Clinical observation on acupuncture combined with Chinese medicine and rehabilitation training for subacute stroke patients
2015-05-18LuoKaitao罗开涛ZhuGaofeng朱高峰ShenLaihua沈来华GaoFeng高峰QianLifeng钱立锋
Luo Kai-tao (罗开涛), Zhu Gao-feng (朱高峰), Shen Lai-hua (沈来华), Gao Feng (高峰), Qian Li-feng (钱立锋)
Jiaxing Hospital of Chinese Medicine, Zhejiang 314000, China
Clinical Study
Clinical observation on acupuncture combined with Chinese medicine and rehabilitation training for subacute stroke patients
Luo Kai-tao (罗开涛), Zhu Gao-feng (朱高峰), Shen Lai-hua (沈来华), Gao Feng (高峰), Qian Li-feng (钱立锋)
Jiaxing Hospital of Chinese Medicine, Zhejiang 314000, China
Objective:To observe the clinical effect of combining acupuncture, Chinese medicine and rehabilitation training for subacute stroke.
Acupuncture Therapy; Acupuncture Medication Combined; Rehabilitation; Activities of Daily Living; Stroke
Along with the aging of population, stroke affects over two million people each year. Thanks to medical advance and public awareness, many patients can survive stroke; however, stroke is still a major cause of disability. Approximately 80%-90% stroke patients develop spasticity within one month (subacute, 30-40 d after stroke). It’s therefore of great significance to manage spasticity in this stage to promote isolated movement and restore motor function of the affected limb[1-3]. To investigate the clinical effect on subacute stroke, we’ve treated stroke patients with acupuncture, Chinese medicine and rehabilitation training. The results are now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
The diagnostic criteria in Western medicine werebased on theKey Diagnostic Points for Cerebrovascular Diseasesat the 4th National Conference of Chinese Medical Association[4].
Diagnosis for cerebral hemorrhage: Sudden onset during physical exertion or emotional fluctuation, recurrent vomiting, headache and elevated blood pressure, rapid progression with complications of disturbance of consciousness, hemiplegia and other local focus symptom of nervous system; a history of hypertension; recommended examination: CT scan; lumbar puncture of cerebrospinal fluid often contains blood and increased pressure (no blood in approximately 20% patients).
Diagnosis for cerebral infarction: Onset during a resting state; no notable headache or vomiting; a slow onset with gradual progression, often related to cerebral atherosclerosis, arteritis and blood diseases; clear consciousness or mild disturbance within 1-2 d after onset; signs and symptoms of internal carotid artery and/or vertebrobasilar artery system; recommended examinations: CT scan or MRI examination; lumbar puncture of cerebrospinal fluid does not contain blood.
1.1.2 Diagnostic criteria in Chinese medicine
The diagnostic criteria in Chinese medicine were based on theCriteria for Stroke Diagnosis and Therapeutic Efficacy Assessment[5].
Major symptoms: Hemiplegia, mental confusion, slurred speech or aphasia, abnormal sensation of one-sided body and deviation of the mouth and tongue.
Associated symptoms: Headache, dizziness, changes in pupil, choking while drinking water, deviation of the eyes, ataxia; a sudden onset with warning signs; aged over 40.
A diagnosis can be made with two or more major symptoms or one major symptom and two associated symptoms, coupled with onset, contributing factors, warning signs and age. Otherwise imaging can be combined to confirm the diagnosis.
1.2 Inclusion criteria
Those who met the diagnostic criteria for stroke in Chinese medicine; cerebral infraction or hemorrhage confirmed by CT scan or MRI examination; initial stroke during subacute stage (30-40 d), National Institutes of Health stroke scale (NIHSS) score ranged from 4 to 24; aged between 35 and 80 years; initial onset or previous onset that had no sequela and did not affect NIHSS score, modified Ranking scale (MRS) ≤1 point; willing to participate in this trial and signed the informed consent.
1.3 Exclusion criteria
Those who have subarachnoid hemorrhage, transient ischemic attack (TIA) or complications of intracranial tumor, arterial aneurysm, vascular malformation, cerebral cysticercosis, intracerebral schistosomiasis, encephalitis, meningitis, hydrocephalus and sequela due to brain trauma; non-arteriosclerotic thrombotic cerebral infarction (cardioembolism, hypercoagulation, exfoliation of vascular wall, and arteritis, etc.); 3-40 d after onset; limb motor dysfunction, emotional disturbance, cognitive impairment or speech disorders due to other reasons (surgery, trauma and congenital disability, etc.) before stroke; having severe heart conditions, cardiac, hepatic and renal failure, malignant cancer, digestive tract bleeding, critical infection or severe diabetes; receiving other clinical trials during the treatment; having mental disorders, multiple skin lesions and joint contracture; uncooperative during the treatment; failed to sign the informed consent; pregnant or breast-feeding women.
1.4 Drop-out and rejection criteria
Those who failed to meet the diagnostic criteria or were misdiagnosed; failed to follow the treatment protocol, <4 times of treatment per week and <35 times of total treatment in the treatment group; having received other therapies (such as surgery, endovascular intervention, and arterial and venous thrombolysis or Chinese patent medicine that may affect the research findings) during treatment; failed to finish the courses of treatment for efficacy evaluation or having incomplete observation data; failed to reach for follow-up study.
1.5 Statistical method
The SPSS 13.0 version software was used for statistical analysis. Measurement data that accord with positive distribution were expressed withusing thet-test. Non-normal data were described using M (QL, QU). The same evaluation index for each subject was repeatedly measured 4 times, and analysis of variance was used for data analysis. The Wilcoxon orF-test was used for inter-group comparison. APvalue of less than 0.05 indicates a statistical significance.
1.6 General data
A total of 120 cases treated at Acupuncture and Rehabilitation Department, Jiaxing Hospital of Chinese Medicine between January 2012 and December 2013 were randomly allocated into a treatment group (n=60) and a control group (n=60). There were no betweengroup statistical differences in gender, age, disease duration, motor function, neurologic deficit score and TCM symptoms scores (P>0.05), indicating that the two groups were comparable (Table 1).
2 Treatment Methods
2.1 Observation group
2.1.1 Basic treatment
The treatment protocol was based upon the2010 China Guidelines for Prevention of Secondary Stroke in Patients with Ischemic Stroke or Transient IschemicAttack. The treatment mainly deals with hypertension, coronary artery disease, diabetes, respiratory infection, urinary infection and enteritis. The treatment purposes are to control blood pressure, blood sugar, alleviate inflammation, maintain water, electrolyte and acid-base equilibrium, improve cerebral circulation and activate cerebral metabolism.

Table 1. Between-group comparison on baseline data
2.1.2 Routine rehabilitation training
The rehabilitation protocol was based upon Brunnstrom’s stage[6]: good postural control display, visual and proprioceptive stimuli, bed and bedside activities and physical agents for stage I-III; and exercise to boost normal voluntary movements of upper limb, hand function training, activities of daily living (ADL), occupational therapy, balanced sitting and standing, shifting from sitting to standing, walking exercise, indoor walking and outdoor activities for stage IV-V, each training lasted for 2 h.
2.1.3 Acupuncture therapy
Points: Baihui (GV 20), Sishencong (EX-HN 1), Shangxing (GV 23), Fengchi (GB 20), Fengfu (GV 16), Jianyu (LI 15), Quchi (LI 11), Shousanli (LI 10), Waiguan (TE 5), Hegu (LI 4), Shangbaxie [1 cun superior to Baxie (EX-UE 9)], Huantiao (GB 30), Yanglingquan (GB 34), Zusanli (ST 36), Juegu (GB 39) and Taichong (LR 3).
Method: Acupuncture therapy was performed by professionally trained doctors based on same location and needling techniques. The patient was asked to take a side-lying position, placing the affected side on top. After routine sterilization, the above points were punctured using filiform needles of 40-75 mm in length. Baihui (GV 20), Sishencong (EX-HN 1) and Shangxing (GV 23) were fast inserted to the underlying layer of galea aponeurotica, followed by 1.5-2.0 cun subcutaneously and reducing manipulation by twirling. Fengchi (GB 20) was punctured 1.0-1.5 cun towards the tip of the nose. Jianyu (LI 15) was punctured 1.5-2.0 cun obliquely downward, followed by reinforcing manipulation by lifting and thrusting to enable the needling sensation radiate towards Hegu (LI 4), coupled with a slow abduction of the affected upper limb to alleviate spasticity and 1-minute reinforcing manipulation by lifting and thrusting. Hegu (LI 4) was punctured 1.0-1.5 cun towards Sanjian (LI 3), followed by reducing manipulation by lifting and thrusting to enable the index finger twitching or extension of all five fingers. Shangbaxie (Extra) was punctured 0.5-1.0 cun obliquely towards the palm, followed by reducing manipulation by lifting and thrusting to enable the needling sensation to radiate to finger tips for extension of all fingers. Huantiao (GB 30) was punctured (from 3 cun lateral to the sacral hiatus) 2.5-3.0 cun perpendicularly, followed by reinforcing manipulation by lifting and thrusting to enable the needling sensation radiate downward. Yanglingquan (GB 34) was punctured 1.0-1.5 cun obliquely outward and downward to enable the lower limb to twitch 3 times. Zusanli (ST 36) was punctured 1.5-2.0 cun perpendicularly to enable the needling sensation to radiate towards the dorsum of the foot. The rest points were punctured and followed by even reinforcing-reducing manipulation. The needles were retained for 30 min. The treatment was done once a day, 8-10 points for each treatment.
2.1.4 Chinese medicine
Ingredients ofBu Yang Huan Wu Tang(Tonify the Yang to Restore Five Tenths Decoction):Huang Qi(Radix Astragali),Chi Shao(Radix Paeoniae Rubra),Chuan Xiong(Rhizoma Chuanxiong),Dang Gui(Radix Angelicae Sinensis),Di Long(Pheretima),Tao Ren(Semen Persicae),Hong Hua(Flos Carthami),Sang Zhi(Ramulus Mori),Wu Shao She(Zaocys),Quan Xie(Scorpio),Fu Ling(Poria) andJiao Liu Qu(Massa Medicata Fermentata Praeparata). The above formula was decocted with water. The 400 mL decoction was taken twice orally, 200 mL for each time. Seven formulae were taken for 1 week, for a total of 8 weeks.
The standard rehabilitation training and acupuncture were performed 5 times a week, for a total of 8 weeks.
2.2 Control group
Patients in the control group received the same internal and rehabilitation training (same method and course of treatment) as those in the treatment group.
3 Therapeutic Efficacy Evaluation
3.1 Observation indices
3.1.1. Neurologic deficit severity
The neurologic deficit was evaluated using the NIHSS. The NIHSS contains 11 items including level of consciousness (0-3 points), visual field (0-3 points), motor arm and leg (0-4 points), sensory (0-2 points) limb ataxia (0-2 points), and language and speech (0-3points). The total score ranges from 0 to 30, with higher scores indicating a more severe condition.
3.1.2 Motor function assessment
The patients’ motor function was assessed using the Fugl-Meyer assessment scale (FMA). The FMA includes motor impairment assessment for upper and lower extremities. Each item has 3 grades: cannot be performed at all (0 point), performed partly (1 point) and performed faultlessly (2 points). The total score for upper extremity ranges from 0 to 66; the total score for lower extremity ranges from 0 to 34. The total score ranges from 0 to 100. The scoring on the FMA can be interpreted as follows: score <50 points, severe motor impairment (grade I); score of 50-84 points, significant motor impairment (grade II); score of 85-95 points, moderate motor impairment (grade III); and score of 96-99 points, mild motor impairment (grade IV).
3.1.3 ADL assessment
The ADL was evaluated using the Barthel index (BI). The BI contains 10 items, each item is scored from 0-15 points and the total score ranges from 0 to 100. The scoring on the BI can be interpreted as follows: score>60 points, almost independent and needs minimal help; score of 41-60 points, partially dependent and needs help; score of 21-40 points, very dependent; and score ≤20 points, totally dependent.
The above indices were evaluated by specific personnel before treatment, after 30-day, 60-day treatments, and 3 months after treatment.
3.2 Safety evaluation
The body temperature, heart rate, respiration, blood pressure and blood sugar were all recorded, coupled with adverse reactions and complications.
3.3 Criteria of therapeutic efficacy
The self-made therapeutic efficacy criteria were established according to theCriteria for Stroke Diagnosis and Therapeutic Efficacy Assessment(trial)[5]and our clinical experience.
Marked effect: The symptoms and signs disappeared, and the patient could basically live independently.
Effect: The symptoms and signs improved, and the patient could walk by stick, or had basic self-care ability.
Failure: The symptoms and signs remained unchanged.
3.4 Treatment results
3.4.1 Between-group comparison on NIHSS
After treatment, the NIHSS in both groups were significantly decreased (P<0.05), and there was a between-group statistical significance at the same time point (P<0.05), indicating that the neurologic deficit in both groups were improved; however, the improvement was more noticeable in the treatment group than that in the control group (Table 2).
3.4.2 Between-group comparison on FMA
After treatment, the FMA scores in both groups were significantly decreased (P<0.05), and there was a between-group statistical significance at the same time point (P<0.05), indicating that the motor impairment in both groups were improved; however, the improvement was more noticeable in the treatment group than that in the control group (Table 3).
3.4.3 Between-group comparison on BI
After treatment, the BI scores in both groups were significantly decreased (P<0.05), and there was a between-group statistical significance at the same time point (P<0.05), indicating that the ADL in both groups were improved; however, the improvement was more noticeable in the treatment group than that in the control group (Table 4).
3.4.4 Between-group comparison on clinical effects
After treatment, the total effective rate was 91.7% in the treatment group, versus 80.0% in the control group, showing a statistical difference (P<0.05) and indicating a better effect in the treatment group than that in the control group (Table 5).
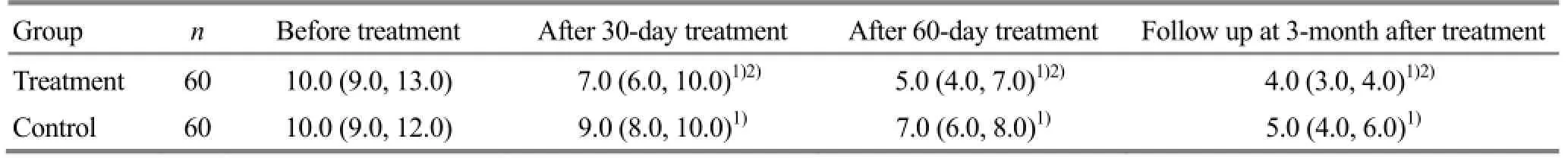
Table 2. Between-group comparison on NIHSS score [M (QL, QU), point]
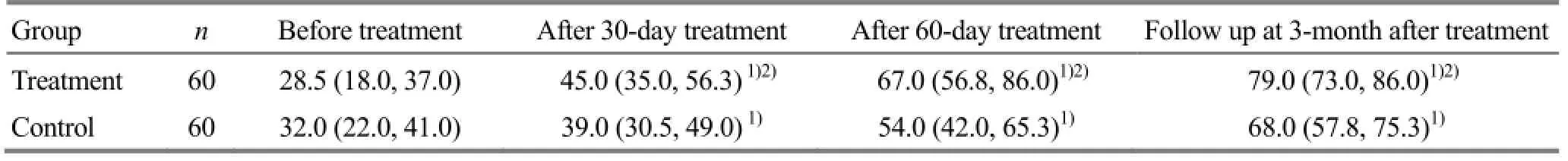
Table 3. Between-group comparison on FMA score [M (QL, QU), point]
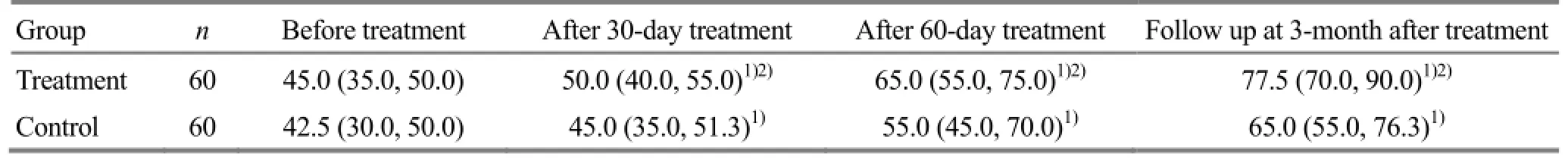
Table 4. Between-group comparison on BI score [M (QL, QU), point]
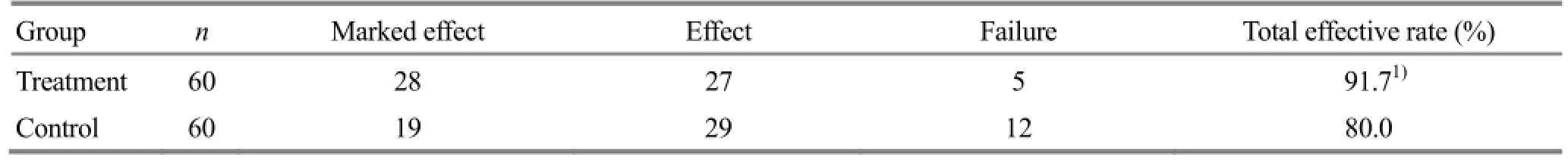
Table 5. Between-group comparison of clinical efficacy (case)
4 Discussion
Stroke is the leading cause of adult disability. Approximately 3/4 of stroke survivors experience total disability and 40% of them develop severe disability. Post-stroke limb dysfunction can greatly affect the patients’ quality of life and increase social and economic cost[7-9]. Early intervention of acupuncture and rehabilitation can effectively prevent aggravation, improve therapeutic efficacy and reduce disability[10]. One month after onset is known as subacute stage. Patients in this stage often have stable vital signs following thrombolysis, defibrase, anticoagulation, intracranial decompression, brain protection, anti-infection and management of blood pressure and sugar[11-12]. In Chinese medicine, pathogenesis of stroke in subacute stage is deficiency of qi and blood and blockage of brain collaterals[13]. Early intervention of acupuncture can coordinate yin and yang, unblock meridians, circulate qi and blood, and restore muscle strength[14].
Based upon the treatment strategy of reinforcing healthy qi and reducing pathogenic factors, the treatment protocol includes points on the head, the affected side and points according to pattern identification. First, points on the head including Baihui (GV 20), Sishencong (EX-HN 1), Fengchi (GB 20), Fengfu (GV 16) and Shangxing (GV 23) were punctured first to refresh the brain. Then, points on the affected side including Jianyu (LI 15), Quchi (LI 11), Shousanli (LI 10), Waiguan (TE 5), Hegu (LI 4), Huantiao (GB 30), Yanglingquan (GB 34) and Juegu (GB 39) were punctured to relax muscles. Neiguan (PC 6), Zusanli (ST 36), Pishu (BL 20), Shenshu (BL 23), Geshu (BL 17) and Sanyinjiao (SP 6) were combined to reinforce qi, nourish yin, resolve stasis and phlegm and harmonize Zang-fu organs. Even reinforcing and reducing, reinforcing and reducing manipulation were applied in sequence to balance yin and yang, regulate Zang-fu organs and restore limb function. Of the ingredients inBu Yang Huan Wu Tang(Tonify the Yang to Restore Five Tenths Decoction), a large dose ofHuang Qi(RadixAstragali) was used as the major component;Dang Gui(Radix Angelicae Sinensis),Chi Shao(Radix Paeoniae Rubra),Tao Ren(Semen Persicae) andHong Hua(Flos Carthami) were used as supplementary components. The formula acts to reinforce qi, circulate blood and resolve stasis. Modern studies have proven thatHuang Qi(Radix Astragali) can increase superoxide dismutase (SOD) activity, inhibit platelets, improve cerebral circulation and accelerate neurologic recovery[15]. In addition to chronic paralysis, the dosage ofHuang Qi(Radix Astragali) inBu Yang Huan Wu Tang(Tonify the Yang to Restore Five Tenths Decoction) was often gradually increased from 15 g. A smaller dose is recommended for patients with a surging forceful or wiry forceful pulse or having associated symptoms including headache, dizziness or feverish sensation in the chest. A bigger dose can be used for those with a thready pulse, and a pale tongue.
In modern medicine, stroke can be hemorrhagic and ischemic; both share the same pathogenesis of blood stasis, which can be both etiological factor and pathological product. Since stagnant blood can obstruct circulation and increase vascular pressure, ischemia may transform into hemorrhage and hemorrhage may cause re-bleeding. The study findings have suggested that combining acupuncture and Chinese medicine in addition to basic treatment and rehabilitation training can obtain better results in subacute stroke patients.
Conflict of Interest
There was no conflict of interest in this article.
Acknowledgments
This work was supported by Zhejiang Key Research Program of Traditional Chinese Medicine for Prevention and Treatment of Major Diseases (浙江省中医药防治重大疾病攻关计划项目, No. 2011ZGG003).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 18 March 2015/Accepted: 19 April 2015
[1] Lou BD, Zhang W, Liu Z, Lin H, Li JX, Wang JJ. Clinical assessment on muscle tone-balancing needling technique on post-stroke spasticity and disability. Zhongguo Zhen Jiu, 2010, 30 (2): 89-92.
[2] He JW, Bai HM. Clinical observation on needling cervical and lumbar Jiaji points for 96 cases with post-stroke hypermyotonia. Zhongyi Zazhi, 2012, 53 (16): 1401-1403.
[3] Wang XF, Liu HL, Li JD, Wang LP. Exploration on TCM pattern of ‘Continuous Comprehensive Rehabilitation Stroke Unit’. Zhongyi Zazhi, 2012, 53 (5): 373-375.
[4] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380
[5] Emergency Coordination Group for Brain Diseases, State Administration of Traditional Chinese Medicine. Criteria for stroke diagnosis and therapeutic efficacy assessment (trial). Beijing Zhongyiyao Daxue Xuebao, 1996, 19 (1): 55-56.
[6] Chen LF, Fang JQ, Wu YY, Ma RJ, Xu SY, Shen KL, Luo KT, Gao F, Bao YH. Acupuncture for subacute post-stroke motor dysfunction: a multicenter randomized controlled clinical trial. Zhongguo Zhen Jiu, 2014, 34 (4): 313-318.
[7] Fu HL, Li SB. Current treatment and future prospect for acute ischemic stroke. Neimenggu Mingzu Daxue Xuebao, 2009, 15(5): 163-166.
[8] Camarata PJ, Heros RC, Latcha RE. Brain attack: the rationale for treating stroke as a medical emergency. Neurosurgery, 1994, 34 (1): 144-157.
[9] Fang XH, Wang CX, Mei LP, Liu M, Ji XM, Li LM. Research advance on epidemiological study of stroke. Zhonghua Liuxingbinxue Zazhi, 2011, 32(9): 847-853.
[10] Luo KT, Yang XB, Fan DH, Shen ZF, Shen LH. Early intervention of combining acupuncture and rehabilitation training in acute cerebral infarction. Zhonghua Zhongyiyao Xuekan, 2013, 31(4): 843-845.
[11] Huang RX, Guo YP. Staging and grouping treatment protocol for stroke (draft). Linchuang Shenjingbingxue Zazhi, 2001, 14(1): 60-62.
[12] Cui GX, Song CZ, Yue SW. Effect of power cycling on walking and activities of daily living in patients with subacute stroke. Zhongguo Kangfu Yixue Zazhi, 2009, 24(6): 530-532.
[13] Ruan YM. Therapeutic efficacy observation on combiningBu Yang Huan Wu Tangand acupuncture for ischemic stroke. Shizhen Guoyi Guoyao, 2013, 24 (5): 1194-1195.
[14] Wang WD, Ding ZQ, Chen HZ, Qiao YQ. Early intervention of combining functional training and acupuncture for the quality of life in stroke patients. Zhongguo Kangfu Yixue Zazhi, 2012, 27 (2): 147-149.
[15] Pahan K, Sheikh FG, Namboodiri AM, Sinqh I. Lovastatin and phenylacetate inhibit the induction of nitric oxide synthase and cytokines in rat primary astrocytes, microglia, and macrophages. J Clin Invest, 1997, 100 (11): 2671-2679.
Translator: Han Chou-ping (韩丑萍)
针药并用结合康复训练治疗亚急性期中风病临床观察
目的:观察针药并用结合康复训练治疗亚急性期中风病的临床疗效。方法:将120例亚急性期中风病患者, 按就诊顺序采用随机数字表法随机分为治疗组和对照组, 每组60例。对照组采用常规康复治疗, 治疗组在常规康复治疗的基础上给予针刺和口服中药治疗。于治疗前、治疗30 d、治疗60 d以及治疗结束后3个月使用美国国立卫生研究院卒中量表(National Institute of Health stroke scale, NIHSS)评价患者神经功能缺损程度, 使用Fugl-Meyer运动功能量表(Fugl-Meyer assessment scale, FMA)评价患者的运动功能, 利用Barthel指数 (Barthel index, BI)评价患者的日常生活活动能力(activities of daily living, ADL), 同时进行中医症状积分以评价患者中医症状变化情况。结果:两组患者治疗30 d、60 d后及治疗结束后3个月的NIHSS、FMA、BI及中医症状积分均与本组入院时有统计学差异(均P<0.05); 两组相同时间点的各指标间差异亦有统计学意义(均P<0.05)。结论:针药并用结合康复训练可改善亚急性期中风病患者的神经功能缺损、运动功能和日常生活能力, 其疗效优于单独常规康复治疗。
针刺疗法; 针药并用; 康复; 日常生活活动; 中风
R246.6 【
】A
Author: Luo Kai-tao, vice chief physician.
Email: lkt740183@163.com
Methods:A total of 120 subacute stroke cases were randomly allocated into a treatment group (n=60) and a control group (n=60). Patients in the control group received standard rehabilitation therapy alone, whereas patients in the observation group received additional acupuncture and Chinese medicine. Before treatment, after 30-day and 60-day treatments, and 3 months after treatment, the neurologic deficit severity was evaluated using the National Institute of Health stroke scale (NIHSS); the motor function was evaluated using the Fugl-Meyer assessment scale (FMA); the activities of daily living (ADL) was evaluated using the Barthel index (BI); and the changes of traditional Chinese medicine (TCM) symptoms were evaluated according to TCM symptom scores.
Results:After 30-day, 60-day treatments, and 3 months after treatment, the NIHSS, FMA, BI and TCM symptoms scores were statistically different from those before treatment in both groups (allP<0.05); and there were between-group statistical differences at same time points (allP<0.05).
Conclusion:Combining acupuncture, Chinese medicine and rehabilitation training can improve neurologic deficit, motor function and ADL in subacute stroke patients and its efficacy is better than rehabilitation therapy alone.
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Survey on acupuncture treatment of neurogenic dysphagia and analysis of regularity of acupoint selection
- Clinical study on nape cluster acupuncture for 50 cases of migraine
- Combining acupuncture and copper-tube moxibustion for 39 cases of recurrent peripheral facial paralysis
- Study on metabolic intensity value changes of points on the face using thermal chromatography technology
- Tuina along the meridians combined with Chinese medicine for motor functions and activities of daily living in patients with post-stroke upper limb spasticity
- Clinical effect observation on acupuncture for chronic obstructive pulmonary disease
