. All study had reported that the baseline data was compared between intervention group and control group.
Intervention
In the experimental group, HPM alone was used to manage PD. In the control group, studies used western medicine, abdominal acupuncture, acupuncture with TDP, moxibustion, moxibustion with starch and Chinese medicine.
Criteria of efficacy evaluation
9 studies reported standard of efficacy evaluation by referred to Guideline for Clinical Research of Chinese Medicine New Drugs23,25-26,28-30,35-37. One study used criterion of diagnosis and therapeutic effect of TCM Syndrome (1994) to evaluate the effectiveness of HPM24.No criteria of clinical effectiveness were reported in one study14. The 5 remaining studies did not report criteria of efficacy evaluation because of no evaluation of clinical effective rate22,31,33-34.
Acupoints
10 acupoints were used in 16 trials, including Shenque (CV8), Guanyuan (RN4), Sanyinjiao (SP6),Lumbosacral spine acupoint, Qihai (CV6), Chungchi(CV3), Zigong (extra 16), Guilai (S29), Baliao acupoint.The frequency of Shenque (CV8) was highest, and the second was Guanyuan (RN4). The frequency of Shenque(CV8), Guanyuan (RN4) was 14 and 2 respectively.
Period of treatment and follow-up
The treatment period lasted three menstruation cycles in 16 studies. Two studies reported the follow-up condition22,23. One study reported that the follow-up was of three menstruation cycles22, and the follow-up was one menstruation cycles in another study23. The general characteristics of included trials for the treatment of PD were presented in Table1.
Risk of bias assessment
Results of the risk of bias assessment were presented in Figure 1. All the included studies reported the randomization. 5 articles27,31-34mentioned the method of center randomized block, and 7 studies22,23,26,29,30,35,36used the method of random number table. One article24reported the using of inappropriate method of clinic visit date, and other studies only reported the randomization and did not describe the random method. Regarding the allocation concealment, two studies22,23reported the allocation concealment with opaque sealed envelope. The blinding of data collectors, outcome assessment and data analysis was reported in one study22and was unclear in the remaining 15 studies. All studies had the complete data and were free of selective reporting. Other bias was unclear with no mention in all included studies.
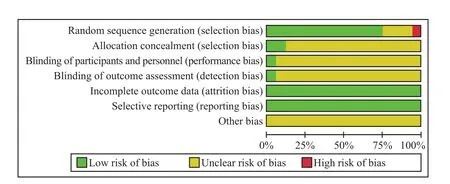
Figure 1. Risk of bias graph of bias assessment
Clinical effective rate
The criteria for the clinical effective were as follows:cure (abdominal pain disappeared during menstruation),significant effective (a significant improvement of abdominal pain during menstruation), effective(improvement of abdominal pain) and ineffective (no improvement after treatment). Clinical effective rate was the accumulation of cure rate, significant effective and effective rate. The effective rate of treatment was pooled for 11 studies, including a total of 844 patients (424 patients in HPM group, 420 patients in control group). As shown in Figure 2, high homogeneity was observed in the meta-analysis (P=0.30, I2=15%), and a fixed-effect model was applied. The meta-analysis revealed a statistically significant increase in clinical effective rate in HMP group compared with control group [OR=3.49, 95%CI(2.25, 5.39), P<0.00001].
Publication bias
A funnel plot was conducted to evaluate publication bias. The funnel plot for the outcome of effective rate shown in Figure 3 was incompletely symmetrical, indicating potential publication bias in the included studies.
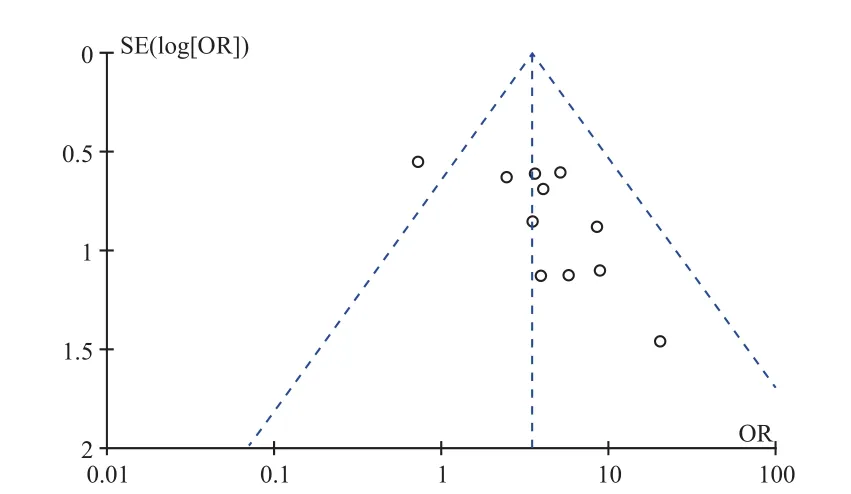
Figure 3. Funnel plot of publication bias
Visual analogue score
Seven studies were considered suitable for the VAS evaluation, yielding 204 patients in HPM group and 202 in the control group. The heterogeneity was low (P=0.21,I2=29%) and a fixed-effect model was applied. The metaanalysis showed that there was significant difference between two groups [MD=–7.48, 95%CI (–9.93, –5.02), P<0.00001](Figure 4), which suggested the patients who used HPM had lower VAS scales than those who used non HPM.
Serum PGF2α
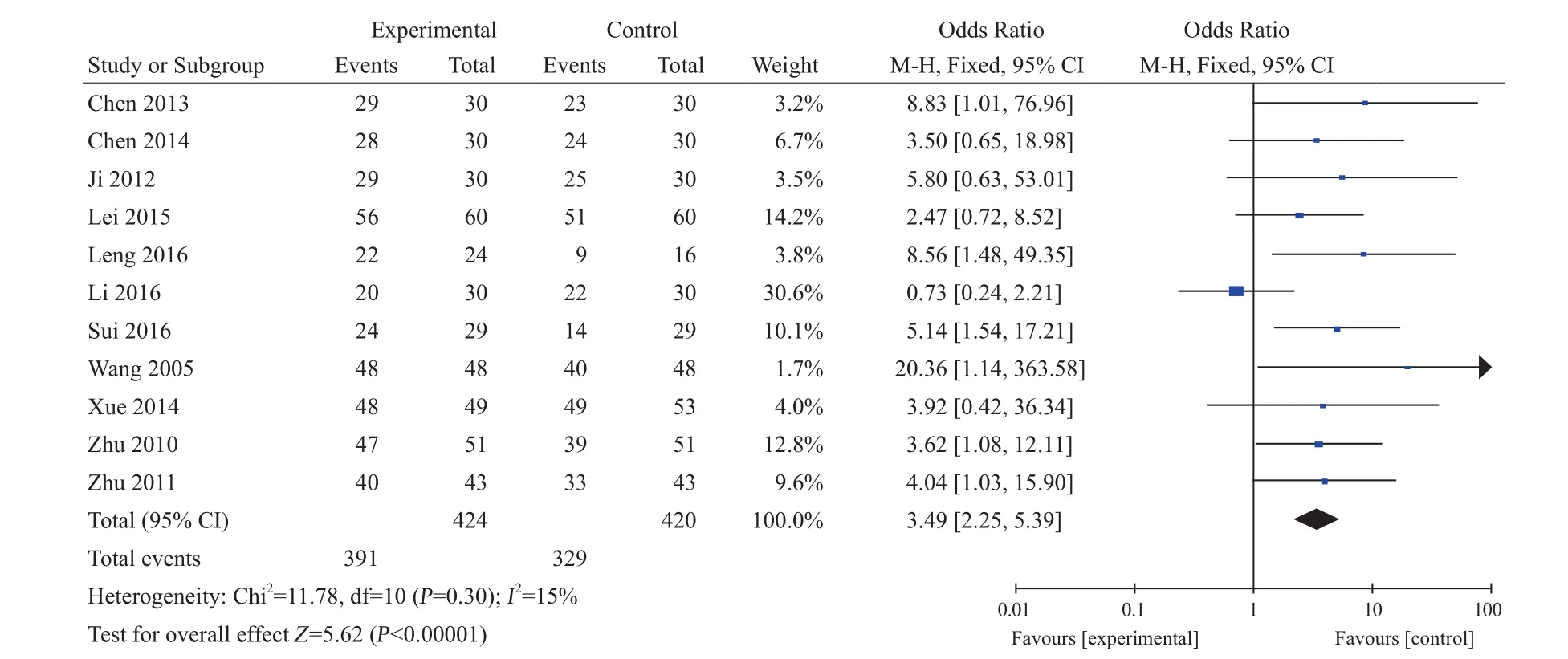
Figure 2. Meta-analysis of the clinical effective rate
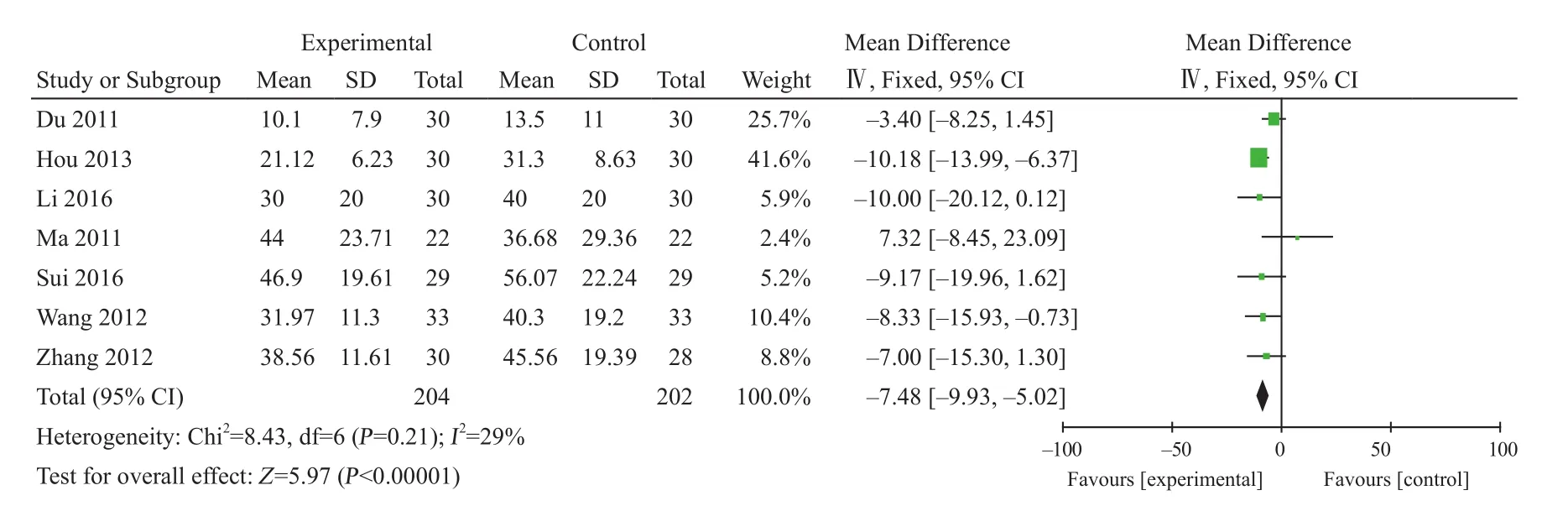
Figure 4. Meta-analysis of the VAS
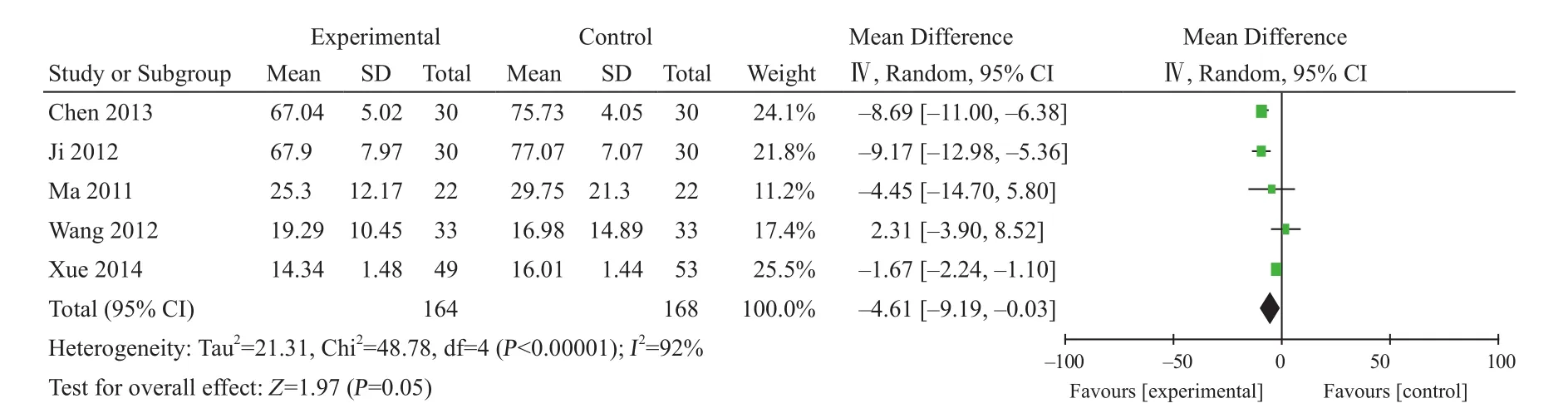
Figure 5. Meta-analysis of serum PGF2α
332 patients from five trials reported serum PGF2α.The meta-analysis revealed high heterogeneity (P<0.1, I2=92%),and a random-effect model was used. The meta-analysis indicated that there was significant difference in serum PGF2αbetween the groups receiving HPM and the control group[MD=–4.61, 95%CI (–9.19, –0.03), P=0.05] (Figure 5).
Recurrence rate and quality of life
Patients who discontinued medication experienced a higher incidence of recurrence because protective effect of these medications vanished rapidly after discontinuation.Studies should pay attention to the recurrence, and recurrence rate should be one of clinical outcomes. In the paper, 2 trials22-23reported follow-up duration, and all included studies did not mention the recurrence of PD during the follow-up stage. In addition, no trials reported the improvement of quality of life.
Adverse events
Three studies reported the side effects between the HPM and control groups. One study23reported no obvious adverse effects or discomfort after treatments.Two studies35-36reported adverse events in control group,including nausea, vomiting, abdominal pain, dizziness and headache.
DISCUSSION
Traditional Chinese medicines, such as herbpartitioned moxibustion, had been widely utilized by physicians to treat primary dysmenorrhea with unique advantages. Moxibustion relieved pain through the frontal cortex-basal ganglia-cerebral cortex and parietal lobebasal ganglia-margin leaf-frontal lobe two circuits. It possibly controlled the pain from sensation, emotion and cognition38. Previous study reported that moxibustion changed function of a series of pain-related brain regions39. In addition, the regulation of normal PGF2α,inhibiting the spastic contraction of uterine smooth muscle were the mechanism of moxibustion for PD40.Studies supported the beneficial effect of herbal formulas and acupoint stimulation in the treatment of primary dysmenorrhea prescribed by physicians according to a patient's symptoms and acupoint stimulation14,41,42,17.HPM had both the function of acupoint stimulation,moxibustion and herb formulas. Therefore it was more effective than acupoint stimulation, moxibustion and herb formulas. Our result of the study showed that compared with non-HPM treatment, the HPM was more effective to increase the clinical effective rate, reduce the VAS,,which suggested HPM was better than western medicine,acupuncture, pure moxibustion and Chinese medicine.
This systematic review and meta-analysis identified 16 studies involving 1126 participants examining the effects of HPM therapy for PD. In our meta-analysis,the clinical effective rate of HPM was evaluated through an analysis of eleven pooled RCTs. Results of the metaanalysis suggested that herb-partitioned moxibustion was superior to western medicine, acupuncture, pure moxibustion and Chinese medicine for the management of primary dysmenorrhea in terms of clinical effective rate(OR 3.49, 95% CI 2.25 to 5.39). However, one studies showed that effective rate of herb-partitioned moxibustion was less than that of abdominal acupuncture. This may be related to the different acupoints in two groups. In terms of visual analogue score, seven studies reported variation using the VAS (MD –7.48, 95% CI –9.93 to–5.02), suggesting that HPM had a significant effect on menstrual pain compared with controls. However, the results were mainly based on immediate effectiveness,and only two studies reported long-term effectiveness with VAS scale for primary dysmenorrhea after three menstrual cycles with treatment. Moreover, 332 patients from five trials reported the serum PGF2αand there was significant difference in serum PGF2αbetween the groups receiving HPM and the control group (MD –4.61, 95% CI–9.19, to –0.03). The analgesic effect of herb-partitioned moxibustion may be associated with the regulation of the PGF2α, which had been proved by experimental evidence43,44.
Previous study demonstrated PD impaired the patients' quality of life45. Reducing this problem was an important reproductive health special duty for gynecologists. Therefore, the quality of life should be one of the indicators of evaluation for PD. Plenty of studies just evaluated immediate effect of management of primary dysmenorrhea, long-term effectiveness was not reported. Recurrence rate was evaluated during follow-up stage, which was an indicator of long-term curative effect. Quality of life and recurrence rate should be the indexes of treatment for primary dysmenorrhea.However, in this review, no article mentioned the quality of life and recurrence, which suggested that the effect of herb-partitioned moxibustion.should be evaluated from different aspects.
62.5% studies reported standard of efficacy evaluation. The standard of efficacy evaluation referred to guideline for clinical research of Chinese medicine new drugs or diagnosis and therapeutic effect of TCM Syndrome. No criteria of clinical effectiveness was reported in six studies. Considering the complexity of the primary dysmenorrhea, it was suggested that the evaluation of clinical effective rate should be standardized and unified. 13 studies (81.25%) did not report the adverse events, only 3 studies (18.75%) reported the adverse effects. The safety of herb-partitioned moxibustion was not yet fully confirmed. We speculated to a certain extent that herb-partitioned moxibustion was safe.
From the meta-analysis results we knew that methodological quality of the included articles was relatively low. The results were unclear in risk of bias assessment of most researches. The methodological quality directly affected the effects evaluation of herbpartitioned moxibustion, thus it's not enough to get a strong conclusion. No trials involved in our study reported the evaluation and calculation method of sample size. The researchers should follow the statement of a randomized controlled clinical report to evaluate the sample size for providing the reliable treatment for patients . Random allocation was the best way to reduce the selective bias of patients between groups and the use of blind method was to avoid subjects and researcher to interfere with the results. In our study, 81.25% trials described the specific random method, 12.5% trials reported the allocation concealment and 6.25% research pointed out blinding of researchers and patients. It was concluded that most of studies had not fully recognized the importance of allocation concealment and blinding.
Shenque (CV8) located in the middle of the abdomen, the center of the umbilicus, which is characterized by thin skin, high sensitivity, numerous capillaries, strong permeation and fast absorption, and has been the major acupoint to be used in treating PD according to the meridian theory of Chinese acupuncture.What's more, it was used most frequently in treating PD according to our results. Previous studies had shown that CV8 stimulation could relieve the abdominal pain and improve the menstrual pain-related symptoms35,46.Guanyuan (RN4), located in three cun below the umbilicus, and it was the intersection of Ren channel and Three Yin channels of foot. Afferent fibers of RN4 and uterus converged and overlapped in the spinal cord of L3 and S5, therefore RN4 stimulation affects the uterus47. Studies showed that CV4 stimulation regulated the imbalance of vasomotor substances TXB2/6-KETOPGF2α, improve hemorrheology of dysmenorrhea rats and reduced pain intensity48. SP6 is located medially four-finger wide above the ankle. One study reported electroacupuncture at SP6 provided immediate analgesia effect for PD49. Recent studies had shown that SP6 stimulation relieved the abdominal pain50. In addition,Sanyinjiao and Guanyuan had synergistic effect for PD51. Thus, Shenque (CV8) and Guanyuan (CV4) were recognized as key acupoints for PD, and SP6 collaborates with rn4 to enhance the clinical effect.
This study had some limitations: ① The sample size was small, leading to a low inspection efficiency.② In most of articles, there was inadequate reporting of allocation concealment, blinding, and other bias, which reduced the reliability of the results. ③ 14 included articles did not mention the data in follow-up stage, so that evaluation of the long-term effects of HPM was difficult. ④ Adverse events were limited in the study, thus safety of HPM was insufficient. In the future, attention should be paid to allocation concealment, blinding,follow-up condition and adverse events.
In conclusion, our systematic review and metaanalysis provides an evidence that herb-partitioned moxibustion has a certain effect for PD on clinical effective rate, pain intensity. However, the conclusion is not completely accurate with limitations of the current RCTs. Clinical acupoints in common use include Shenque(CV8) and Guanyuan (CV4), and acupoints should be used based on syndrome differentiation. Adverse event of herb-partitioned moxibustion for PD is insufficient,and the safety of herb-partitioned moxibustion remains to be defined by future studies. Attention should be paid to long-term effects of herb-partitioned moxibustion in clinical research. Moreover, more randomized, doubleblind, large sample size trials of herb-partitioned moxibustion for PD are needed to obtain evidence of effectiveness and safety.
杂志排行
World Journal of Integrated Traditional and Western Medicine的其它文章
- Therapeutic Effects of "Soothing the Liver Method" on Stress-related Non-alcoholic Fatty Liver on Neuroendocrine-metabolic Level
- New Year's Message
- Systematic Review and Meta-Analysis of Randomized Controlled Trials of Xianling Gubao Capsule as Adjuvant Treatment of Osteoporotic Fracture
- Analysis on the Pharmacists Intervention Results of the Problems from 2000 Prescriptions of Chinese Herbal Pieces
- Probing the Definition of Yin and Yang in Our Body
- A Life System Tuning Model
