Comparison of neurological clinical manifestation in patients with hemorrhagic and ischemic stroke
2017-02-10SeyedhosseinOjaghihaghighiSamadShamsVahdatiAkramMikaeilpourAliRamouz
Seyedhossein Ojaghihaghighi, Samad Shams Vahdati, Akram Mikaeilpour, Ali Ramouz
1Emergency Medicine Deparmtent, Tabriz University of Medical Science, Tabriz, Iran
2Road Traff c Injury Research Center, Tabriz University of Medical Science, Tabriz, Iran
3Tabriz University of Medical Science, Tabriz, Iran
4Medicine Faculty and Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
Comparison of neurological clinical manifestation in patients with hemorrhagic and ischemic stroke
Seyedhossein Ojaghihaghighi1, Samad Shams Vahdati2, Akram Mikaeilpour3, Ali Ramouz4
1Emergency Medicine Deparmtent, Tabriz University of Medical Science, Tabriz, Iran
2Road Traff c Injury Research Center, Tabriz University of Medical Science, Tabriz, Iran
3Tabriz University of Medical Science, Tabriz, Iran
4Medicine Faculty and Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
BACKGROUND: Cerebrovascular accident (CVA) is the third leading cause of death and disability in developed countries. Anyone suspected of having a stroke should be taken immediately to a medical facility for diagnosis and treatment. The symptoms that follow a stroke aren't signif cant and depend on the area of the brain that has been affected and the amount of tissue damaged. Parameters for predicting long-term outcome in such patients have not been clearly delineated, therefore the aim of this study was to investigate this possibility and to test a system that might practicably be used routinely to aid management and predict outcomes of individual stroke patients.
METHODS: A descriptive hospital-based study of the neurological symptoms and signs of 503 patients with ischemic stroke, including severe headache, seizure, eye movement disorder, pupil size, Glasgow Coma Scale (GCS), agitation were analyzed in this study.
RESULTS: In the current study, dilated pupils, agitation, acute onset headache, lower GCS score, seizure, and eye gaze impairment had signif cantly higher prevalence in hemorrhagic stroke patients (P<0.001). However, the rate of gradual progressive headache is significantly higher in ischemic stroke patients (P<0.001).
CONCLUSION: Although this result provides reliable indicators for discrimination of stroke types, imaging studies are still the gold standard modality for diagnosis.
Stroke; Neurologic manifestations; Statistical model
INTRODUCTION
In the developed world, cerebrovascular accidents (CVA) is the third leading cause of death after heart diseases and cancers,[1–3]and is the most common cause of morbidity and prominent disability in survivors,[1,2]where, 20% of patients will be in need of medical care and rehabilitation procedures in the few months after a CVA event.[1,2]On the other hand, CVA wastes a signif cant proportion of health care system budget.[4]
Two types of brain stroke are hemorrhagic and ischemic. Hemorrhagic stroke, which is due to blood vessel rupture, accounts for 20% of CVAs. Ischemic stroke due to brain vessels occlusion and blockage includes 80%.[1,2]
In order to prevent complications and permanent defects, early diagnosis is the key in stroke patients, however, distinguishing the type of stroke plays a crucial role in patient care. Simple clinical findings are helpful in distinguishing the type of stroke,[1,2]but need for diagnostic imaging is an undeniable fact.[5–9]Non-contrast computed tomography (CT) scan is the most commonly used modality to distinguish two types of stroke, but it is not accessible in all hospitals and emergency departments, which may lead to loss of treatment golden time.[2–22]According to this issue, many studies described various clinical findings especially neurological signs and symptoms, and some of them presented formulas to distinguish stroke types based on clinical evaluations. These characteristics including focal or non-focal symptoms, negative or positive symptoms and sudden or gradual onset result in primary segregation of stroke types in emergency department that leads to early diagnosis and treatment. However, previous studies claimed that, neurological signs such as eye gaze and pupil size changes, can be reliable facts to distinguish stroke types.[1–3]
Regarding this issue, in the present study, we aim to identify the rate of neurological f ndings, such as eye signs and symptoms and Glasgow Coma Scale (GCS) changes in stroke patients and evaluate their prevalence in each type of stroke, in order to introduce a guidance to distinguish stroke types that can be more advantageous in districts without CT scan possibility. On the other hand, in developing countries, imaging facilities are not available in most of the small districts and towns, where early diagnosis of ischemic stroke can lead to early patient referral to centers with f brinolytic therapy facilities and decrease in stroke injuries.
METHODS
In the present descriptive study, one stroke center, including Imam Reza hospital with 24 hour access to CT scan, enrolled. As a pilot study designed to determine the prevalence of current study variables in stroke patients referred to these centers, the study group population calculated to be at least 500 patients. In a two-year period, from 2012 to 2013, all patients with neurologic defects complaint with or without decreased level of consciousness were included in our study. Patients with underlying diseases such as, metabolic deficiencies, trauma, and toxicity or peripheral nervous system disorders were excluded. Emergency department (ED) physicians clarif ed their diagnosis on the type of stroke during the first visit after admission, based on clinical f ndings. The presence of impaired eye gaze, GCS level, pupils' size, anisochoria and agitation were carefully examined.
All data including age, sex and examinations, were given to ED physicians in designed checklists. Noncontrast CT (NCT) was performed in order to conf rm the diagnosis in all patients, which is the standard modality to distinguish hemorrhagic and ischemic stroke rapidly. Ninety-five percent of subarachnoid hemorrhages (SAHs) and parenchymal hemorrhage, that are larger than 1 cm, are def nable with brain NCT scan. However, most of the time, infarct lesions are not visible in CT scan in the 6–12 hours time window, and according to the infarct area size, in 1/3 of ischemic CVA patients, rapid onset and mild changes are detectable in CT scan study after approximately 3 hours of signs and symptoms onset. Checklists, along with the computed tomography reports, were used to perform calculations and analysis. In order to analyze demographic and clinical data, chi square test was used for qualitative variables andt-test for quantitative variables.
All patients' data were protected and they were free to leave the study at any stage, however, there were no fees charged for patients participated in study.
RESULTS
Out of 503 patients with stroke diagnosis admitted to emergency department in one center, mean age (SD) was 68.45 (8.76), and the ages range was from 28 to 92 years. About 46.1% of patients were female, and 53.1% were male. The diagnosis was hemorrhagic stroke in 144 patients and ischemic stroke in 359 patients.
Acute headache and agitation were the most prevalent manifestations, that were present in 140 (27.8%) and 139 (27.6%) patients. Eye gaze impairment, seizure and gradual headaches were present in 89 (17.7%), 29 (5%) and 9 (3.8%) patients respectively. During pupil examination, midriatic pupil was observed in 223 (44.3%) patients, and only 2 (0.4%) patients had miosis.
Mean age of patients, each sex proportion and patients manifestations were separated by their diagnosis as listed in Tables 1–3.
In order to distinguish stroke type regarding to clinical examinations especially neurological manifestations, the following variables were studied and analyzed: GCS, acute onset headache, progressive headache, agitation, pupil size, and seizure.

Table 1. Demographic information of hemorrhagic and ischemic strokes patients, admitted to Emam Reza hospital emergency department during 2012–2013
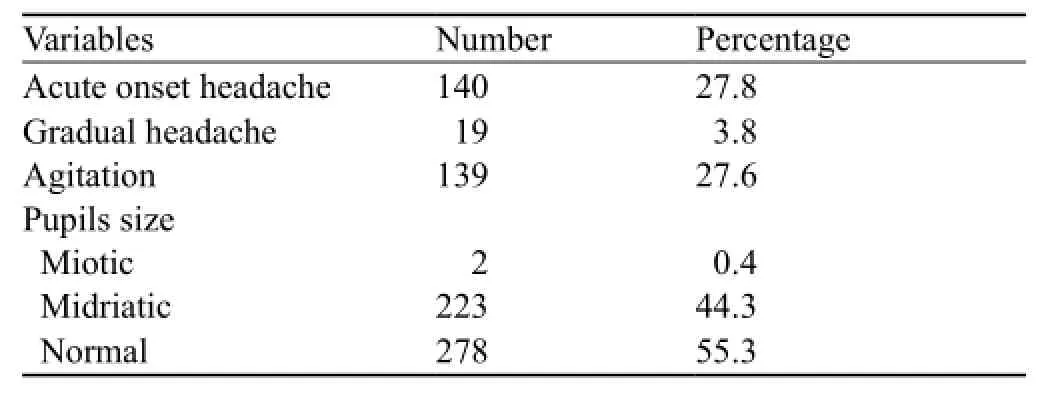
Table 2. Clinical manifestations of hemorrhagic and ischemic strokes patients, admitted to Emam Reza hospital emergency department during 2012–2013

Table 3. Comparing clinical manifestations between hemorrhagic and ischemic strokes patients, admitted to Emam Reza hospital emergency department during 2012–2013
According to GCS records, mean GCS (SD) score in ischemic stroke patients was 12.67 (0.81), however, the minimum score was 7 and the maximum was 15. Though, in hemorrhagic stroke patients, mean (SD) GCS score was 8.97 (0.182), with minimum of 6 and maximum of 15 (independent sample testP<0.001).
During examination, eye gaze impairment was present in 24 (6.7%) ischemic stroke patients and 65 (45.1%) hemorrhagic stroke patients (chi-square testP<0.001). Totally 261 (72.7%) patients among those with an ischemic stroke had normal pupil, but 98 (27.3%) patients had midriatic pupils during examinations. However, midriatic pupils was present in 125 (86.8%) hemorrhagic stroke patients, while 11 (11.8%) were normal, and only 2 (1.4%) patients had miotic pupil (Chi square testP<0.001). Anisocoria was detected only in 10 (2%) patients of this study group and all of them were hemorrhagic stroke victims (6.9%). Out of 503 patients, only 25 (5%) had seizure manifestation, and all of them belonged to the hemorrhagic stroke group (17.4%) (Chi square testP<0.001).
Agitation prevalence was 6.7% among ischemic stroke patients (24 patients) and 79.9% among hemorrhagic patients (115 patients) (Chi square testP<0.001). Seven (19%) patients with acute onset headache were in the ischemic stroke group, and 133 (92.4%) patients with acute onset headache symptoms were in the hemorrhagic stroke group. After being scanned, CT scan reports in ischemic stroke patients claimed, hypo dense lesion in 324 (90.3%) patients, hyper dense artery sign in 328 (91.4%) patients, sulcus effacement in 6 (1.7%) patients, and mass effect in 2 (0.6%) patients. However, in all hemorrhagic stroke patients (n=144) hyper dense lesion was visible.
DISCUSSION
Cerebrovascular accident (CVA) includes any vascular injury that diminishes brain and its derivatives blood flow, and causes various degrees of neurologic dysfunction and disability. Recently, CVA is the third leading cause of death after heart diseases and cancers in the Western world and it affects 700 000 person annually.[1–3,5]In addition, CVA leads to morbidity and prominent disability in 15%–30% of survivors,[1,2]and 20% of patients will require rehabilitation procedures.[1,2]CVA accounts for a significant quota of healthcare budgets and causes excessive healthcare expenses as well. Mortality during hospital admission is 15% and up to 20%–25% during the next 30 days. Although, 50%–70% of the patients recover from the neurological dysfunctions, 15%–30% of stroke victims suffer permanent disabilities.[5–7]Twenty percent of brain strokes are hemorrhagic, which are due to blood vessel rupture, and 80% are ischemic followed by brain vessels occlusion and blockage due to thrombosis or atherosclerosis.[1–2]
There are two types of hemorrhagic stroke, which are intracranial hemorrhage (ICH) and subarachnoid hemorrhage (SAH). Hypertension (HTN), myocardial infarction (MI), thrombolytic consumption are the most common risk factors for hemorrhagic stroke onset.[2]Hemorrhagic strokes have a wide spectrum of clinical manifestations, though acute onset headache, vomitingand severe increases in blood pressure are the most prevalent signs and symptoms, that lead to localized neurological signs, developing in a few minutes.[1,9]Although, these signs and symptoms are not specific for any type of stroke, previous studies proved that, occurrence of acute manifestations most likely propounds the probability of hemorrhagic stroke.
There are three main etiology described for ischemic stroke including, hypo-perfusion, embolism, and thrombosis, which is the most common reason. Signs and symptoms in these patients can be slowly progressive, and can develops over several hours with variable severity.[2]Various manifestations can be present as a result of ischemic stroke, including paresis, ataxia, paralysis, vomiting, and eye gaze, however, occurrence site of these signs depends on the brain area that is being nourished by suffering vessels.[1,2]
Immediate diagnosis and treatment may dramatically diminish the rate of neurological impairment in patients after CVA, and differentiating the type of stroke plays a crucial role in patient management and treatment.[1–2]Although, non-contrast computed tomography scan (NCT scan) is a widely used modality to exclude the presence of hemorrhage in stroke victims due to its ability to prove hemorrhage in first hours after CVA, it is not accessible in all hospitals and emergency departments.[16–22]Early diagnosis is important in stroke patients to prevent permanent defects. Although, the need for diagnostic imaging in distinguishing stroke types is an undeniable fact, in units without imaging facilities, clinical f ndings can be helpful in distinguishing types of stroke.[1,2,9]
Results corresponding with previous studies, claim that study group patients were fine representatives of stroke victims, and this fact indicates that the current study results are applicable to all stroke patients.
In the current study, ischemic stroke diagnosis was the most prevalent stroke type. According to pathophysiology of the CVA, mean age of patients with ischemic stroke was higher than hemorrhagic stroke patients, as expected.[20]
In the current study, statistical analysis claimed that lower GCS scale, agitated mood, acute onset headache, seizure, and midriatic pupil had a higher prevalence in hemorrhagic strokes, which was similar to the Besson study.[20]Comparing the prevalence in the two group of stroke patients showed a significant relation between hemorrhagic stroke onset and these clinical manifestations in patients (P<0.001). This fact suggests that the presence of these signs and symptoms can strongly suggest the type of stroke and help ED physician in primary diagnosis making. On the other hand, since manifestations in ischemic stroke progress over several hours, gradual headache had a higher prevalence in ischemic strokes. Also in this study, occurrence of this symptom propounds more probability of ischemic stroke in patients (P<0.001).
After all, though clinical manifestations are helpful in distinguishing stroke types during primary visit, imaging is still the gold standard diagnostic method for brain stroke patients. However, in small district hospitals and centers, where imaging facilities are not accessible, these results can be applicable for patient management, treatment and timely referral to stroke center.
CONCLUSION
In the current study, various clinical manifestations of different types of CVA are evaluated, in order to distinguish hemorrhagic and ischemic strokes that categorize the signs and symptoms by their prevalence in each type of stroke. Even though the results proved signif cant correlation between stroke types and specif c clinical findings, further studies are required to identify each manifestation's value in stroke type anticipation. It may be better to use some new scoring such as NIHSS in combination with the signs and symptoms.
Funding:None.
Ethical approval:The study was approved by the Ethical Committee.
新型农村社会养老保险试点分析与对策——以彭泽县天红镇为例……………………………………… 欧阳勤 欧阳燕(6/28)
Conf icts of interest:All authors declare that they have no conf ict of interest.
Contributors:Haghighi SHO proposed the study and wrote the f rst draft. All authors read and approved the f nal version of the paper.
REFERENCES
1 Marx J, Hockberger R, Walls R. Rosen's Emergency Medicine, 6th edition, 2006; 1606–1619.
2 Tintinalli JE, Kelen GD, Stapczynski JS. Emergency Medicine: A Comprehensive Study Guide, Sixth Edition. 2004; 1382–1389.
3 American Heart Association: Heart Diseale and stroke statistics-2004 update. Dallas, Tex, American Heart Association, 2003.
4 Broderick J, Brott T, Kothari R, Miller R, Khoury J, Pancioli A, et al. The Greater Cincinnati/Northern Kentucky Stroke Study: preliminary f rst-ever and total incidence rates of stroke among blacks. Stroke. 1998;29(2):415–21.
5 Williams GR, Jiang JG, Matchar DB, Samsa GP. Incidence and occurrence of total (f rst-ever and recurrent) stroke. Stroke. 1999;30(12):2523–8.
7 Smith RW, Scott PA, Grant RJ, Chudnofsky CR, Frederiksen SM. Emergency physician treatment of acute stroke with recombinant tissue plasminogen activator: a retrospective analysis. Acad Emerg Med. 1999;6(6):618–25.
8 Lewandowski CA, Frankel M, Tomsick TA, Broderick J, Frey J, Clark W, et al. Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: Emergency Management of Stroke (EMS) Bridging Trial. Stroke. 1999;30(12):2598–605.
9 Brott T, Adams HP Jr, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–70.
10 Lyden P, Lu M, Jackson C, Marler J, Kothari R, Brott T, et al. Underlying structure of the National Institutes of Health Stroke Scale: results of a factor analysis. NINDS tPA Stroke Trial Investigators. Stroke. 1999;30(11): 2347–54.
11 DeGraba TJ, Hallenbeck JM, Pettigrew KD, Dutka AJ, Kelly BJ. Progression in acute stroke: value of the initial NIH stroke scale score on patient stratification in future trials. Stroke. 1999;30(6):1208–12.
12 Bozkurt S, Arslan ED, Köse A, Ayrık C, Yılmaz A, Dündar GA. Lingual angioedema after alteplase treatment in a patient with acute ischemic stroke. World J Emerg Med. 2015;6(1):74–6.
13 Grotta JC, Chiu D, Lu M, Patel S, Levine SR, Tilley BC, et al. Agreement and variability in the interpretation of early CT changes in stroke patients qualifying for intravenous rtPA therapy. Stroke. 1999;30(8):1528–33.
14 Schellinger PD, Jansen O, Fiebach JB, Hacke W, Sartor K. A standardized MRI stroke protocol: comparison with CT in hyperacute intracerebral hemorrhage. Stroke. 1999;30(4):765–8.
15 Linfante I, Llinas RH, Caplan LR, Warach S. MRI features of intracerebral hemorrhage within 2 hours from symptom onset. Stroke. 1999;30(11):2263–7.
16 Wardlaw JM, del Zoppo G, Yamaguchi T. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2000;(2):CD000213.
17 Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363(9411):768–74.
18 No authors listed. A randomized trial of tirilazad mesylate in patients with acute stroke (RANTTAS). The RANTTAS Investigators. Stroke. 1996;27(9):1453–8.
19 Bogousslavsky J, Van Melle G, Regli F. The Lausanne Stroke Registry: analysis of 1 000 consecutive patients with f rst stroke. Stroke. 1988;19(9):1083–92.
20 Besson G, Robert C, Hommel M, Perret J. Is it clinically possible to distinguish nonhemorrhagic infarct from hemorrhagic stroke? Stroke. 1995;26(7):1205–9.
21 Celani MG, Righetti E, Migliacci R, Zampolini M, Antoniutti L, Grandi FC, et al. Comparability and validity of two clinical scores in the early differential diagnosis of acute stroke. BMJ. 1994;308(6945):1674–6.
22 Whiteley W, Wardlaw J, Dennis M, Lowe G, Rumley A, Sattar N, et al. The use of blood biomarkers to predict poor outcome after acute transient ischemic attack or ischemic stroke. Stroke. 2012;43(1):86–91.
Received March 26, 2016
Accepted after revision September 16, 2016
Samad Shams Vahdati, Email: sshamsv@yahoo.com
World J Emerg Med 2017;8(1):34–38
10.5847/wjem.j.1920–8642.2017.01.006
猜你喜欢
杂志排行
World journal of emergency medicine的其它文章
- Comparison of extracorporeal and conventional cardiopulmonary resuscitation: A meta-analysis of 2 260 patients with cardiac arrest
- The association of layperson characteristics with the quality of simulated cardiopulmonary resuscitation performance
- Cardiopulmonary resuscitation knowledge and attitude among general dentists in Kuwait
- Simplif ed point-of-care ultrasound protocol to conf rm central venous catheter placement: A prospective study
- Clinical and historical features of emergency department patients with pericardial effusions
- A comparison of perspectives on costs in emergency care among emergency department patients and residents
