Effect of Biostimble Therapy on Gastrointestinal Function Recovery after Gynecological Surgery
2022-03-23WenMingCaoNaYuPeiPeiZhangXinXinZhouJunQiZhaoKuiMeiZhangXiuRongWangYanLingLi
Wen-Ming Cao,Na Yu,Pei-Pei Zhang*,Xin-Xin Zhou,Jun-Qi Zhao,Kui-Mei Zhang,Xiu-Rong Wang,Yan-Ling Li
1Changle County People's Hospital,Shandong Province,China.
2Shandong Provincial Third Hospital,Shandong,China.
3Pingan Hospital,Longhua District,Shenzhen,China.
Abstract
Keywords: Biostimble therapeutic instrument, Electrical stimulation, Zu San Li acupoints,Gastrointestinal dysfunction
Introduction
Postoperative gastrointestinal dysfunction is a common complication after abdominal surgery. Postoperative patients have symptoms of discomfort, such as nausea, vomiting, anorexia, abdominal pain,abdominal distension, and difficult defecation [1]. Patients not only endure the pain caused by surgery but also experience the discomfort caused by complications. Patients are prone to negative emotions such as depression and anxiety, which affect their postoperative recovery.
Enhanced recovery after surgery (ERAS) is a combination of evidence-based measures to optimize perioperative management. The implementation of the concept of accelerated recovery surgery in gynecologic oncology patients is conducive to shorter hospital stays,lower overall healthcare costs, and increased patient satisfaction[2-3]. Several different ERAS interventions have been used to manage bowel function, including adequate pain control, prokinetic drugs,coffee consumption, gum chewing, early ambulation, and early oral feeding and supportive strategies [4].
对当下护理专业本科生职业认同度相关问题进行问卷调查,根据调查结果分析总结出护理本科生对待护理专业的心理特点及影响因素,并对专业认同度较低的学生进行个案访谈,分别采取不同的对策进行心理指导,帮助其树立正确的职业观,增强护理本科生的职业认同感。
Based on Chinese medicine meridian doctrine, low-frequency pulsed electrophysiological technology was used to stimulate the Zu San Li acupoints to reduce postoperative abdominal pain and bloating and restore bowel sounds. This method is simple and economical to operate, painless to patients, and highly reproducible. There are no reports related to low-frequency pulsed electrophysiological techniques to alleviate postoperative abdominal pain and distension at home or abroad, which is an original and innovative scientific research.
The purpose of this study was to evaluate the safety and efficacy of bioelectrical stimulation technology on postoperative recovery of gastrointestinal function for patients receiving gynecological surgery,which could provide new evidence for promoting rehabilitation after gynecological surgery.
Methods
Participants
Women patients with diagnosed uterine fibroids, aged 40 to 70 years,undergoing elective gynecological surgery were enrolled in this study at the gynecology department of Changle County People's Hospital between March 2021 and December 2021. Twenty patients underwent total transabdominal hysterectomy; twenty patients underwent a laparoscopic hysterectomy, and twenty patients underwent a transvaginal hysterectomy. There were 10 cases of laparoscopic myomectomy and 10 cases of open myomectomy. Inclusion criteria were gynecologic surgery patients aged 40-70 years who have no serious intraoperative or postoperative complications. Patients were excluded if they had neurological, psychiatric disorders, a known history of gastrointestinal disease, and electrode patch allergy.Patients' ages, heights, weights, conditions, medical histories were recorded. The adhesion criteria were scored according to the patient's pelvic adhesions during the procedure (Table 1). Postoperative symptoms and signs of patients were recorded in detail. All postoperative patients were closely observed, and detailed records of adverse reactions were recorded. All patients signed an informed consent form. This study was approved by Changle County People's Hospital ethics committee, Shandong Province, China (ethics number:20210322).

Table 1 Scoring criteria for pelvic adhesions
Postoperative treatment measures
All patients in both the experimental and control groups were given postoperative gynecological postoperative care routine, diet abstinence for 6 hours, fluid and potassium supplementation, and prophylactic application of antibiotics for 24 hours. Except for general postoperative treatment, the patients in the experimental group received acupoint electrical stimulation treatment. The electrode pads connecting the Biostimble therapeutic instrument were arranged at the location of the bilateral Zu San Li acupoints (Figure 1). Zu San Li acupoint is located on the anterolateral side of the lower leg, three inches below the calvarium, with one cross finger from the anterior tibial crest. The DD procedures of the Biostimble therapeutic instrument were selected. The pulse current frequency was 50 Hz.Pulse width adjusted to 200 Us. The treatment was given twice a day for 30 minutes each time.

Figure 1 Zu San Li acupoints
Instrumentation
Biostimble treatment instrument was purchased from Foshan Sansan Datang Medical Technology Co., Ltd.. The registration certificate number is Guangdong arm note permit 20182260716 (Figure 2).

Figure 2 Biostimble treatment instrument
Clinical Observation
Postoperative bowel sounds recovery time.Six hours after the operation, the observer began to listen to bowel sounds with a stethoscope, fully auscultate the four areas of the abdominal umbilical cord (upper left, lower left, lower right, and upper right, 1 minute/time per area), and auscultate once every two hours. If the observer heard the first bowel sound, it was changed to auscultate once every four hours. If the bowel sound returned to normal, it was changed to record once every morning until discharge. Bowel sound≥3 times/min indicates that bowel sounds return to normal. The recovery time of bowel sounds was determined as the time from the end of gynecological surgery to the recovery of bowel sounds.
First postoperative exhaust time.The patient was told to record the specific time of the first anal exhaust and report to the observer. The first anal exhaust time is the time from the end of the operation to the first anal exhaust.
Postoperative symptom score.Postoperative symptoms and signs of patients were evaluated six times daily by an evaluator who was blinded to the study allocation. The main assessment items include lower abdominal distension and pain, nausea and vomiting, degree of fever. The scoring criteria are shown in Table 2-4. Scoring criteria for lower abdominal pain refers to the literature and are revised according to clinical (Table 2). Scoring criteria for nausea and vomiting refers to the criteria recommended by the European Conference on Clinical Oncology 2017 (Table 3). The body temperature is measured with an oral electric thermometer and scoring criteria see table 4.

Table 3 Scoring criteria for nausea and vomiting

Table 4 Scoring criteria for body temperature
Treatment outcomes.The treatment outcomes were classified as“Complete recovery,” “Significant improvement”. “Complete recovery” referred to completely restored gastrointestinal function including bowel sound ≥ 3 times/min, smooth anal exhaust, no nausea and vomiting, no abdominal pain, and abdominal distension 72 hours after surgery. “Significant Improvement” referred to bowel sound ≥3 times/min, anal exhaust, exhaust accompanied by slight abdominal pain, and abdominal distension 72 hours after surgery.
Safety observation.Preoperative blood routine, urine routine, stool routine, coagulation function, liver and kidney function, electrolytes,electrocardiogram, chest X-ray were performed, and laboratory tests such as blood routine, urine routine, liver and kidney function,electrolytes were performed within three days after surgery.
Data entry and data analysis
An entry clerk and a data supervisor jointly operated the data entry to avoid data entry errors. All data were managed and analyzed by the SPSS 22.0 statistical package. Measures data were expressed as the mean±standard deviation, paired t-tests were used before and after medication administration, and analysis was performed by variable transformation or nonparametric statistics when variance was not equal. The chi-square test was used for comparisons between groups of count data, and the Ridit test was used for comparisons of rank data.
Results
Table 2 displays participants’ baseline characteristics. The mean age of participants was 57.5±6.28 years in the experimental group. There were 10 cases of total transabdominal hysterectomy, 10 cases of laparoscopichysterectomy,10 patientswithtransvaginal hysterectomy, 5 cases with Laparoscopic myomectomy, and 5 cases with open myomectomy in the experimental group. Patients in the control group were aged 47-69 years (mean 58.4±7.25). There were 10 cases of total transabdominal hysterectomy, 10 cases of laparoscopichysterectomy,10 patientswithtransvaginal hysterectomy, 5 cases with Laparoscopic myomectomy, and 5 cases with open myomectomy in the control group. There was no significant difference in age, BMI between the patients in the experimental group and the control group (All P > 0.05). There was no significant difference between the experimental group and the control group patients in underlying disease, surgical procedure, anesthesia technique, anesthesia time, operative time, estimated blood loss,blood transfusion (Table 5).

Table 5 Baseline characteristics of the enrolled patients
Comparison of main efficacy indicators
The recovery time of postoperative bowel sounds in the experimental group was 22.66±4.31 hours, and the time of first anal venting was 29.79±3.56 hours, while the recovery time of postoperative bowel sounds in the control group was 28.01±4.22 hours, and the time of first anal venting was 36.24 ± 3.43 hours. The recovery time of postoperative bowel sounds and the time of first anal venting were shorter in the experimental group than that in the control group (All P<0.001, Table 6).
The duration of abdominal distension was 23.79±5.12 hours, and the duration of abdominal pain was 30.15 ± 4.24 hours in the experimental group. While the duration of abdominal distension was 29.07±5.06 hours, and the duration of abdominal pain was 37.17±5.24 hours in the control group. There was a significant difference between the two groups (All P <0.001). There was no statistical difference between the two groups regarding postoperative symptoms scores at the 24-hour after an operation. The mean postoperative symptoms scores in the experimental group (1.17±1.03) were lower than that in the control group (2.08±1.71) at the 72-hour after the operation (P=0.005). In the experimental group, there were 23 cases of complete recovery, 17 cases of improvement. In the control group,there were 12 cases of complete recovery, 28 cases of improvement.The difference in treatment outcome between the experimental and controls was statistically significant (P=0.013, Table 7).
Adverse reaction monitoring
Two patients in the experimental group developed allergies to the electrode patch of the therapeutic instrument, and their condition improved after the topical application of anti-allergy drugs. No other significant side effects were observed during treatment in either group.
Discussion
In gynecological surgery, the causes of gastrointestinal dysfunction include electrolyte disorders, anesthesia, and surgery. Patients with gastrointestinal dysfunction may have abdominal pain, abdominal distension, difficulty venting, difficulty in defecation and other discomforts after surgery. Severe gastrointestinal dysfunction may not only elevate the diaphragm and thus affect respiratory function but also compress the inferior vena cava and affect blood return, thus affecting the healing rate of the incision. Therefore, it is clinically important to quickly improve abdominal distension and pain after surgery, shorten the time of exhaustion and recovery of gastrointestinal function, reduce patients' pain, promote their postoperative recovery, and prevent the occurrence of adverse complications. The traditional treatment for postoperative abdominal pain and distension in gynecology is gastrointestinal decompression and oral administration of gastrointestinal function agonists or proprietary Chinese medicines that promote gastrointestinal motility,which have certain efficacy. However, the above measures are mostly implemented after the symptoms of abdominal pain and distension appear, and the patients have already suffered great physical pain.
The interpretation of gastrointestinal function in Chinese medicine cannot be fully equated with the structure and function of the stomach and intestines in the anatomical sense of modern medicine. The gastrointestinal function recognized by Chinese medicine mainly covers the common functions of the spleen, stomach, small intestine,large intestine, and other organs. Some scholars believe that surgery causes depletion of qi and blood and damage to the spleen and stomach, resulting in the deficiency of qi and blood, weakness of the spleen and stomach, loss of qi elevation and elevation, loss of spleen and stomach transport, and transformation, weakness of large intestine conduction, and lack of internal qi, resulting in abdominal distension, stool closure, tiredness, shortness of breath, vomiting,abdominal pain [5-8]. According to Chinese medicine, regulating qi,activating blood circulation and removing blood stasisis are the key to treating this disease.

Table 6 Study outcomes
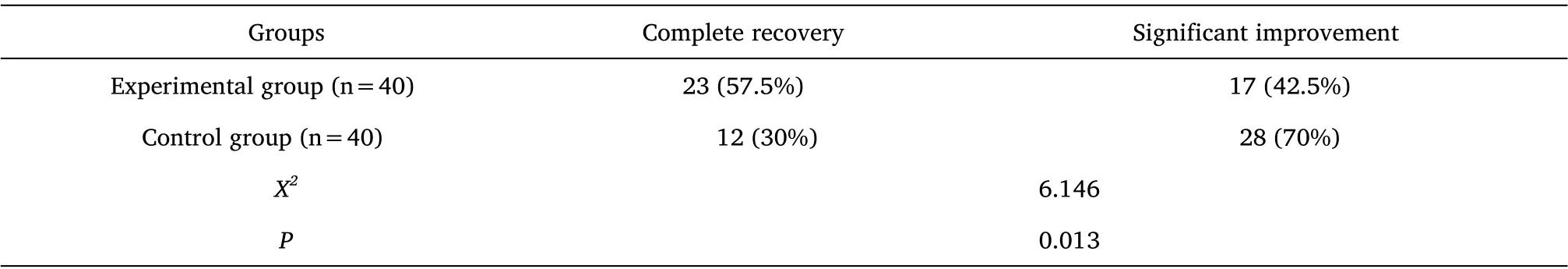
Table 7 Recovery of gastrointestinal function outcomes (n, %)
In reducing gastrointestinal discomfort, a combination of Chinese and Western medicine has been used to achieve good clinical results[9]. Chinese medicine treatment for postoperative gastrointestinal disorders in gynecology includes Chinese herbal soup for internal use,Chinese herbal reserved enema, acupuncture therapy, acupoint massage, acupoint compressing, acupoint injection, auricular point pressure bean, moxibustion, doujinshi, umbilical moxibustion, and buried thread. Preoperative enemas with Qi-regulating and bowel-clearing herbal soup can reduce the incidence of intestinal adhesions, vomiting, and abdominal distension [10]. Oral administration of Li-Qi-Tong-Qi Tang [11-12] is recommended 6-12 hours after surgery to relieve vomiting. In addition, preoperative acupuncture point embedding can prevent gastrointestinal discomfort symptoms [13]. Based on the emotional and mental regulation and Western symptomatic management model, it is recommended to add a warming Chinese herbal incense sac placed on the outside of the patient's nose once every 10 minutes for 1-2 minutes and instruct the patient to inhale deeply to prevent postoperative nausea and vomiting[14]. The rectal application of Kangwomen's anti-inflammatory suppository can effectively promote postoperative intestinal venting and relieve abdominal distension, one capsule each time, twice a day,until the resumption of venting [15] or dissolve the suppository in warm boiled water and take the clear liquid for enema [16].
Biostimble therapy is also known as low-frequency pulse electrophysiology technology. Low-frequency electrical stimulation can improve blood circulation and tissue nutrition, enhance the function of the reticuloendothelial system, and have inherent anti-inflammatory and anti-swelling effects. Stimulating Zu San Li points have the functions of tonifying the middle and benefiting the qi,activating the meridians, regulating the spleen and stomach,supporting the righteousness and eliminating the evil, and removing wind and dampness. Based on the low-frequency pulsed electrophysiological techniques, acting on the Zu San Li acupoints with the modern advanced instruments can reduce postoperative abdominal pain and bloat and restore bowel sounds as soon as possible. However, there are no effect reports related to low-frequency pulsed electrophysiological techniques to alleviate postoperative abdominal pain and distension. The present study found that the application of Biostimble therapy instrument for stimulation of the Zu San Li acupoints could shorten the recovery time of bowel sounds, the time of first anal exhaust, the duration of abdominal distension, and the duration of abdominal pain, which could significantly reduce the symptoms of abdominal pain and distension and nausea and vomiting and promote the patients' recovery as soon as possible. The method is simple and economical to perform, painless to patients. The mechanism of action may be related to the regulation of gastrointestinal fluid secretion, gastrointestinal hormones and blood flow. These findings nevertheless require further validation in an independent cohort.
Conclusion
In conclusion, Biostimble therapy instrument electrostimulation on Zu San Li acupoints can promote rapid recovery of gastrointestinal function in patients after general gynecological surgery.It is a safe and inexpensive and is worth promoting.
猜你喜欢
杂志排行
Psychosomatic Medicine Resesrch的其它文章
- Current Status and Risk Factors of Kinesiophobia in Patients with Temporomandibular Disorders in Tianjin,China:a Cross-Sectional Study
- Screening of Postpartum Depression Diagnostic Markers Based on Immune-Related Genes and Immune Infiltration
- Integrated Behavioral Healthcare in Thailand:A Case Study from Chiang Mai
- Effect of Mindfulness-based Cognitive Training on Sleep Quality and Mindfulness Cognitive Level of College Students
- A Review of Traditional Chinese Medicine for the Treatment of Depression
