Tuina along the meridians combined with Chinese medicine for motor functions and activities of daily living in patients with post-stroke upper limb spasticity
2015-05-18HanShukai韩淑凯MaZhiwei马志伟ZhangNa张娜ChenCaiping陈彩平RenZhanchang任占昌
Han Shu-kai (韩淑凯), Ma Zhi-wei (马志伟), Zhang Na (张娜), Chen Cai-ping (陈彩平), Ren Zhan-chang (任占昌)
1 Wangdu County Hospital of Chinese Medicine, Hebei 072450, China
2 Wangdu County Hospital, Hebei 072450, China
Clinical Study
Tuina along the meridians combined with Chinese medicine for motor functions and activities of daily living in patients with post-stroke upper limb spasticity
Han Shu-kai (韩淑凯)1, Ma Zhi-wei (马志伟)1, Zhang Na (张娜)2, Chen Cai-ping (陈彩平)1, Ren Zhan-chang (任占昌)1
1 Wangdu County Hospital of Chinese Medicine, Hebei 072450, China
2 Wangdu County Hospital, Hebei 072450, China
Objective:To observe the effect of combining Chinese medicine and tuina along the meridians on motor function and activities of daily living (ADL) in patient with post-stroke upper limb spasticity.
Tuina; Massage; Drugs, Chinese Herbal; Spasm; Post-stroke Syndrome; Activities of Daily Living; Rehabilitation
Stroke has high incidence, mortality and relapse rates in China. Spasticity is commonly seen in post-stroke patients, often manifesting as increased muscle tone, restricted joint motion or even joint contracture and malformation. Spasticity affects patients’ physical activities, and physical inactivity worsens spasticity. As a result, it greatly affects patient’s quality of life, family care and social cost. More than 80% of daily activities are performed by upper limbs and normal quality of life depends on upper limb functions. It’s therefore of great significance to alleviate upper limb spasticity, control abnormal motion pattern and enhance isolated movement in stroke patients. We’ve treated this condition with tuina along the meridians and self-made Chinese medicine. The results are now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
This was based on theKey Diagnostic Points for Cerebrovascular Diseases[1]and diagnostic criteria for cerebral infarction and hemorrhage made at the 4th National Conference of Chinese Medical Association, coupled with CT scan or MRI examination.
The diagnosis for upper limb spasticity was based on the criteria inPhysical Medicine and Rehabilitation, Clinical Diagnosis and Treatment Guidelines[2]: increased resistance during passive movement of upper limbs, severe muscle spasticity manifests as joint rigidity at a certain angle of flexion or extension; local joint and muscle pain, long-time spasticity may cause muscle or tendon contracture; tendon hyperreflexia of the spastic upper limb; and impaired upper limb motor function and activities of daily living (ADL).
1.2 Inclusion criteria
Those who met the diagnostic criteria; aged between 47 and 80 years, having stable vital signs and clear consciousness; muscle tone ≥1 but ≤4 according to the modified Ashworth scale (MAS); II, III and V stage by Brunnstrom approach; having a duration of less than 3 months; willing to participate in this trial and signed the informed consent.
1.3 Exclusion criteria
Those with critical or acute unstable conditions, coupled with unconsciousness or cognitive impairment; having severe complications of heart, lung, liver and kidney diseases, diabetes or bleeding tendency; and those who have recently taken sedatives or muscle relaxants.
1.4 Statistical method
Statistical analysis was performed with SPSS version 14.0 software. Measurement data were expressed withThet-test was used for inter-group and intra-group (paired data) differences before and after treatment. The Chi-square test was used for grouped data and rank sum test for ranked data. APvalue of less than 0.05 indicates a statistical significance.
1.5 General data
A total of 220 eligible cases (156 inpatients and 64 outpatients) treated in Acupuncture and Cerebrovascular Departments, Wangdu County Hospital of Chinese Medicine were recruited in this study. They were randomly allocated into a treatment group (n=110) and a control group (n=110). Cases in the treatment group aged between 45 and 72 years and their disease duration lasted from 7 d to 2 months. Cases in the control group aged between 47 and 81 years old and their disease duration lasted from 6 d to 2.1 months. There were no significant between-group differences in baseline data (P>0.05), indicating that the two groups were comparable (Table 1).
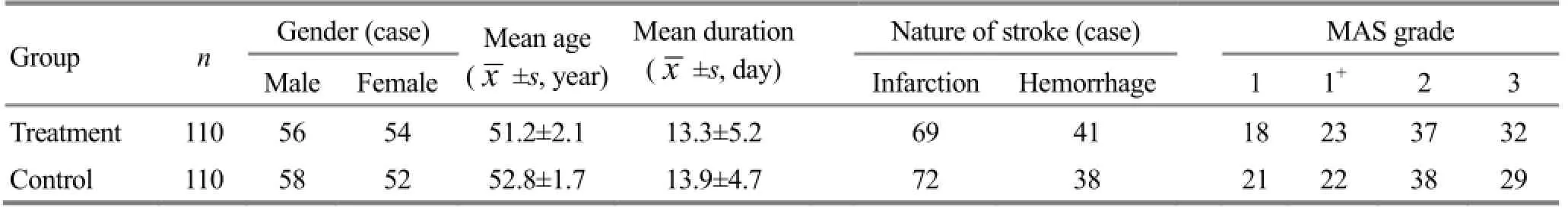
Table 1. Between-group comparison of baseline data
2 Treatment Methods
Patients in both groups received treatment after their conditions were stabilized.
2.1 Treatment group
2.1.1 Tuina along the meridians
According to the interior-exterior connection of meridians, the meridians on the upper limb were classified into three groups: the Lung Meridian and the Large Intestine Meridian; the Pericardium Meridian and the Triple Energizer Meridian; the Heart Meridian and the Small Intestine Meridian. First, the practitioner applied heavy fast Gun-rolling (Figure 1) and Na-grasping (Figure 2) manipulations to the three yin meridians of Hand from the shoulder joint towards the wrist; then applied gentle slow Rou-kneading (Figure 3) and Ca-rubbing (Figure 4) manipulations to the three yang meridians of hand from the wrist towards the shoulder joint. The practitioner was supposed to increase the force gradually until the patient felt soreness, numbness, distension and mild pain. Lasting, forceful and even force were especially focused on the Five Shu-Transmitting points and Luo-Connecting points. The treatment was done 15 min each time, twice a day.

Figure 1. Gun-rolling manipulation

Figure 2. Na-grasping manipulation

Figure 4. Ca-rubbing manipulation
2.1.2 Chinese medicine
Patients took spasticity-alleviating and meridianunblocking formula orally.
Ingredients: 10 g ofJiang Can(Bombyx Batryticatus),Quan Xie(Scorpion),Dang Gui(Radix Angelicae Sinensis) andBai Shao(Radix Paeoniae Alba) respectively,Shui Zhi(Hirudo) 3 g, and 15 g ofHuang Qi(Radix Astragali) andSheng DiHuang(Radix Rehmanniae) respectively.
Method: The above ingredients were ground into fine powder and stored in a bottle after filtration by a 100-mesh sieve. Patients took 15 g with warm water for each dose, 3 doses a day.
2.2 Control group
Patients in the control group received anti-spasticity rehabilitation training once a day. The training includes good limb position, maintaining of joint range of motion, alleviation of spasticity around body movement control points, static muscle stretching, and passive movement and passage.
The therapeutic efficacies in the two groups were observed after 3 weeks of treatment.
3 Treatment Results
3.1 Observation indices
3.1.1 Upper limb motor function assessment
Simplified Fugl-Meyer assessment scale (FMA) for the upper extremity was used to assess the upper limb motor function[3]. A total of 60 points indicate grade-5 muscle strength and completely normal upper limb motor function, whereas a zero point indicates grade-0 muscle strength.
3.1.2 ADL assessment
The modified Barthel index (MBI) was used for assessment of patients’ ADL[4]. Total scores range from 0 to 100, with higher scores indicating greater independence.
3.1.3 Muscle tone assessment
The modified Ashworth Scale (MAS) was used to assess muscle hypertonia (shoulder intortor, elbow flexors and wrist flexors)[5].
MAS grading includes 0 (0 point), 1 (1 point), 1+(2 points), 2 (3 points), 3 (4 points) and 4 (5 points), with higher scores indicating increased hypertonia.
3.2 Results
3.2.1 Between-group comparison on FMA score
Before treatment, there was no significant betweengroup difference in FMA score (P>0.05). After treatment, the FMA scores in both groups were increased (P<0.05) and there was a significant between-group difference (P<0.05). This indicates that the upper limb motor functions were improved in both groups but it was more significant in the treatment group than that in the control group (Table 2).
Table 2. Between-group comparison on FMA scores before and after treatment, point)
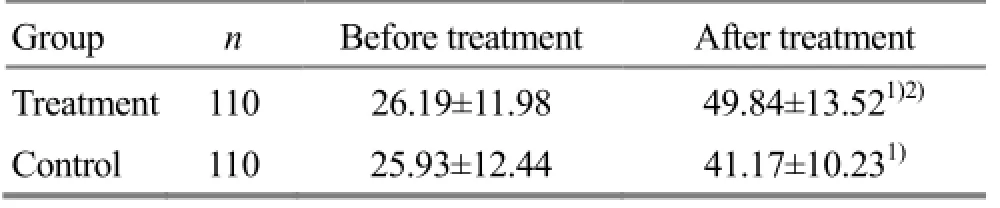
Table 2. Between-group comparison on FMA scores before and after treatment, point)
Note: Intra-group comparison before and after treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
?
3.2.2 Between-group comparison of MBI score
Before treatment, there was no significant betweengroup difference in MBI score (P>0.05). After treatment, the MBI scores in both groups were increased (P<0.05) and there was a significant between-group difference (P<0.05). This indicates that the ADL were improved in both groups but the improvement was more significant in the treatment group than that in the control group (Table 3).
3.2.3 Between-group comparison of MAS score
Before treatment, there were no between-group statistical significances in MAS scores (P>0.05). After treatment, the MAS scores in both groups were increased (P<0.05) and there was a between-group statistical significance (P<0.05). This indicates that the MAS scores were decreased in both groups but the decrease was more significant in the treatment group than that in the control group (Table 4).
Table 3. Between-group comparison on MBI scores before and after treatment (point)
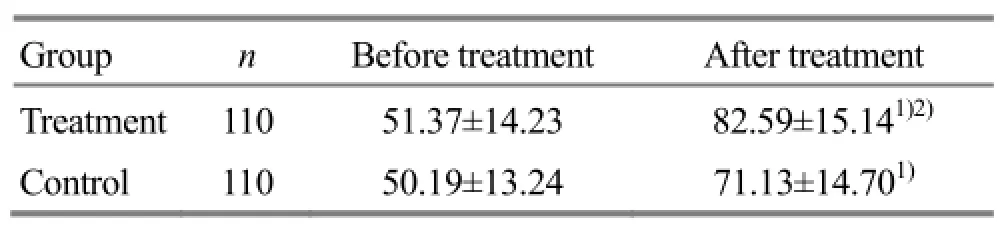
Table 3. Between-group comparison on MBI scores before and after treatment (point)
Note: Intra-group comparison before and after treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.01
?
Table 4. Between-group comparison on MAS scores before and after treatment (, point)
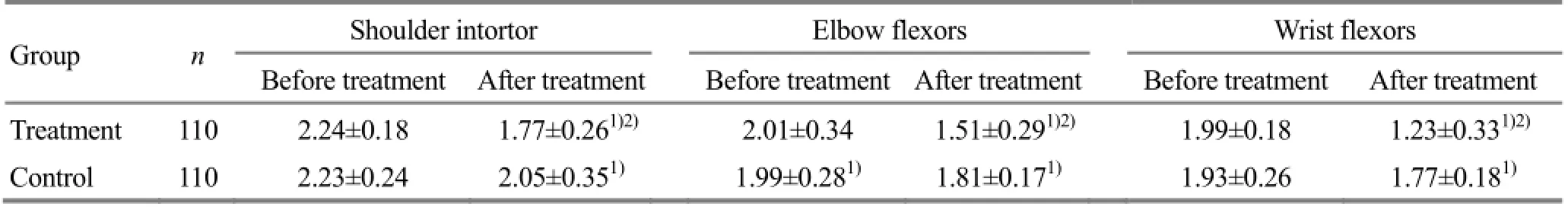
Table 4. Between-group comparison on MAS scores before and after treatment (, point)
Note: Intra-group comparison before and after treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
?
4 Discussion
Post-stroke hemiplegic spasticity occurs when the high-level neural center fails to control involuntary motor function and low-level center (spinal cord) takes over and thus abnormal motor pattern emerges. This often manifests as spasticity of the flexor muscles in the upper limb and flaccidity of the extensor muscles. Patients may present with abnormal elbow flexion, wrist flexion, forearm pronation and finger flexion, etc. hypermyotonia or persistent spasticity may affect remodeling of normal motor pattern. Consequently, it’s of great significance to alleviate spasticity, control abnormal motor pattern and promote isolated movement for the recovery of stroke patients.
In Chinese medicine, this condition falls under the category of ‘wind stroke’ and ‘spasticity syndrome’. Based upon its clinical manifestations, the pathogenesis of post-stroke upper limb spasticity can be described as qi deficiency with phlegm retention, blockage of meridians, malnourishment of muscles and tendons and yin-yang imbalance. The treatment strategies are therefore to reinforce qi, unblock meridians, circulate blood, resolve stasis, remove wind and resolve phlegm. Of major ingredients in the spasticity-alleviating and meridian-unblocking formula,Huang Qi(Radix Astragali) tonifies qi and lifts yang,Shui Zhi(Hirudo) circulates blood and resolves stasis, andJiang Can(Bombyx Batryticatus) unblocks meridians. Modern pharmacological studies have shown thatHuang Qi(Radix Astragali) can significantly dilate peripheral, coronary, cerebral, intestinal and renal vessels, improve microcirculation, increase capillary resistance, prevent capillary fragility and permeability induced by physical and chemical factors and alleviate inflammation[6].Shui Zhi(Hirudo) can break blood and resolve stasis.Jiang Can(Bombyx Batryticatus) is pungent in taste and enters the Liver and Lung Meridians. It can alleviate spasticity, remove wind, resolve phlegm-dampness, unblock meridians, and balance yin and yang.Dang Gui(Radix Angelicae Sinensis) can nourish and circulate blood, resolve stasis and unblock meridians.Bai Shao(Radix Paeoniae Alba) andSheng Di Huang(Radix Rehmanniae) can reinforce qi, nourish yin and prevent yin from being damaged by dryness. In summary, the formula can reinforce qi, resolve stasis, circulate blood, unblock meridians and harmonize yin and yang[7-8].
Applying to specific body points, tuina therapy can regulate physiological or pathological state, unblock meridians, harmonize qi and blood, reinforce healthy qi, remove pathogenic factors, and balance yin and yang.
Tuina along the meridians is based on the theories on Zang-fu organs and meridians. The twelve regular meridians are associated with internal Zang-fu organs. Yin meridians are associated with the Zang organs (interior), whereas yang meridians are associated with the Fu organs (exterior). Physiologically, the interior-exteriorly connected meridians are connected. Pathologically, they can be mutually affected. Patients with post-stroke upper limb spasticity present with spasticity of the flexor muscles and flaccidity of the extensor muscles, i.e., yin-yang imbalance. The treatment strategies of tuina therapy are to reinforce healthy qi and remove pathogenic factors. Reducingtuina manipulation along the three hand yin meridians can relax muscles and tendons, regulate the functions of Zang-fu organs and meridians, coordinate different parts of the body and balance excitability and inhibition. At the same time, reinforcing tuina manipulation along the three hand yang meridians can activate upper limb nerve, improve neurotrophy, boost nerve tissue metabolism and thus increase nerve excitability and help recovery of the impaired nerve. On the other hand, it can circulate blood and increase muscle tone. To sum up, tuina along the meridians can alleviate spasticity by inhibiting nerve excitability through stimulating dominant muscle groups and increase muscle tone by activating nerve/muscle excitability through stimulating non-dominant muscle groups. This can further activate muscle proprioceptor to maintain and coordinate normal muscle tone and motor function and result in isolated movement[9-11].
This study has proven that tuina along the meridians combined with Chinese medicine can substantially reduce hypertonia of spastic upper limb, increase ADL and upper limb motor function. On one hand, this combined method can reinforce yang meridians, unblock meridians and harmonize qi and blood. On the other hand, it can reduce yin meridians, remove wind, resolve phlegm and alleviate spasticity. Combining external tuina therapy and internal regulation can regulate meridians and Zang-fu organs and restore homeostasis of the body.
Conflict of Interest
There was no conflict of interest in this article.
Acknowledgments
This work was supported by Scientific Research Fund Project of Hebei Provincial Administration Bureau of Traditional Chinese Medicine (河北省中医药管理局科研基金资助项目, No. 2013145).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 15 March 2015/Accepted: 23 April 2015
[1] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[2] Chinese Medical Association. Clinical Diagnosis and Treatment Guidelines: Fascicle of Physical Medicine and Rehabilitation. Beijing: People’s Medical Publishing House, 2005: 11-14.
[3] Zhu YL. Neurology. Beijing: People’s Medical Publishing House, 2001: 151-153.
[4] Shen T. Research advance on acupuncture for hypermyotonia following stroke. Gansu Zhongyi, 2003, 16(10): 6.
[5] Yan TB, Dou ZL. Practical Paralysis Rehabilitation. Beijing: People’s Medical Publishing House, 1999: 112.
[6] Shen YJ. Chinese Pharmacology. Shanghai: Shanghai Scientific and Technical Publishers, 1997: 165.
[7] Zuo YF, Han SK, Cao WJ, Ma HJ, Yang WH. Influence ofBuqi Huatan Tongluodecoction and acupuncture therapy of exterior-interior related meridian points on the quality of life in patients with shoulder-hand syndrome after stroke. Zhongxiyi Jiehe Xinnaoxueguanbing Zazhi, 2011, 9(7): 807-808.
[8] Sun WG, Han SK, Cao WJ, Sun ZY, Liu JH, Zuo YF, Wang Y. Influence ofBuqi Huatan Tongluodecoction and acupuncture therapy of exterior-interior related meridian points on the depression in patients with shoulder-hand syndrome after stroke. Zhongyiyao Daobao, 2012, 18(3): 16-18.
[9] Mao GY, Xu JR. Acupoint massage with meridians for shoulder periarthritis. Shanghai Zhongyiyao Zazhi, 2004, 38(2): 49-50.
[10] Xie GY, Wang HM. Hemiparalysis in different stages treated with collateral massage combined with acupuncture. Zhejiang Zhongyiyao Daxue Xuebao, 2006, 30(4): 408-409.
[11] Tang JL, Han SK. Observation on curative effect of patients with upper extremity spasm after cerebral apoplexy treated with Chinese traditional manipulation along the meridians. Huli Yanjiu, 2011, 25(7): 1839-1840.
Translator: Han Chou-ping (韩丑萍)
循经推拿加中药对脑卒中后上肢痉挛患者运动功能和日常生活活动能力的影响
目的:观察循经推拿结合中药对脑卒中后上肢痉挛患者运动功能和日常生活活动能力(activities of daily living, ADL)的影响。方法:将220例脑卒中后上肢痉挛患者采用随机数字表法随机分为治疗组和对照组, 每组110例, 治疗组给予循经推拿结合止痉通络中药口服治疗, 对照组给予常规康复治疗, 共治疗3星期。于治疗前后分别采用简式Fugl-Meyer量表(Fugl-Meyer assessment scale, FMA)、改良Barthel指数(modified Barthel index, MBI)和改良Ashworth痉挛量表(modified Ashworth scale, MAS)评定患者的运动功能、ADL和肌张力。结果:治疗组患者FMA评分、MBI评分、肩内旋肌、屈肘肌及腕屈肌肌张力评分及对照组均较治疗前明显改善(P<0.05), 并且上述指标均以治疗组患者的改善程度较显著, 与对照组间差异均具有统计学意义(P<0.05)。结论:循经推拿法结合止痉通络方能明显缓解患侧屈肌肌张力, 从而显著提高患者的运动功能和日常生活活动能力。
推拿; 按摩; 中草药; 痉挛; 中风后遗症; 日常生活活动; 康复
R244.1 【
】A
Author: Han Shu-kai, vice chief physician.
E-mail: hanshukai1975@163.com
Methods:A total of 220 patients with post-stroke upper limb spasticity were randomly allocated into a treatment group (n=110) and a control group (n=110). Patients in the treatment group received tuina along the meridians combined with spasticity-alleviating and collateral-unblocking Chinese medicine, whereas patients in the control group received routine rehabilitation therapy. Patients in both groups were treated for 3 weeks. Then the patients’ motor function, ADL and muscle tone were evaluated before and after treatment using the Fugl-Meyer assessment scale (FMA), modified Barthel index (MBI) and modified Ashworth scale (MAS).
Results:After treatment, the FMA scores, MBI scores, and muscle (shoulder intortor, elbow flexors and wrist flexors) tones were significantly improved (P<0.05), but the improvement was more significant in the treatment group than that in the control group (P<0.05).
Conclusion:Tuina along the meridians combined with spasticity-alleviating and collateral-unblocking Chinese medicine can substantially alleviate muscle tone on the affected side and remarkably improve the patients’ motor function and ADL.
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Survey on acupuncture treatment of neurogenic dysphagia and analysis of regularity of acupoint selection
- Clinical study on nape cluster acupuncture for 50 cases of migraine
- Combining acupuncture and copper-tube moxibustion for 39 cases of recurrent peripheral facial paralysis
- Study on metabolic intensity value changes of points on the face using thermal chromatography technology
- Clinical observation on acupuncture combined with Chinese medicine and rehabilitation training for subacute stroke patients
- Clinical effect observation on acupuncture for chronic obstructive pulmonary disease
