胰十二指肠切除术在高龄患者中的应用
2011-04-26马晋峰木村理平井一郎森谷敏辛竹下明子山西省肿瘤医院普外科太原03003日本山形大学医学部消化器外科山形9909585
马晋峰, 木村理, 平井一郎, 森谷敏辛, 竹下明子 (山西省肿瘤医院普外科, 太原 03003;日本山形大学医学部消化器外科, 山形 990-9585)
Pancreaticoduodenectomy for periampullary cancer,defined as cancers arising from the ampulla of Vater or near-by i.e.,duodenum,distal common duct or the head of the pancreas,is the only possible curative treatment,and it may be the best palliative procedure for cases where resection is noncurative[1-4].At the same time,pancreaticoduodenectomy is also suitable for some benign diseases such as chronic pancreatitis and intraductal papillary mucinous neoplasm(IPMN)etc.Previously pancreatoduodenectomy had an operative mortality of up to 25%,but with the greater experience gained by centralization of treatment the mortality has decreased to 2% -8%.Furthermore,increase of survival time after pancreaticoduodenectomy for cancer has also been reported during the past decades[4-7].
In 2003,population of the elderly(65 years and over)was 24.31 million citizens and constituted 19.0 percent of the total population in Japan,its largest scale on record in either number or percentage terms.The elderly population was expected to continue expanding rapidly in the years ahead,topping the 20 percent level by 2006 in Japan[8].The aging of the Japanese population has generated an interest in the suitability of older patients for major surgical procedures.Pancreaticoduodenectomy is a major surgical procedure which has mainly restricted to younger patients in a good physical condition.A few of studies have shown a decreasing operative morbidity and mortality after pancreaticoduodenectomy and suggest that age is not a contraindication to pancreaticoduodenectomy.Furthermore,the cumulative survival rate is not different from that obtained in younger patients[9-13].
During the recent years,we have no upper age limit for pancreaticoduodenctomy at the affiliated hospital of Yamagata University School of Medicine.Both the two oldest patients treated with pancreatiduodenctomy were 81 years old,and the post-operative courses of these two patients were uneventful.We collected the detailed clinical data to assess how age affects the operative and long-term outcome of patients aged 75 years and over who were treated with pancreaticoduodenectomy.
1 Patients and Methods
Between January,2002 and December,2006,72 patients underwent pancreaticoduodenectomy at the affiliated hospital of Yamagata University School of Medicine for presumed peri-ampullary neoplasms,chronic pancreatitis and gastric neoplasms.There were 42 males and 30 females with ages ranging from 38 to 81 years.There were 18 patients aged 75 years and over and 54 patients younger than 75 years old.
Two senior surgeons did all the pancreaticoduodenectomies.The surgical procedure for pancreaticduodenectomy was a Whipple procedure.If the disease had been diagnosed with malignant neoplasms pre-operatively,resection of all the regional lymph nodes and connective tissue was added during the Whipple procedure,including an extensive dissection of all structures in the hepatoduodenal ligament,along the hepatic artery and its ramifications,along the portal vein,and at the front surface of the head of the pancreas,and along the mesenteric vein and mesenteric artery.The retroperitoneal space at the post surface of the head of the pancreas,in the front of the right kidney,V.cava,and aorta,was also dissected with excision of connective tissue and lymph nodes.The pancreas and common duct resection margins and the dissected extrapancreatic nerve plexuses were examined by frozen sections,the results of which determined the extent of the surgical procedure.Resection was made by end-to-side pancreatocojejunostomy,end-to-side hepaticojejunostomy and end-to-side gastrojejunostomy.
The outcomes of both the two groups were retrospectively compared.Comorbidities,preoperative laboratory values,intraoperative variables,pathological diagnosis,and postoperative complications were reviewed.Perioperative mortality was defined as death in hospital or death within 30 days of surgery.The special complications included wound infection,intra-abdominal abscess,bile leak,gastric-jejunal leak,pancreatic leak and fistula formation,urinary tract infection,pneumonia,postoperative myocardial infraction or arrhythmia,and delayed gastric emptying,etc.Pancreatic leak was detected by measuring the ratio of amylase on the first day of feeding.A pancreatic anastomotic leak was defined as a drain amylase level that was at least 3 times of the serum amylase value,and a fistula was defined as a pancreatic leak extending beyond the 14th postoperative day.
The SPSS 11.0 software package was used for statistical analysis.The data were analyzed by Chi-square analysis and Student’s t test when appreciate.P <0.05 was considered significant.
2 Results
Of the 18 patients aged 75 years and over(older group),8 were male(44.4%)and 10 were female(55.6%)with an average age of(77.2 ± 1.5)years.Fifty-four patients(yonger group)were younger than 75 years old with an average age of(63.3 ± 9.7)years.There were 33 males(61.1%)and 21 females(38.9%).
Patient characteristics and preoperative comorbidities were compared as depicted in Table 1.Eleven of the 18 patients(61.1%)75 years of age and over were in a good physical condition,and no comorbidity was demonstrated.In the younger group,comorbidity was not demonstrated in twenty patients(37.0%).There was a greater incidence of pre-existing hypertension in the older group as compared with the younger group.The younger group,however,demonstrated an increased incidence of diabetes mellitus,cardiac valve disease,coronary artery disease,cardiac arrhythmia,chronic renal insufficiency,cerebrovascular disease,and benign disease in hepato-biliary-pancreastic system,and a greater number of patients had co-exist of other neoplasms.None of these differences was statistically significant.No preexisting chronic lung disease was demonstrated in both groups.
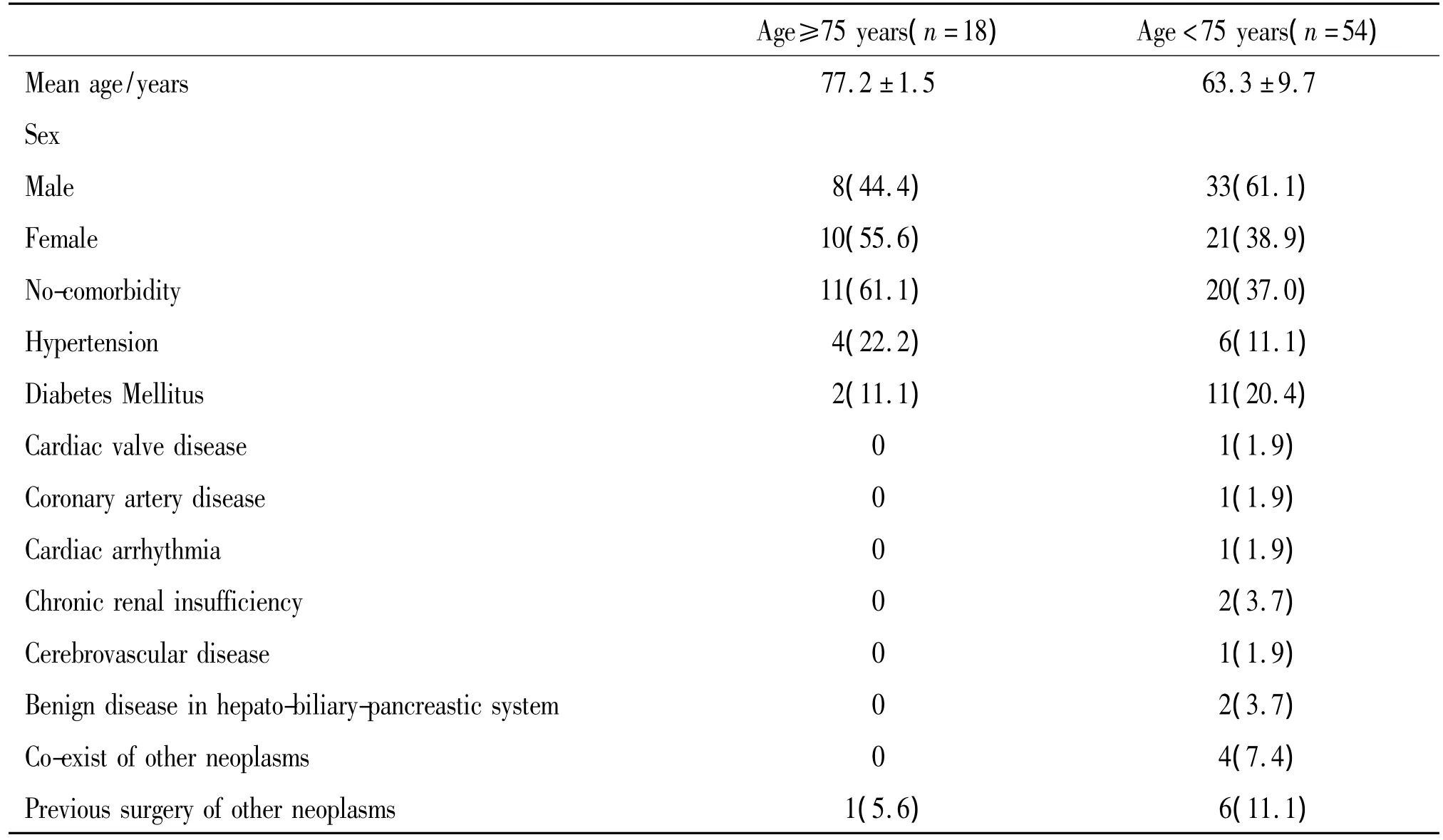
Tab 1 Patient characteristics and preoperative comorbidities
Table 2 summarizes the perioperative variables compared in these patients.The operative time was essentially similar in both groups[(531±36)min vs(545±12)min].The younger group had a higher average estimated operative blood loss of(745±61)ml compared with(656 ±119)ml in the older group,while the difference was not significant.In the younger group,14 patients(25.9%)required fresh frozen plasma(FFP)transfusions with an average of 1.33 units of FFP during the operation,while in the older group,no patient required FFP transfusions,and the difference was significant(P < 0.001).The average intensive care unit(ICU)stay was(1.8 ±1.2)days for patients aged 75 years and over and(2.1 ±1.7)days for patients younger than 75 years old.There was not significant difference.
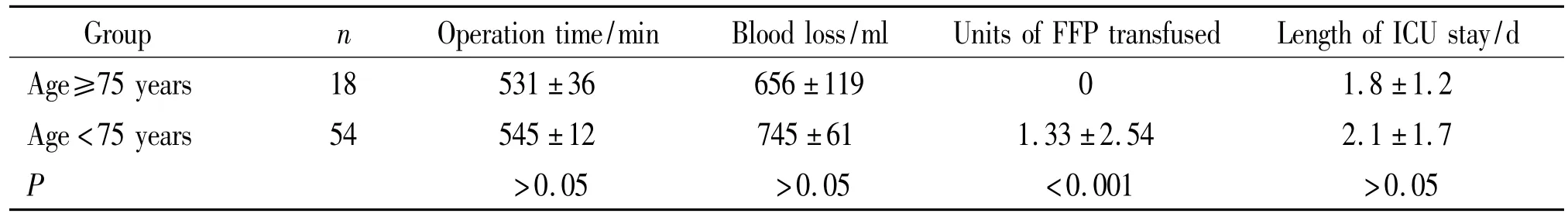
Tab 2 Comparison of intraoperative variables and length of ICU stay
Table 3 shows the comparison of special treatment postoperatively and length of hospital stay between two groups.In the younger group,one patient was treated with tracheotomy postoperatively for the serious pneumonia,while no patients in the older group was treated with tracheotomy.The difference was not significant.Blood dialysis and using of catecholamine were not performed preoperatively in both groups.The period of time from beginning to drinking water and the period of removing the pancreatic tube were slightly different between 2 groups,but the differences were not significant.In the younger group,three patients were re-operated after pancreaticoduodenectomy,two patients for postoperative bleeding and a patient for delayed gastric emptying.No patient in the older group was treated with re-operation postoperatively,and the difference was not significant between 2 groups.The average length of hospital stay in the older group was slightly longer than that of the younger group [(61.1 ± 10.5)d vs(54.3 ± 2.6)d,P >0.05).
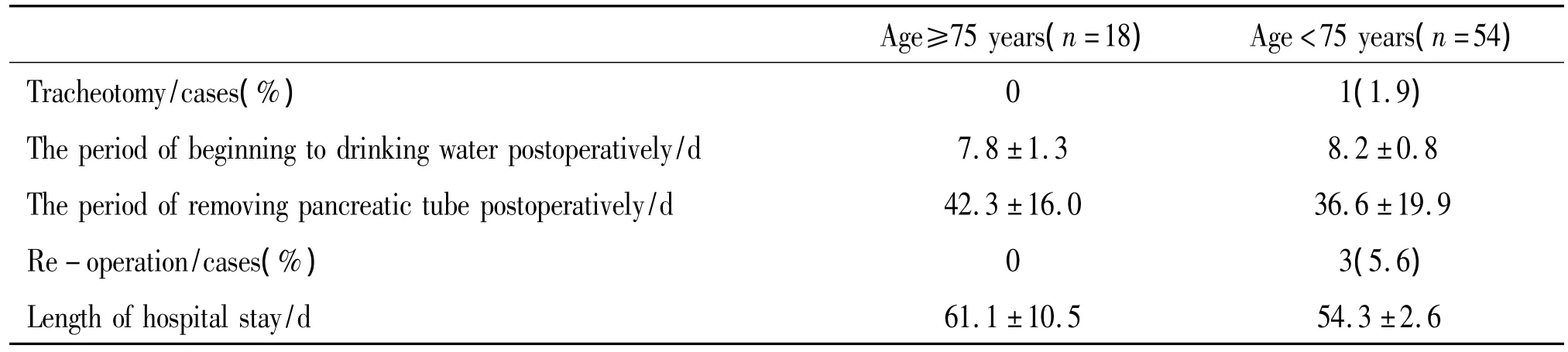
Tab 3 Comparison of special treatment postoperatively and length of hospital stay
Data on perioperative morbidity and mortality are shown in Table 4.With respect to the categories of complications,the difference was not found between the two groups.And there was no difference in the percentage of individuals without postoperative complications(50.0%vs 50.0%,P > 0.05).Wound infection and intra-abdominal abscess were only developed in the younger group.Post-operative bleeding,delayed gastric emptying,and pneumonia were also developed only in the younger group which were treated with re-operation and tracheotomy,respectively.Cardiac complication,bile leak and cholangitis were only developed in the older group.However,no differences were statistically significant.There was a slight increase in the incidence of pancreatic leak and developed pancreatic fistula in the older group.Four patients(22.2%)developed pancreatic leaks after surgery in the older cohort,of whom two(11.1%)were treated as fistulas.Eight patients(14.8%)in the younger group developed postoperative pancreatic leak,of whom one(3.4%)was treated as fistulas.There was no significant difference in the rate of pancreatic leak or fistula formation between the two groups.There were no perioperative death and urinary tract infection in both groups.
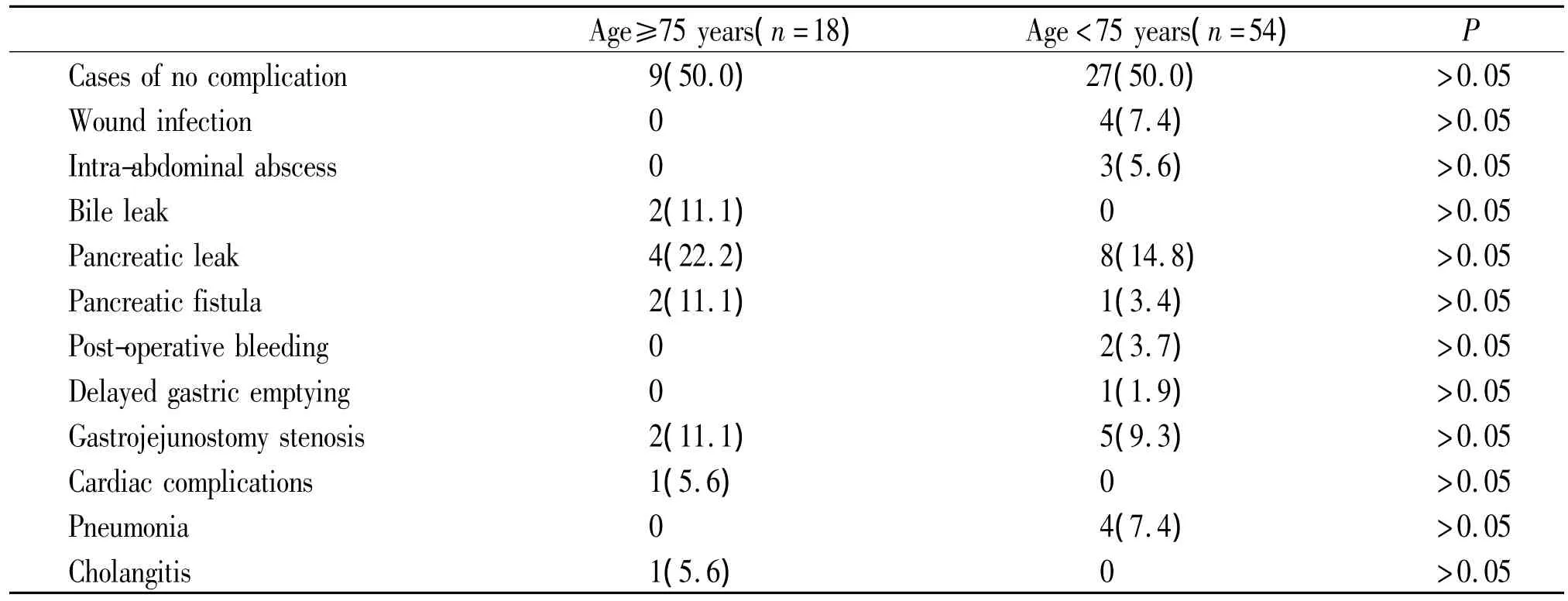
Tab 4 Comparison of postoperative morbidity cases(%)
Table 5 summarizes the postoperative pathological diagnosis of the two groups.Of the 18 pancreaticoduodenal resection performed in the older group,17(94.4%)were for malignant disease and 1(5.6%)was for benign disease.Ten(55.6%)were for distal bile duct adenocarcinoma,five(27.7%)were for pancreatic adenocarcinoma,two(11.1%)were for ampullary adenocarcinoma,and one(5.6%)was for intraductal papillary mucinous adenoma(IPMA)of the pancreas.Significant difference in diagnosis was made in comparing the incidence of distal bile duct adenocarcinoma between the older group and the younger group(P=0.021).In the younger group,47(87.0%)were for malignant diseases.Sixteen(29.7%)were diagnosed as pancreatic adenocarcinoma,fourteen(25.9%)with bile duct adenocarcinoma,twelve(22.2%)with ampullary adenocarcinoma,four(7.4%)with intraductal papillary mucinous carcinoma(IPMC)of the pancreas,and one(1.9%)with a gastrointestinal stromal tumor(GIST).Of the seven patients who were operated for benign diseases,three(5.6%)had chronic pancreatitis and four(7.4%)had intraductal papillary mucinous adenoma(IPMA)of the pancreas.
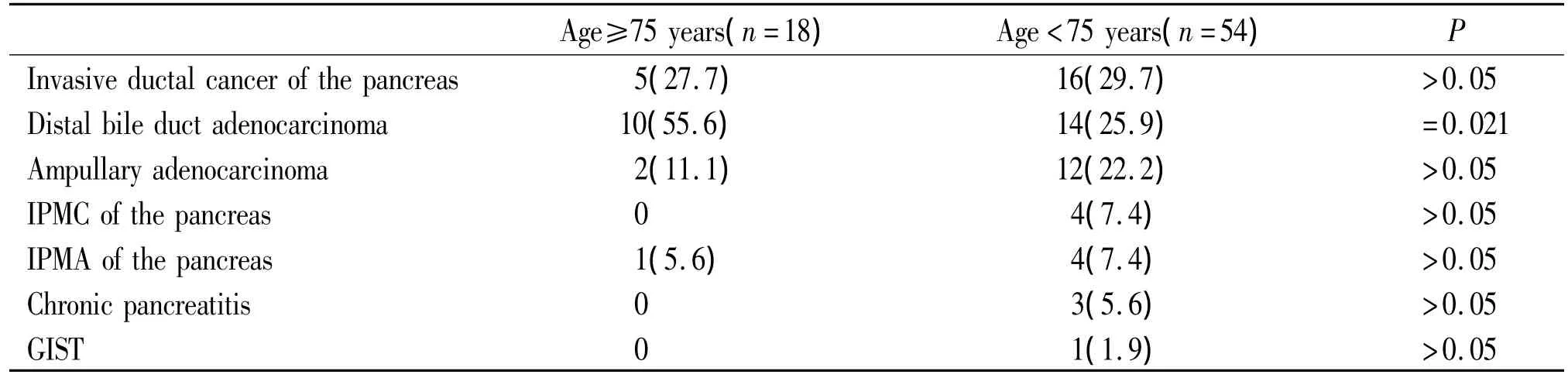
Tab 5 Comparison of pathological diagnosis between 2 groups cases(%)
3 Discussion
The populations of many developed countries are aging,and the incidence of periampullary cancers is increasing.In patients with untreated periampullary cancer the average survival time is 6 months.Age is considered to be a major risk factor for the development of pancreatic adenocarcinoma.About three-quarters of the patients with pancreatic adenocarcinoma are 60 years of age or over[14].It is therefore likely that more patients with periampullary cancer will be evaluated for surgical intervention,including patients of advanced age.In the past,advanced age was considered a major factor associated with perioperative morality after pancreaticoduodenectomy[15-19].Furthermore,Forrest and Longermire in a study of 279 patients concluded that there seems to be no justification for performing this major operation in patients over age 70 in preference to a simple bypass,because no improvement in prognosis or longevity occurred after resection[19].Due to this,and to a low 5-year survival rate,panceaticoduodenectomy was not recommended for a number of years.
Over the past 10 years,the operative mortality and morbidity in curative procedures had decreased considerably in centers that had continued the operative treatment of periampullary cancer[5-7,12].These studies have reported that a marked decrease in morbidity and mortality associated with pancreaticoduodenectomy with mortality rates of less than 5 percent is the rule rather than the exception,thereby expanding their diagnostic and surgical experience.
Furthermore,several investigations have studied patients with advanced age in relation to morbidity and mortality after pancreaticoduodenectomy.Sohn et al[20]compared their series outcomes of 46 patients 80 years of age and over with those of patients younger than 80 years.They found that patients 80 years of age and over had a shorter median operative time but a longer postoperative length of stay and a higher complication rate when compared with their younger counterparts.Pancreaticoduodenectomy in the older group had a mortality of 4.3 percent when compared with 1.6 percent in the younger group.Therefore,they concluded that pancreaticoduodenectomy can be performed safely in selected patients 80 years of age or over with morbidity and mortality rates approaching those observed in younger patients.Similar results have been reported from other series recently.Hodul et al[21]reported on 122 patients undergoing pancreaticoduodenectomy for periampullary neoplasms,48 of them were 70 years of age or over.There was no operative mortality in the older versus 1.4 percent in those patients younger than 70 years.And the perioperative morbidity was 35 percent in the younger group versus 40 percent in the older group,and there was no significant difference.Cameron et al[7]published a series of 145 consecutive pancreaticoduodenectomies done without mortality.Advanced age was not a factor in predicting either morbidity or mortality in that series.The subgroup of 37 patients who were 70 years of age or over was compared with 108 patients who were 69 years of age and younger,and no significant differences in preoperative risk factors and specific complications were present.The hospital course was similar in the two groups with no difference being seen in the operative time,estimated blood loss,number of FFP transfusions per patient,and the length of hospital stay.
Because of the improved operative experience and low operative morbidity and mortality which may be obtained by pancreaticoduodenectomy,many centers have no upper age limitation for performing pancreaticoduodenectomy[3,5-7,9-13].The patients are effectively relieved of jaundice and pain,and the survival time is prolonged with an improved quality of life compared to nonoperative palliative treatment or bypass operation.
During the recent years,age is also not a limitation for pancreaticoduodenctomy in our department.Both the two oldest patients treated with pancreaticoduodenctomy in our department were 81 years old,and the post-operative courses of these two patients were uneventful.In this study,18(25.0%)patients who were 75 years of age and over were compared with 54(75.0%)patients who were 74 years of age and younger,and no significant differences in preoperative risk factors such as hypertension,diabetes,coronary artery disease,cardiac arrhyth-mia,chronic obstructive pulmonary disease,chronic renal insufficiency,co-exist of other neoplasms were present.The operative time,intraoperative blood loss were not significantly different between two groups.However,the average unit of FFP transfusion was significant higher in younger group than in the older group.Although specific complication rates,including intraabdominal abscess,pancreatic leak,pancreatic fistula formation,post-operative bleeding,delayed gastric emptying,pneumonia,and so on,were not significantly different in the old group in this study,post-operative bleeding,delayed gastric emptying,and pneumonia were developed only in the younger group which were treated with re-operation and tracheotomy,respectively.There was no perioperative death in both the older group and the younger group in this study.The length of ICU stay and hospital stay were similar in the two groups.The similar morbidity rate and no mortality in this study would also support the selection of patients 75 years of age and over for pancreaticoduodenectomy.
Although pancreaticoduodenectomy is performed mainly for periampullary cancer,it is also often performed for periampullary benign disease or some other kinds of malignant disease.In this study,9 patients with intraductal papillary mucinous neoplasm(IPMN)of the pancreas(5 patients with IPMA of the pancreas and 4 patients with IPMC of the pancreas),3 patients with chronic pancreatitis,and one patient with GIST were involved.IPMN of the pancreas,which originates from the pancreatic duct,is considered a borderline malignant tumor with a low tendency for invasion and metastasis,and has a better prognosis than ordinary ductal cell carcinoma of the pancreas[21-28].The five-year survival rate of IPMN has been reported to be 86%when the tumor did not invade into adjacent organs,such as the pancreas or duodenum.If the neoplasm is diagnosed as IPMA,the five-year survival rate has been considered to be 100%.In this study,the average age of patients with IPMN of the pancreas and chronic pancreatitis was(60.6 ±10.7)years,and the oldest patient with IPMA of the pancreas was 79 years old.Therefore,the suggestion that age is not a contraindication will supply a chance of radical treatment for older patients with IPMN of the pancreas and improve the quality of life for older patients with chronic pancretitis.
In conclusion,pancreaticoduodenectomy is indicated as the only chance for cure the patients with resected periampullary cancer.At the same time,it is also one of the choices of patients with IPMN of the pancreas,chronic pancreatitis,and some other kinds of neoplasms.According to the recent conclusions from other researchers and our experience,age alone is not a limiting factor for pancreaticoduodenectomy in patients aged 75 years or over.They can tolerate the operation similarly to younger patients,with the same postoperative morbidity and mortality.In view of the fact that in elder patients with periampullary cancer,incidence rate of bile duct adenocarcinoma is the highest,doctors should pay high attention to the biliary system when elderly population receives health checkup or disease screening.
Reference:
[1] Lillemoe KD,Cameron JL,Yeo CJ,et al.Pancreaticoduodenectomy.Does it have a role in the palliation of pancreatic cancer[J]?Ann Surg,1996,223:718 -725.
[2] Reinders ME,Allema JH,van Gulik TM,et al.Outcome of microscopically nonradical,subtotal pancreaticoduodenectomy(Whipple’s resection)for treatment of pancreatic head tumors[J].World J Surg,1995,19:410 -414.
[3] Malleo G,Marchegiani G,Salvia R,et al.Pancreaticoduodenectomy for pancreatic cancer:The Verona experience[J].Surg Today,2011,41(4):463 -470.
[4] Wang C,Wu H,Xiong J,et al.Pancreaticoduodenectomy with vascular resection for local advanced pancreatic head cancer:a single center retrospective study[J].J Gastrointest Surg,2008,12(12):2183-2190.
[5] Yeo CJ,Sohn TA,Cameron JL,et al.Periampullary adenocarcinoma:analysis of 5-year survivors[J].Ann Surg,1998,227:821 -831.
[6] Todoroki T,Koike N,Morishita Y,et al.Patterns and predictors of failure after curative resections of carcinoma of the ampulla of Vater[J].Ann Surg Oncol,2003,10(10):1176 -1183.
[7] Cameron JL,Pitt HA,Yeo CJ,et al.One hundred and forty-five consecutive pancreaticoduodenectomies without mortality[J].Ann Surg,1993,217:430 -438.
[8] Statistical Research and Training Institute.Statistical Handbook of Japan,Chapter 21:Health and Sanitation[M].Tokyo:MPHPT,2004.
[9] Wade TP,Halaby IA,Stapleton DR,et al.Population-based analysis of treatment of pancreatic cancer and Whipple resection:Department of Defense hospitals,1989 -1994[J].Surgery,1996,120:680-687.
[10] Kairaluoma MI,Kiviniemi H,Stahlberg M.Pancreatic resection for carcinoma of the pancreas and the periampullary region in patients over 70 years of age[J].Br J Surg,1987,74:116 -118.
[11] Kang CM,Kim JY,Choi GH,et al.Pancreaticoduodenectomy of pancreatic ductal adenocarcinoma in the elderly[J].Yonsei Med J,2007,30,48(3):488 -494.
[12] Hannoun L,Christophe M,Ribeiro J,et al.A report of forty-four instances of pancreaticoduodenal resection in patients more than seventy years of age[J].Surg Gynecol Obstet,1993,177:556 -560.
[13] Fong Y,Blumgart LH,Fortner JG,et al.Pancreatic or liver resection for malignancy is safe and effective for the elderly[J].Ann Surg,1995,222:426 -437.
[14] Lillemoe KD.Pancreatic and periampullary carcinoma in the eldly[J].Probl Gen Surg,1997,13:108 -120.
[15] Lerut JP,Gianello PR,Otte JB,et al.Pancreaticoduodenal resection.Surgical experience and evaluation of risk factors in 103 patients[J].Ann Surg,1984,199:432 -437.
[16] Obertop H,Bruining HA,Schattenkerk ME,et al.Operative approach to cancer of the head of the pancreas and the peri-ampullary region[J].Br J Surg,1982,69:573 -576.
[17] Onoyama H,Ajiki T,Takada M,et al.Does radical resection improve the survival in patients with carcinoma of the gallbladder who are 75 years old and older[J]?World J Surg,2002,26(11):1315-1318.
[18] Cohen JR,Kuchta N,Geller N,et al.Pancreaticoduodenectomy.A 40-year experience[J].Ann Surg,1982,195:608 -617.
[19] Forrest JF,Longmire WP.Carcinoma of the pancreas and periampullary region[J].Ann Surg,1979,189:129 -138.
[20] Sohn TA,Yeo CJ,Cameron JL,et al.Should pancreaticoduodenectomy be performed in octogenarians[J]?J Gastrointest Surg,1998,2:207 -216.
[21] Hodul P,Tansey J,Golts E,et al.Age is not a contraindication to pancreaticoduodenectomy[J].Am Surg,2001,67:270 -276.
[22] Nishihara K,Fukuda T,Tsuneyoshi M,et al.Intraductal papillary neoplasm of the pancreas[J].Cancer,1993,72:689 -696.
[23] Kimura W,Sasahira N,Yoshikawa T,et al.Duct-ectatic type of mucin producing tumor of the pancreas-new concept of pancreatic neoplasia[J].Hepatogastroenterology,1996,43:692 -709.
[24] Kimura W,Nagai H,Kuroda A,et al.Analysis of small cystic lesions of the pancreas[J].Int J Pancreatol,1995,18:197 -206.
[25] Rivera JA,Castillo CF,Pins M,et al.Pancreatic mucinous ductal ectasia and intraductal papillary neoplasms:a single malignant clinicopathologic entity[J].Ann Surg,1997,225:637 -646.
[26] Siech M,Tripp K,Schmidt-Rohlfing B,et al.Intraductal papillary mucinous tumor of pancreas[J].Am J Surg,1999,177:117 -120.
[27] Kimura W,Kuroda A,Makuuchi M.Problems in the diagnosis and treatment of a so-called mucin-producing tumor of the pancreas[J].Pancreas,1998,16:363 -369.
[28] Kimura W,Makuuchi M,Kuroda A.Characteristics and treatment of mucin-producing tumor of the pancreas[J].Hepatogastroenterology,1998,45:2001 -2008.
