The decision for hospice care in patients with terminal illness in Shanghai: A mixed-method study
2022-02-08ChunyanChnXiaobinLaiAipinXuShuanshuanYanJinxianJinHuinYan
Chunyan Chn , Xiaobin Lai , Aipin Xu , Shuanshuan Yan , Jinxian Jin ,Huin Yan
a Department of Nursing, Shanghai Cancer Center of Fudan University, Shanghai, China
b Department of Oncology, Shanghai Cancer Center of Fudan University, Shanghai, China
c School of Nursing, Fudan University, Shanghai, China
d The Community Health Service Center of Chengjiaqiao Road, Shanghai, China
e The Community Health Service Center of Linfen Road, Shanghai, China
f The Hospice Care Center, Yingyuan Hospital, Shanghai, China
g The Community Health Service Center of Jinshanwei Town, Shanghai, China
Keywords:Hospice care Decision making Family Social media
ABSTRACT Objectives: To investigate why patients with terminal illness and their families in Shanghai choose the hospice ward and their decision-making process.Methods: This was a mixed-method study consisting of a cross-sectional survey and a descriptive qualitative study.Medical decision-makers for patients hospitalized in hospice wards were recruited between September 2019 and July 2021.A medical decision-maker is a family member who makes medical decisions for a patient.All 146 participants completed a self-developed 10-item questionnaire that included five items about their demographic characteristics and five items about the decision-making process.The semistructured interviews were conducted with nine participants to understand the family’s decision-making process when they chose a hospice ward.The interviews were analyzed using qualitative content analysis.Results: The mean age of the 146 participants was 57.6 years old.Of the decision-makers,56.85%were the patients’children.Family-dominated discussions involving other family members were the main decisionmaking mode (84.93%).Patient participation in the decision-making process was reported in 43.15% of families.The participation of doctors(17.81%)and nurses(2.05%)were reported in a small number of families.The most common reason for choosing the hospice ward was the inability to find any other hospital for the patients(82.19%).The most commonways to learn about the service were neighbors and friends(38.36%)and social media (28.77%).Two themes and six categories emerged from the interviews.The first theme was reasons for choosing hospice wards.The reasons included being unable to care for the patients at home,stayinginahospicewardcouldreducethepsychologicalstress forhomecare,beingunabletobeadmittedinto tertiary/secondary hospitals, and thinking a hospice ward was a suitable place for the family.The second themewasthe decisionprocess of choosing a hospiceward.Thistheme included the followingtwo categories,i.e.,ways to learn about the hospice ward and family-discussion decision mode.Conclusion: To most families having dying patients, a hospice ward is a reasonable and balanced choice after the families experience huge care stress and practical difficulties.The participation of patients should be encouraged in the family discussion so that their wishes can be known.More efforts will be needed to guide the families with dying patients to make reasonable medical choices.Social media can be a good way to improve public awareness of hospice services in the future.Meanwhile, healthcare providers should be more involved in the decision-making process.
What is known?
· The utilization of hospice services in Shanghai is not satisfactory.
· The choice of patients and their families is one of the main reasons for accepting or rejecting hospice care.
· A few studies have explored end-of-life decision-making in the Mainland of China.
What is new?
· A hospice ward is a reasonable and balanced choice for most families having dying patients after the families experience the caring stress and practical difficulties.
· Patient participation in the decision-making process should be encouraged in the future.
· Social media is a good way to improve public awareness of hospice services.At the same time,healthcare providers should be more involved in the decision-making process to guide the families to make a reasonable medical decision at the end-of-life stage.
1.Introduction
Hospice care has developed rapidly in the Mainland of China over the last decade.Since 2017,71 cities have become pilot areas of hospice care to establish a localized hospice care system that fits the sociocultural context of the Mainland of China.Shanghai was one of the earliest pilots.Two hundred forty-seven community health service centers in the city have provided hospice care in three modes: outpatient hospice services, inpatient hospice services, and home services [1].Inpatient hospice care is the main mode of care for patients with a two-month life expectancy.Thus,dying patients could spend their last days there.
Despite the widely distributed hospice services in the city,their utilization is not satisfactory.In 2018, at least 69,100 patients in Shanghai needed hospice care.However, only 9,700 patients used the service [2].A recent local study reported that the utilization rates of hospice beds in 10 of the 16 districts were higher than 50%.The lowest utilization rate among the 16 districts was less than 20%[2]; in Shanghai, this rate was lower than the rate in areas where hospice services were well-developed.In the United States,approximately 50%of Medicare decedents receive hospice care[3],while another study reported that hospice service utilization in a metropolitan area in the United Kingdom was 64.6%[4].Shih et al.reported that 55.3%of cancer patients received hospice services in a tertiary hospice in Taipei, China [5].
Multiple factors could influence the use of hospice services.The choice of patients and their families is one of the main reasons for accepting or rejecting hospice care[6-9].The reason why patients with terminal illness and their family members accept hospice care needs to be investigated.Overseas studies found that some factors,including the patient’s age,gender,educational background,health status,family's perception of patient’s health,life and death value,family’s care burden, economic status, and living conditions, may affect their choice [6-8].A few studies on a similar topic were conducted on the Chinese population[9-12].Wang et al.reported the choice of resuscitation at the terminal stage by family members in Beijing [9].Another qualitative study conducted in Shanghai interviewed 12 decision-makers of patients with advanced cancer and summarized the factors associated with their decision on palliative care [10].The other studies mainly focused on terminal resuscitation [11,12].These studies began to explore end-of-life decision-making in the Mainland of China.However, the following research questions still need to be answered with more empirical evidence: What makes the patients and their families choose the hospice service? How do they learn about the service?How is the option of hospice service discussed in the family? The answers to these questions could help healthcare providers enhance the use of local hospice care in the future.Hence, this study aimed to investigate the reasons of patients with a terminal illness, and their families chose hospice services in Shanghai and the process of their decision-making on hospice care.
2.Methods
2.1.Study design
This was a mixed-method study with a convergent parallel design.The quantitative part was a cross-sectional survey using a questionnaire to investigate the reasons of the families of dying patients for choosing the hospice service and the process of making that decision.The qualitative part was a descriptive study to explore the families’decision-making process using interviews.The quantitative and the qualitative results could validate each other and deepen the understanding of the studied phenomenon.An integrated conclusion could be drawn based on this solid foundation [13].The study was conducted in the hospice wards of six healthcare service centers in Shanghai.
2.2.Ethical considerations
The ethics application was sent to the ethics committees of the community health service centers involved.The ethics committees deemed that the study could be exempted from the ethics approval because no patients were involved.The study’s objectives and the methods were described to the eligible family members when they were invited to participate.The principles of voluntary participation and confidentiality were emphasized as well.The participants completed the online questionnaire after providing consent.Finally, all participants in the qualitative study signed consent forms before the interviews.
2.3.The quantitative part: the cross-sectional survey
2.3.1.Participants
The inclusion criteria for the participants in the survey were as follows: i) a family member of a dying patient, ii) the patient’s proxy decision-maker, and iii) able to read and communicate in Mandarin.The dying patient was defined as i)diagnosed with a lifethreatening illness, ii) a life expectancy of two months, and iii)hospitalized in a hospice ward of a community health service center in Shanghai.The sample size was calculated based on the number of questionnaire items.The sample size should be 5-10 times the number of items (10 items).Therefore, the sample size was determined to be between 50 and 100.In the early stage of the study, eligible decision-makers were identified by designated healthcare providers in each of the six hospice wards.Then, the decision-makers were introduced to the researcher.The researcher presented the study and invited them to participate.After the COVID-19 outbreak, the designated healthcare providers recruited the participants.
2.3.2.Instruments
A self-designed questionnaire was developed to collect data in the cross-sectional survey.The questionnaire consisted of two parts.The first part consisted of five items to collect the participants’demographic data,such as age,relationship with the patient,educational background, working status, and perception of the patient’s condition.The second part consisted of five items on the family decision-making process,including who was involved in the decision-making discussion, whether the patient was involved in the discussion, the reasons for choosing a hospice ward, ways to learn about the hospice service, and hospitalization frequency within the last three months.Each item comprised a single multiple-choice question.The questionnaire was developed based on previous literature [14,15]and included 10 items.A pilot study was conducted to test if the participants faced any difficulties while completing the questionnaire.Ten family members of the dying patients were invited to the pilot study.The expression of a few items was revised after the pilot study so that the participants could understand the questions without confusion.
2.3.3.Data collection
The data were collected intermittently between September 2019 and July 2021 in the hospice wards of six community health service centers in Shanghai.Three of the community health service centers were located in urban areas.The other three were located in rural areas.Data collection was suspended for a few months when the pandemic situation was serious.Before the COVID-19 outbreak,the questionnaires were collected by the researcher.Following the outbreak, the questionnaires were collected by a designated healthcare provider in each hospice ward because the researchers were not allowed to enter the wards.An online questionnaire was used for data collection.The participant completed the questionnaire using their mobile phone.
2.3.4.Data analysis
The quantitative data collected by the questionnaire were analyzed using the SPSS 20.Descriptive analysis methods were used to present the variables, including means, standard deviations, and frequencies.
2.4.The qualitative part: the descriptive qualitative study
2.4.1.Participants
The inclusion and exclusion criteria for the participants in the qualitative part were the same as those in the quantitative part.The participants were asked if they were interested in an interview to share more about the decision-making process after the questionnaire was finished.The researcher (X.Lai) introduced the qualitative part of the study to the participants in detail.The consent form was signed before the interview was conducted.
2.4.2.Data collection
Initially, the plan was to invite the participants from the six community health service centers for the interviews to expand the variety of participants.Due to the COVID-19 pandemic,participant recruitment and data collection for the second part of the study were halted.Hence, the qualitative study was conducted in one community health service center.Semi-structured interviews were conducted by the second author (X.Lai) in a quiet room in the hospice ward.Nine participants were interviewed from September 2019 to January 2020.An interview guide was developed for the qualitative study.The following questions were asked: i) Would you please share how your family cared for the patient before he/she came to the hospice ward? ii) How did you know about the hospice service in the community?iii)What caused you to make a final decision on the hospice ward? iv) Would you please share more about the decision-making process?How did all of the family members react to the proposal of choosing hospice service? The interviews ranged from 15 to 30 min.Each participant was interviewed once, and all interviews were audio-recorded.
2.4.3.Data analysis
The interviews were transcribed verbatim.The transcripts were imported into NVivo 11 software and analyzed using qualitative content analysis [16].The contents of the interviews were first abstracted and labeled with codes.The codes were then sorted into categories.Finally, themes were created based on the categories.
2.4.4.Rigor
The rigor of the qualitative study was enhanced using the following measures.Researchers with different practice backgrounds (i.e., academic and clinical backgrounds) and specialty backgrounds (i.e., nursing and medicine) were involved in the study to foster the reflexivity of the study.Group discussions were conducted throughout the whole study process.The study was developed after several discussions within the team.During the data analysis, the team members reviewed the data and discussed the findings together until they reached a consensus on the findings to reduce the researcher bias caused by having a single interviewer.During the writing phase, the manuscript’s content was also reviewed and discussed within the team.The quotes in the manuscript were checked to match the findings of the subcategories and categories.
3.Results
3.1.The results of the quantitative part
A total of 146 decision-makers joined the study and completed the questionnaire.Demographic information of the participants is listed in Table 1.The mean age of the participants was 57.6 years(SD= 14.58).More than half of the participants(56.85%) were the patients’ children.Of the participants, 52.05% had studied till vocational school.Only one-third (32.19%) of the participants realized that the patient was at the terminal stage.Although each family had one major decision-maker,following a family discussion instead of alone was very common.Most of families (84.93%)collectively discussed choosing the hospice ward (Table 2).However,the patient’s participation in the decision-making process was reported in 43.15% of families.Doctors and nurses were less frequently involved in the decision-making.17.81%and 2.05%of the participants reported that doctors and nurses joined the decisionmaking process, respectively.The main reason for choosing thehospice ward was that the family could not find any other place for the patient (82.19%), followed by the hospice ward being close to home (64.38%).
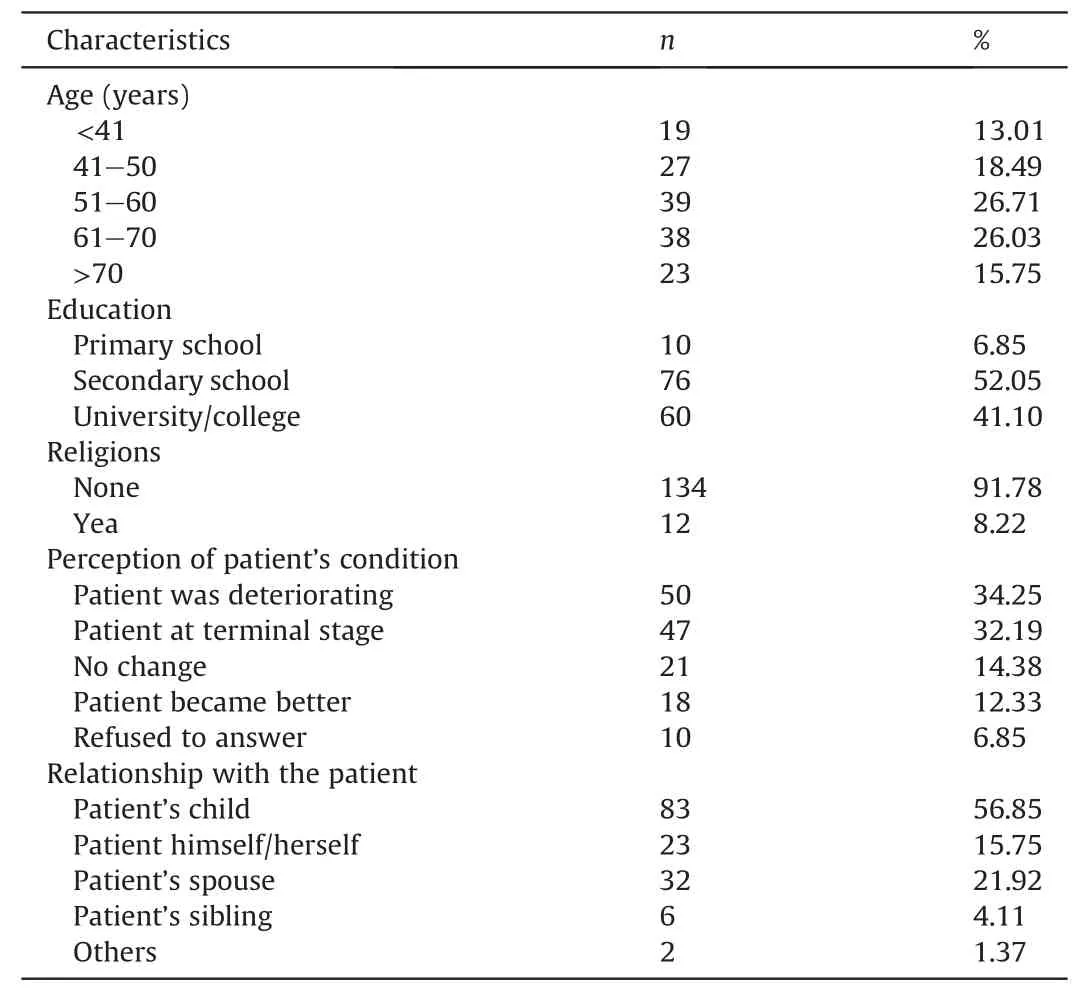
Table 1The demographic characteristics of the participants (n = 146).
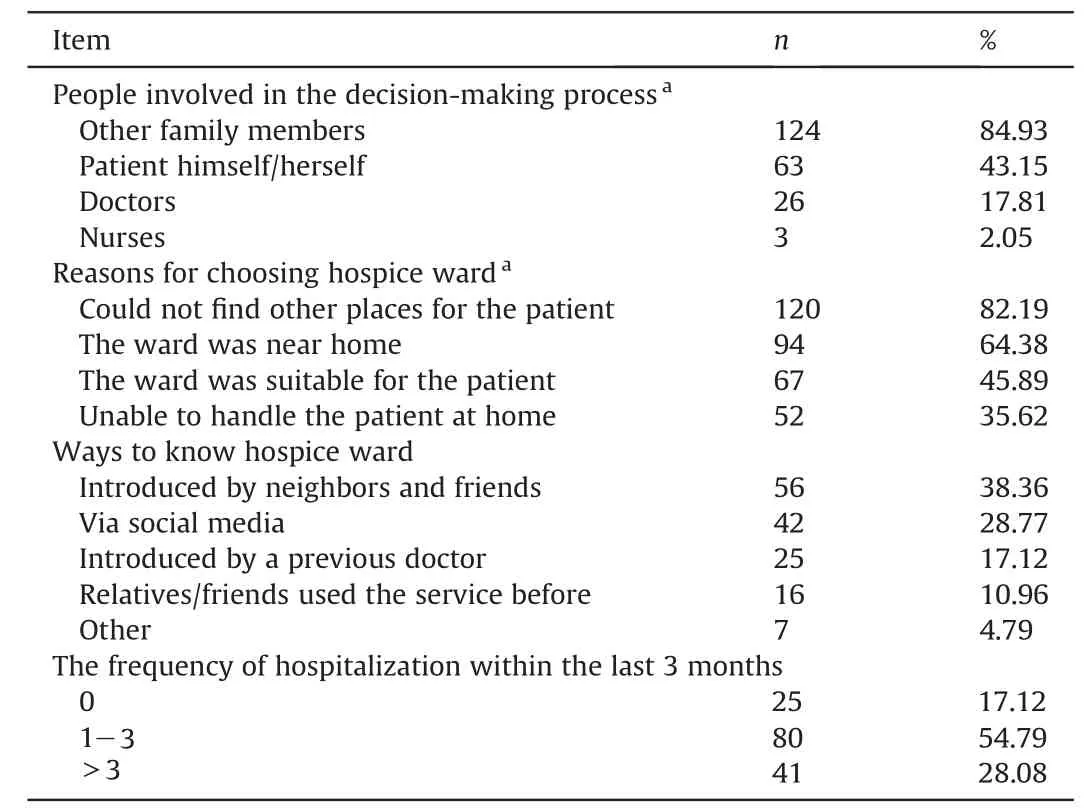
Table 2The decision process of choosing the hospice ward (n = 146).
3.2.The results of the qualitative part
Nine participants were interviewed to understand further how they considered the services and why they ultimately chose the hospice ward.The demographic information of the interviewees is presented in Table 3.Two themes emerged from the interviews:i)reasons for choosing hospice wards and ii) the decision process of choosing a hospice ward(Table 4).

Table 3The information of the interviewees.

Table 4The process of qualitative data analysis.
3.2.1.The reasons for choosing a hospice ward
3.2.1.1.Unable to be cared for at home.The original intention of some families was to send the patient to a hospital to receive care instead of providing it at home.The main reason for giving up home care was that the patients could no longer be cared for at home.In some families,the patient had severe symptoms or conditions that had to be managed medically in a hospital.
“Her [the wife’s]pain was more and more severe.The prescribed pain drug did not work at all.She could not sleep because of the pain.So, we came here, hoping that her problem could be solved.”(No.6)
In other families, family members found that caring for a very sick patient at home was beyond their abilities.Middle-aged family members could not provide prolonged 24-h bedside care.They thought that patients would receive better, professional care in a hospital.
“The patient can be better cared for here(the hospice ward)than at home.There are nurses, doctors, nursing assistants, drugs, and oxygen.But we had nothing at home.”(No.1)
For older carers,physical burnout was the last straw that caused them to cease home care.
“My hand got tenosynovitis because I had to care for my husband all day long.I wanted to continue caring for him at home.However,I had no further strength.So, we sent him here.” (No.7)
3.2.1.2.Reducing the psychological stress of home care.Psychological stress experienced by family members was another reason for choosing hospital care.On the one hand,the participants felt deeply sad and powerless when they witnessed the patient’s suffering but could do nothing.On the other hand, the worry that unexpected accidents might occur at home made them highly nervous.
“He fainted at home several times.I was so scared.After sending him here, I felt more relieved.At least, nurses and doctors are always here.It could be handled promptly if anything happened to him suddenly.”(No.3)
3.2.1.3.Giving up tertiary/secondary hospitals.Physical and mental exhaustion finally prompted the family members to stop home care.According to some participants,a hospice ward was not their first choice.They usually visited a tertiary or secondary hospital.However, the patient could only stay in a tertiary or secondary hospital for 1-2 weeks because of the medical insurance policy.When the patient’s condition was too poor for them to be discharged to home,the patient had to change hospitals after being in the hospital for the allowed number of days.However, the participants experienced finding a tertiary or secondary hospital increasingly difficult with the patient's deterioration.They finally chose a hospice ward realistically after several attempts.
“My husband was lucky to be admitted to a secondary hospital after he lost consciousness.However, I still needed tofind another hospital for him after staying in the secondary hospital for 12 days.I went to the six hospitals near our home one by one,but it was a futile effort.They told me that the hospital beds were all occupied.I almost despaired.Finally, I found this place.They agreed to admit my husband.” (No.1)
3.2.1.4.A suitable place for the family.Only a few participants stated that they intentionally found a hospice ward for the patients because they knew it was suitable.They did not want the patient to receive unnecessary treatment or resuscitation.The type of care provided in the hospice ward was exactly what they wanted.A few participants chose the hospice ward near their home,so visiting the patients was convenient.
“We all know she [the wife]is dying.We believe that the service here is exactly what we want.We just want her last days to be painless and comfortable.” (No.2)
3.2.2.The process of choosing a hospice ward
3.2.2.1.Ways to learn about the hospice ward.The idea of using hospice services was drawn in various ways.A few participants knew about the service before the patient had deteriorated.One participant said that their family knew about the service because the patient was a doctor.Another participant chose the hospice ward because one of his relatives had previously used the service.A few participants remembered that hospice services had been introduced on social media,and then they found the hospice ward nearby.For the other participants, hospice services were mainly suggested by relatives and friends.Only two participants said that doctors in the previous hospitals suggested the hospice ward.
“I did not know about the service before.Later,one of my relatives suggested,‘if you could notfind any other places,you can send the patient here.’” (No.1)
3.2.2.2.Family discussions: the way to make the decision.According to the interviews, all families had discussions or family meetings before making a final decision.For most families,the final decision to choose hospice services was made after struggling psychologically.A participant shared that some of the family members still had different opinions during the discussion.However, after careful consideration,they ultimately agreed to use the hospice.
“Atfirst,some family members still wanted to send the patient to a‘larger’hospital.I acknowledge that a larger hospital has better conditions,but it was too difficult tofind one.Moreover,the patient cannot stay for a long time in such a hospital.Staying home was also impossible.They were unable to share the burden of caring.So,at last, they agreed with my proposal.”(No.1)
Another family finally chose the hospice ward after some hesitation.
“I discussed this idea with my husband several times.I was not willing to send him.I could stay with him all the time at home.He did not wanttocomehere.Stayingathomewasmorecomfortable.ButIcould not care for him at home anymore.He realized that if I continued,I would break down.Finally,we decided to come here.”(No.7)
In the two cases, both the family members and the patients accepted the reality and chose the hospice ward.They realized that this was the most reasonable and balanced choice for both patients and family members.
The discussions were relatively smooth for other families.The participants said that all of their family members clearly understood the patient’s condition and prognosis, so they chose the hospice service without much hesitation.In one family, hospice service was proposed by the patient, and the family decided to respect her choice.
“My wife [the patient]proposed the idea of receiving hospice care.Both my son and I decided to respect her choice.We are psychologically prepared that she will soon die.All we want is for her to be able to die peacefully without pain.Right now, she suffers a lot.” (No.6)
4.Discussion
4.1.A hospice ward is a realistic and balanced choice for the family
In the study,the most common reason for choosing the hospice ward was that the families could not find any other place for the patients.The results were echoed in the decision-makers’ interviews.They believed that the patient could be better cared for in a healthcare institution than at home.They felt safer when the patient was in a hospital.The findings indicate that being cared for in a hospital at the end-of-life stage may be the preferred choice of Chinese families.Previous studies support the conclusion that Chinese families prefer patients receiving care in a healthcare institution instead than at home [10,17].Although some families choose hospice wards because they are suitable for the patients,many still choose hospice wards only because they want them to be cared for in a healthcare institution.
The hospice ward is often the last choice for several reasons.One is the family’s perception of the patient’s condition.Accurate perception of patient prognosis affects the choice of hospice care[18].In this study, only one-third of the decision-makers understood that the patients were dying.According to the interviews,the families who realized that the patients were dying chose the hospice ward deliberately because they thought it was the best choice.Decision-makers who thought that the patient was deteriorating,exhibited no change, or even improved may still try active treatment but not hospice care.
Another reason may be the location of the hospice ward.Chinese families in urban areas usually hold different attitudes toward healthcare institutions at different levels.For example, people living in Shanghai usually choose tertiary or secondary hospitals as their first choice when they need medical help since there are many top-level tertiary and secondary hospitals in Shanghai.The availability of top healthcare institutions means that primary healthcare institutions (i.e., the community health service centers in the city)are less attractive to the public.Hence, community health service centers become their last choice when the tertiary and secondary hospitals are unavailable.Locating a hospice ward in a community health service center undoubtedly will affect people’s willingness to use the service.Meanwhile,the limited drug supply and medical equipment in the community health service centers also contribute to some families avoiding hospice services in the community [19].There seems to be a gap between the patients’ and their families’preferences and hospice service supply.
Many studies have discussed the use of hospice services in Shanghai and the challenges of frontline hospice care providers[2,17,19-23].Previous local studies have demonstrated that the community-based, city-covered hospice services have not been fully functioning[2,19,21,23].Hospice care should be an inseparable part of the whole healthcare system in the city.The communitybased hospice service could benefit dying patients in the long run.The collaboration between the existing community-based hospice service and the secondary and tertiary hospitals must be established.Unfortunately, only a few patients have been transferred from the secondary and tertiary hospitals to the communitybased health service centers [2].Frontline healthcare providers working in the tertiary and secondary hospitals should also be more actively involved so that end-of-life patients who need hospice care can be transferred from the secondary and tertiary hospitals.In addition,could hospice services be delivered in a tertiary or secondary hospital in the future to cater to clients’preferences?How could hospice services be provided in tertiary or secondary hospitals cost-effectively?All these questions are worthy of further discussion.
4.2.Social media and healthcare providers could have more influence to increase hospice service use
Meanwhile, strategies for transferring patients at the terminal stage to hospice wards must be determined to enhance the use of the existing community-based hospice services in the city.Considering that most patients with a late-stage illness can be treated in tertiary or secondary hospitals,a referral system between tertiary and secondary hospitals and hospice wards is needed to enhance the existing hospice services.The referral system is also suggested in several studies[24];however,more work is required.Most families learned about the hospice service through their friends or neighbors or via social media in the survey.Xu et al.also reported that advertising hospice care through social media provides an opportunity for families to choose [10].These findings suggest that strengthening the media propaganda of hospice care could be an effective way to enhance the utilization of hospice services.
Enhancing hospice care use is the job of hospice care providers and healthcare providers who work outside of the hospice care setting and care for patients with life-limiting illnesses.Previous studies found that healthcare providers working outside hospice care settings significantly influence the decision of hospice care[24-29].Whether a healthcare provider communicates with a patient and the family about hospice care is essential in transferring the patient to the hospice service[28].However,in this study,only 17.12% of the decision-makers had learned about the hospice service from their doctors.Only a few doctors and nurses joined the decision-making process of choosing hospice services.The findings indicate that healthcare providers who work outside hospice care settings are lacking during the decision-making process.Lack of knowledge about the existing hospice service may be a reason for not mentioning it to the patients and their families [30].The current study supports this argument, as the option of hospice care was mentioned only by a few doctors.A recent study also reported fewer than half of the doctors working in Shanghai’s community health service centers recommended the hospice service to patients[31].Better communication about end-of-life issues between healthcare providers and patients and their families is needed.
4.3.Nursing implications and limitations
Nurses, especially those who cared for patients with lifethreatening illnesses, could play a more active role in facilitating the family to make a reasonable medical decision when the patient is at the end-of-life stage.Patient education could help the patients and their families better understand the illness prognosis and prepare psychologically for the end of life.In addition,nurses could further discuss end-of-life issues with the patients and their families when the disease deteriorates.Furthermore,local hospice care resources could be introduced to the patients and their families.Meanwhile, nurses could lead family meetings to guide the family planning for the patient at the end-of-life stage.
A few limitations should be considered before generalizing the findings of this study.Due to the COVID-19 pandemic, data collection did not progress as smoothly as expected.The number of patients admitted to hospice wards significantly decreased during the crisis.Family visits were also restricted.Hence, the crosssectional survey and the qualitative interviews sample were smaller than the estimated sample size.However, the multi-site data collection in the urban and rural areas of the city somewhat mitigated the limitation of the small sample size.Another rule was that only patients in hospice wards were researched, while the reasons for patients and their families not to use the hospice service should also be explored.This way, the decision-making process of patients with terminal illnesses concerning hospice services could be better understood.Strategies from different perspectives could be proposed to enhance hospice service use based on comprehensive research of the decision-making process.
5.Conclusion
The families in Shanghai preferred hospitalized care for patients with terminal illnesses.A hospice ward is a realistic and balanced choice for most families.Neighbors,friends,and social media play a positive role in introducing hospice services to families and could continue to do so in the future.Meanwhile, the decision-making process regarding hospice care among Chinese patients and their families must be further explored to develop tailored strategies for hospice service use.
Credit author statement
Chunyan Chen: Conceptualization, Methodology, Formal analysis, Writing-original draft.Xiaobin Lai:Conceptualization, Methodology, Formal analysis, Investigation, Writing-original draft,Supervision.Aiping Xu: Methodology, Investigation, Resources,Writing-review & editing.Shuangshuang Yang: Methodology,Investigation, Resources, Writing-review & editing.Jingxian Jin:Methodology, Investigation, Resources, Writing-review & editing.Huifeng Yang: Methodology, Investigation, Resources, Writingreview &editing.
Funding
This work was funded by the 2020 Original Research Project of Fudan University, Shanghai, China.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of competing interest
The authors have declared no conflict of interest.
Acknowledgements
The authors would like to thank all of the colleagues and friends who helped to approach eligible health care providers.We would also like to thank Editage (www.editage.cn) for English language editing.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.12.002.
杂志排行
International Journal of Nursing Sciences的其它文章
- The development of an evidence-informed Convergent Care Theory:Working together to achieve optimal health outcomes
- The development and implementation of a model to facilitate self-care of the professional nurses caring for critically ill patients
- Self-endangering: A qualitative study on psychological mechanisms underlying nurses’ burnout in long-term care
- Early mobilization implementation for critical ill patients: A crosssectional multi-center survey about knowledge, attitudes, and perceptions of critical care nurses
- Distress management in cancer patients:Guideline adaption based on CAN-IMPLEMENT
- Demand analysis of an intelligent medication administration system for older adults with chronic diseases based on the Kano model
