下颌髁突矢状骨折髓内髓外双重内固定术的临床应用
2016-11-04陈传俊陈晓阳陈静
陈传俊陈晓阳陈静
1.皖南医学院口腔医学院,芜湖 241002;2.安徽医科大学第三附属医院口腔颌面外科,合肥 230061;3.安徽济民肿瘤医院口腔科,合肥 230011
·临床研究·
下颌髁突矢状骨折髓内髓外双重内固定术的临床应用
陈传俊1陈晓阳2陈静3
1.皖南医学院口腔医学院,芜湖 241002;
2.安徽医科大学第三附属医院口腔颌面外科,合肥 230061;
3.安徽济民肿瘤医院口腔科,合肥 230011
目的 探讨髓内及髓外双重内固定在下颌髁突矢状骨折开放复位内固定中的应用价值。方法 采用髓内髓外双重内固定术治疗18例24侧髁突矢状骨折,固定方法:单一螺钉或克氏针行髓内固定,配合一块钛板行髓外固定,伴发他处骨折者同期行精确复位固定。术后通过拍摄CT和全景X线片评价钛板固定情况、骨折段复位精准度及稳固性,通过临床检查评价咬合关系、开口度、开口型。结果 术后X线全景片或CT检查显示,24侧髁突矢状骨折段均未发现术后旋转移位,对位良好;钛板和螺钉无扭曲、折断和松脱。术后咬合关系、开口度、开口型恢复良好。结论 髓内髓外双重内固定具有抗骨折段旋转作用,髓内螺钉和髓外钛板在空间上互不干扰,是下颌骨髁突矢状骨折固定的良好方法。
髁突矢状骨折; 坚强内固定; 髓内固定; 髓外固定
颌面部外伤患者发生下颌髁突矢状骨折(sagittal fracture of the mandibular condyle,SFMC)时,下颌髁突内侧的骨折段常因翼外肌的牵拉而发生向前、内、下方的移位,早期多表现为髁突高度降低,后期常发生颞下颌关节强直,尤其是在伴发下颌骨前份骨折且没有精准复位的状态下更容易发生关节强直[1-4]。对于发生了骨折段移位的SFMC,除儿童以外,目前国内外在治疗方案的选择上逐渐趋于统一,即采用手术开放复位内固定进行治疗;但是就移位骨折段的固定方法而言,则存在多种方法并存的局面:单个微型钛板固定[5]、骨折段取出回植双微型钛板或单板固定[6-7]、单个长皮质钉固定等[8-9]。上述固定方法常因翼外肌的牵引作用而发生一些术后并发症,如单个长皮质钉固定可发生骨折段旋转,单个微型钛板固定可发生钛板扭曲甚至折断,骨折段取出后再回植有导致骨吸收甚至骨坏死的可能。为解决现有固定方法存在的缺陷,本文使用髓内和髓外双重内固定方法治疗SFMC,取得了良好的效果,现报告如下。
1 材料和方法
1.1 患者资料
本组病例来自2002—2015年累积的18例SFMC患者(共24侧),其中12例为单侧SFMC,6例为双侧SFMC,伴发下颌骨他处骨折4例。男14例,女4例,年龄18~80岁。致伤原因:8例为轿车驾驶车祸伤,4例为摩托车驾驶事故伤,3例为骑自行车事故伤,2例为运动性损伤,1例为斗殴致伤。所有的患者均为单侧或双侧SFMC伴骨折段移位,且经CT或全景X线片确诊。受伤至手术时间为5~16 d,平均7.8 d。
1.2 外科复位方法
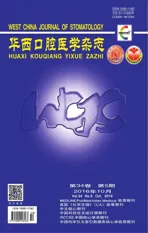
术前于上下牙槽突安放支抗钉实施颌间弹性牵引。全身麻醉下以耳屏前的拐杖型切口入路,分离达关节囊,T形切开髁突颈部的关节囊附着从而暴露髁突残端,由于髁突残端的阻挡使得术者的视野和器械难以抵达移向前下内方的骨折段,从而增加了骨折段复位的难度,故笔者使用提骨钩勾住下颌乙状切迹用力向足向牵拉,以加大关节间隙及周围的操作空间(图1),再辅以神经拉钩或牙周膜剥离子等纤细的器械轻轻夹持或勾住移位的骨折段使之复位。固定分两个步骤进行。1)髓内固定:平行于髁突横轴,在骨折段复位的状态下自髁突外极向内极方向钻孔,穿经髁突残端和骨折段,以等同于髁突内外极之间距离长度的皮质螺钉旋入或克氏针插入(图2左)。2)髓外固定:用0.6 mm的四孔微型钛板横跨骨折线安放于皮质表面,与髓内固定螺钉或克氏针呈十字交叉(不平行)并固定(图2右)。最后将移位或撕裂的关节盘复位缝合,分层关闭创口。伴发下颌他处骨折者同期行精确复位固定。次日实施颌间牵引并持续2周,嘱患者进软食2周。术后随访,随访时间为10~25个月,平均为16个月。
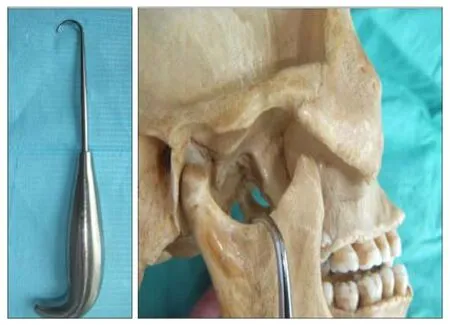
图 1 使用提骨钩(左)足向牵拉以扩大关节间隙和手术野(右)Fig 1 A lift bone hook used (left) to grapple the sigmoid notch with caudal traction to widen the joint space (right)
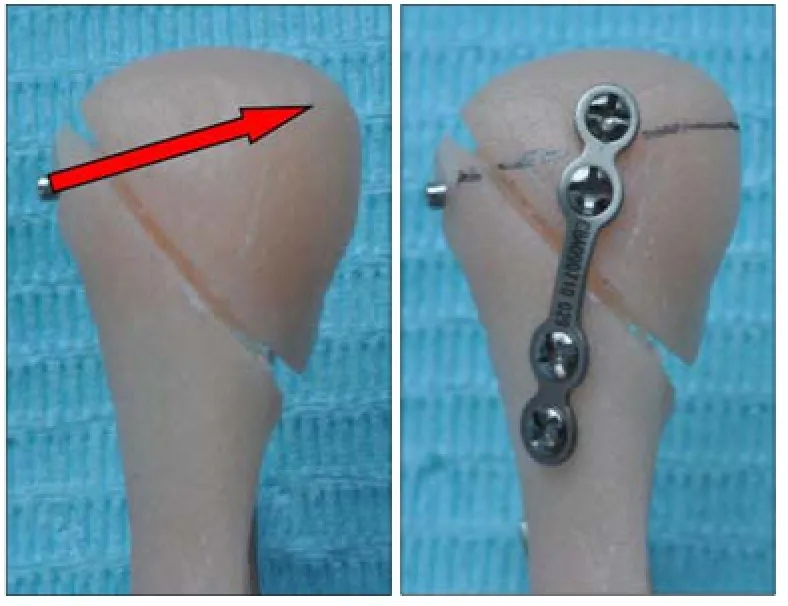
图 2 髓内髓外双重内固定Fig 2 Extramedullary fixation combined with intramedullary fixa- tion
1.3 效果评价
术后拍摄CT和全景X线片来评价钛板固定情况、骨折段复位精准度及稳固性,通过临床检查评价患者咬合关系的恢复情况,并检查患者的开口度和开口型。
2 结果
在24侧SFMC中,有2例患者出现暂时性面神经损伤,主要表现为额皱变浅,半年后均恢复正常;其余无术中和术后并发症。术后X线全景片或CT检查显示:骨折段对位良好,无旋转移位情况发生,髁突形态正常(图3);无钛板及螺钉松脱、扭曲或折断。术后咬合关系恢复良好,开口度及开口型恢复正常。
图 3 1例患者的术前(左)及术后(右)CTFig 3 Preoperative (left) and postoperative (right) CT scan of a patient
3 讨论
有关SFMC的内固定方式方法有诸多报道。有学者[5-6]将前内下移位的内侧骨折段解剖分离并剥离翼外肌附着后取出,在体外钻孔并安放内固定钛合金板,然后将骨折段连同钛合金板复位回植固定。这种外科处理方法有值得商榷的地方,因为骨折段一旦失去肌肉附着,血液循环即被中断,骨折段有发生吸收甚至坏死的可能性[7-8]。有学者[8-9]曾推荐利用单一长螺钉固定SFMC骨折段,但笔者在使用单一长螺钉固定这一方法时曾遇见意外情况,即骨折段固定术后在翼外肌的强力牵引下发生旋转移位,长螺钉犹如穿插于冰糖葫芦的中轴,成了骨折段移位的旋转轴。Meng等[10]和Xin等[11]提出可以使用两个长螺钉固定,以避免骨折段旋转。也有学者[6]使用两个微型钛板固定SFMC骨折段,也是为了避免骨折段的旋转移位。这些方法较好地解决了骨折段旋转移位的问题,但从解剖上看,颞下颌关节是小关节,髁突本身是较小的指状突起,发生SFMC时,有时骨折线靠近髁突内极,其内侧移位的骨折段则是一微小的骨块,当使用两个螺钉髓内固定或是使用两个钛板髓外固定时,一方面微小的骨折段安放钛板或螺钉常显得空间不足,另一方面反复多个钻孔有导致骨折段破碎的可能。笔者也曾使用两个长螺钉固定SFMC骨折段,在操作过程中常发生骨折段破碎的现象。综上所述,SFMC现有的固定方式均存在一定的缺陷,本文所采用的髓内和髓外双重内固定有以下优点。1)抗旋转作用。髓内髓外联合双重固定,特别是固定装置的十字交叉安放,具有抗旋转作用,避免了单一长螺钉髓内固定出现术后骨折段旋转移位的可能性。2)固定件分配空间合理,髓内髓外双重固定合理地分配了固定件占用的空间,互不干扰,特别适合那些内侧移位的小骨折段固定。
SFMC内固定方式目前尚不统一,其治疗方案的选择也是从争议走向趋同的过程。由于SFMC容易导致颞下颌关节强直,故其治疗方案的选择备受关注[4,9,12-15]。近年来的公开资料越来越多地倾向于对成人SFMC选择外科开放复位内固定,儿童的SFMC选择保守治疗方案[16-18]。He等[13-14]通过回顾性调查分析发现,SFMC伴发下颌他处骨折可因下颌弓外展而扩大,髁突外极或髁突的残端向外上移位而抵触颧弓发生粘连,形成关节强直。Duan等[4]通过分析CT及MRI资料显示,关节盘的受损或移位与SFMC的创伤性关节强直高度相关,这是因为骨折段或髁突外极残端与颞骨关节面间失去正常阻隔结构而直接相抵,从而诱发关节强直。Meng等[19]于2009年提出翼外肌牵张成骨假说,解释翼外肌在创伤性颞下颌关节强直发生中的作用。该假说认为,翼外肌的动力牵拉使得骨折段和髁突残端间的间隙渐进性成骨,大量的成骨和周边结构的融合导致关节强直,其骨生成机制和牵张成骨类似。这一假说已被动物模型所证实[20-21]。综上所述,伴随着对创伤性颞下颌关节强直发生机制的理解深化,SFMC治疗方案的选择也在发生变化,外科精准复位内固定术逐渐成为被广泛认同的方案。
[1] Long X, Li X, Cheng Y, et al. Preservation of disc for treatment of traumatic temporomandibular joint ankylosis[J]. J Oral Maxillofac Surg, 2005, 63(7):897-902.
[2] 王霄, 张益, 李江明. 髁突矢状骨折继发颞下颌关节强直动物模型的建立[J]. 北京大学学报(医学版), 2011, 43(6): 903-907.
Wang X, Zhang Y, Li JM. Experimental establishment of animal model of temporomandibular joint ankylosis secondary to condylar sagittal fracture[J]. J Peking Univ (Health Sci), 2011, 43(6):903-907.
[3] Arakeri G, Brennan PA. The role of concomitant mandibular fractures in disc displacement and development of TMJ ankylosis secondary to sagittal fractures of the mandibular condyle[J]. Int J Oral Maxillofac Surg, 2011, 40(11):1333-1335.
[4] Duan DH, Zhang Y. A clinical investigation on disc displacement in sagittal fracture of the mandibular condyle and its association with TMJ ankylosis development[J]. Int J Oral Maxillofac Surg, 2011, 40(2):134-138.
[5] 景捷, 赵洪伟, 孙刚, 等. 脱位性髁突矢状骨折手术治疗的近期疗效观察[J]. 华西口腔医学杂志, 2007, 25(1):58-60.
Jing J, Zhao HW, Sun G, et al. Surgical treatment of dislocation sagittal fracture of the mandibular condyle[J]. West Chin J Stomatol, 2007, 25(1):58-60.
[6] Jing J, Han Y, Song Y, et al. Surgical treatment on displaced and dislocated sagittal fractures of the mandibular condyle [J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2011, 111(6):693-699.
[7] Pereira MD, Marques A, Ishizuka M, et al. Surgical treatment of the fractured and dislocated condylar process of the mandible[J]. J Craniomaxillofac Surg, 1995, 23(6):369-376.
[8] Vesnaver A. Open reduction and internal fixation of intraarticular fractures of the mandibular condyle: our first experiences[J]. J Oral Maxillofac Surg, 2008, 66(10):2123-2129.
[9] Luo S, Li B, Long X, et al. Surgical treatment of sagittal fracture of mandibular condyle using long-screw osteosynthesis[J]. J Oral Maxillofac Surg, 2011, 69(7):1988-1994.
[10] Meng FW, Liu YP, Hu KJ, et al. Use of a temporary screw for alignment and fixation of sagittal mandibular condylar fractures with lateral screws[J]. Int J Oral Maxillofac Surg, 2010, 39(6):548-553.
[11] Xin P, Jiang B, Dai J, et al. Finite element analysis of type B condylar head fractures and osteosynthesis using two positional screws[J]. J Craniomaxillofac Surg, 2014, 42(5):482-488.
[12] Liu CK, Jing CX, Li W, et al. Observational study of surgical treatment of sagittal fractures of mandibular condyle [J]. J Craniofac Surg, 2015, 26(4):e359-e364.
[13] He D, Cai Y, Yang C. Analysis of temporomandibular joint ankylosis caused by condylar fracture in adults[J]. J Oral Maxillofac Surg, 2014, 72(4):763.e1-763.e9.
[14] He D, Ellis E 3rd, Zhang Y. Etiology of temporomandibular joint ankylosis secondary to condylar fractures: the role of concomitant mandibular fractures[J]. J Oral Maxillofac Surg, 2008, 66(1):77-84.
[15] Ferretti C, Bryant R, Becker P, et al. Temporomandibular joint morphology following post-traumatic ankylosis in 26 patients[J]. Int J Oral Maxillofac Surg, 2005, 34(4):376-381.
[16] Baker AW, McMahon J, Moos KF. Current consensus on the management of fractures of the mandibular condyle. A method by questionnaire[J]. Int J Oral Maxillofac Surg, 1998, 27(4):258-266.
[17] Vesnaver A, Ahčan U, Rozman J. Evaluation of surgical treatment in mandibular condyle fractures[J]. J Craniomaxillofac Surg, 2012, 40(8):647-653.
[18] Liu Y, Bai N, Song G, et al. Open versus closed treatment of unilateral moderately displaced mandibular condylar fractures: a meta-analysis of randomized controlled trials[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2013, 116(2): 169-173.
[19] Meng FW, Zhao JL, Hu KJ, et al. A new hypothesis of mechanisms of traumatic ankylosis of temporomandibular joint[J]. Med Hypotheses, 2009, 73(1):92-93.
[20] Liu CK, Liu P, Meng FW, et al. The role of the lateral pterygoid muscle in the sagittal fracture of mandibular condyle (SFMC) healing process[J]. Br J Oral Maxillofac Surg, 2012, 50(4):356-360.
[21] Wu D, Yang XJ, Cheng P, et al. The lateral pterygoid muscle affects reconstruction of the condyle in the sagittal fracture healing process: a histological study[J]. Int J Oral Maxillofac Surg, 2015, 44(8):1010-1015.
(本文编辑 吴爱华)
Extramedullary fixation combined with intramedullary fixation in the surgical reduction of sagittal mandibular condylar fractures
Chen Chuanjun1, Chen Xiaoyang2, Chen Jing3.
(1. Stomatological School, Wannan Medical College, Wuhu 241002, China; 2. Dept. of Oral and Maxillofacial Surgery, The Third Affiliated Hospital of Anhui Medical University, Hefei 230061, China; 3. Dept. of Stomatology, Anhui Jimin Tumor Hospital, Hefei 230011, China)
Supported by: National Natural Science Foundation of China (815500037). Correspondence: Chen Chuanjun, E-mail: ccj6318 @sina.com.
Objective This study aimed to evaluate the clinical effect of extramedullary fixation combined with intramedullary fixation during the surgical reduction of sagittal mandibular condylar fractures. Methods Twenty-four sagittal fractures of the mandibular condyle in18 patients were fixed by two appliances: intramedullary with one long-screw osteosynthesis or Kirschner wire and extramedullary with one micro-plate. The radiologically-recorded post-operative stability-associated complications included the screw/micro-plate loosening, micro-plate twisting, micro-plate fractures, and fragment rotation. The occluding relations, the maximalinter-incisal distances upon mouth opening, and the mandibular deflection upon mouth opening were evaluated based on follow-up clinical examination. Results Postoperative panoramic X-ray and CT scans showed good repositioning of the fragment, with no redislocation or rotation, no screw/plate loosening, and no plate-twisting or fracture. Clinical examination showed that all patients regained normal mandibular movements, ideal occlusion, and normal maximal inter-incisal distances upon mouth opening. Conclusion Extramedullary fixation combined with intramedullary fixation is highly recommended for sagittal condylar fractures because of the anti-rotation effect of the fragment and the reasonable placement of the fixation appliances.
sagittal condylar fracture; rigid internal fixation; intramedullary fixation; extramedullary fixation
R 782.4
A [doi] 10.7518/hxkq.2016.05.008
2016-05-23;
2016-07-24
国家自然科学基金(815500037)
陈传俊,教授,博士,E-mail:ccj6318@sina.com
陈传俊,教授,博士,E-mail:ccj6318@sina.com