Emergency bedside ultrasound for the diagnosis of pediatric intussusception: a retrospective review
2014-03-20SamuelLamAdamWiseChristopherYenter
Samuel H. F. Lam, Adam Wise, Christopher Yenter
1Department of Emergency Medicine, Advocate Christ Medical Center, Oak Lawn, Illinois, USA
2Department of Emergency Medicine, University of Illinois at Chicago, Chicago, Illinois, USA
Corresponding Author:Samuel Lam, Email HiufungSamuel.Lam@advocatehealth.com
Emergency bedside ultrasound for the diagnosis of pediatric intussusception: a retrospective review
Samuel H. F. Lam1,2, Adam Wise1, Christopher Yenter1
1Department of Emergency Medicine, Advocate Christ Medical Center, Oak Lawn, Illinois, USA
2Department of Emergency Medicine, University of Illinois at Chicago, Chicago, Illinois, USA
Corresponding Author:Samuel Lam, Email HiufungSamuel.Lam@advocatehealth.com
BACKGROUND:Ultrasound diagnosis of pediatric intussusception is feasible with limited operator training. The authors report the test characteristics of bedside ultrasound (BUS) for the diagnosis of pediatric intussusception at a single institution.
METHODS:Inclusion criteria were: 1) patients of 0–18 years old were seen in the pediatric emergency department (ED) with a clinical presentation suspicious for intussusception; 2) BUS was performed to identify intussusception and bedside impression documented in the medical record; 3) a "formal" diagnostic study (such as computed tomography, ultrasound, or barium enema) was performed by the radiology department after BUS was completed. Electronic medical record and ED BUS archive were screened for potentially eligible ED visits between January 1st2009 to October 3rd2012. These records were then reviewed to identify patients for inclusion in the study. All emergency physicians who performed the BUS had undergone a minimum of 1-hour didactic training on the use of BUS to diagnose pediatric intussusception.
RESULTS:A total of 1 631 charts were reviewed, with 49 meeting inclusion criteria. Five of those were later excluded for incomplete documentation or lack of saved BUS images. The prevalence of intussusception was 23%. The mean age of the subjects was 31 months. BUS was 100% sensitive (95%CI 66%–100%) and 94% speci fi c (95%CI 79%–99%) for detection of pediatric intussusception compared to radiology study results. Positive and negative likelihood ratios were 16.5 (95%CI 4.30%–63.21%) and 0 (95%CI 0–0) respectively.
CONCLUSIONS:BUS is an accurate means of diagnosing acute intussusception in pediatric patients. Further study might be indicated to con fi rm such bene fi ts.
Emergency medicine; Intussusception; Ultrasonography
INTRODUCTION
Intussusception is a condition affecting 2.4 per 1 000 live births in the United States and is the second only to appendicitis as the most common cause of an acute abdominal emergency in children.[1]If left undiagnosed and untreated, it can potentially lead to bowel necrosis and death. The classic triad of colicky abdominal pain, vomiting, and "currant jelly" stool occur in only 30%–40% of cases at presentation.[2]Often patients present with vague symptoms such as crying, abdominal discomfort, or lethargy. The diagnosis of intussusception is complicated by the fact that most of the cases occur in children younger than 2 years, who are unable to provide a clear history. Barium enema is considered the gold standard in diagnosis of intussusception. However it is invasive, exposes children to radiation, and requires the on-site presence of an experienced radiologist, making it impractical in many hospitals during the after-hours.

Figure 1. Classic appearance of intussusception on ultrasound "the doughnut sign".
Ultrasound was fi rst utilized to diagnose intussusception in the 1980s. It has the advantage of being radiation-free and non-invasive. Over the years, it has been proven to be highly sensitive and specific.[3–5]Hence ultrasound has become the fi rst-line diagnostic test for suspected intussusception in many radiology departments throughout the world. As the scanning technique is relatively easy to learn and the pathological pattern ("doughnut sign" shown in Figure 1) quite easy to recognize, it has been found that trainees with as little as 3 months of training in ultrasound can perform the study with similar accuracy as staff radiologists.[6]All these properties make it an ideal tool for the emergency physician with proper training to diagnose intussusception at the bedside.
The purpose of the current study was to measure the test characteristics of emergency physician-performed bedside ultrasound for the diagnosis of pediatric intussusception when compared to radiology department results as a gold standard.
METHODS
This was a single-site retrospective study on children who received bedside ultrasound (BUS) in the Advocate Christ Medical Center Pediatric Emergency Department (ED) for suspected intussusception. It was approved by the Advocate Health Care Institutional Review Board. Our ED is a tertiary pediatric referral center with over 30 000 visits per year, and is staffed by board-certi fi ed emergency physicians around the clock. Ultrasound studies of the radiology department are performed by technicians 24 hours a day, 7 days a week at our hospital. On-site staff radiologists provide interpretation of radiologic studies and perform barium/air enema if needed, with pediatric radiologists available as backups in the after-hours.
Emergency physicians who performed BUS to diagnose pediatric intussusception had undergone a minimum of 1-hour didactic training on the application. A Sonsite M-Turbo machine (Bothell, WA, USA) with pediatric transducers was used to perform the studies. Recorded study images were archived at the ED ultrasound of fi ce. They were reviewed weekly for quality assurance.
The ED compiled its medical record electronically using a web-based system with built-in features allowing for record search by age range, diagnosis, and visit date. In addition, documented procedures such as BUS were also searchable. This electronic medical record database (EMR) was queried for ED visits meeting the following inclusion criteria: (1) Patients 0–18 years old seen in the ED from January 1, 2009 to October 3, 2012; (2) clinical presentation suspicious for intussusception; (3) BUS performed by credentialed emergency physicians in the ED with documented bedside interpretation in the medical record; (4) A formal diagnostic radiology study (such as computed tomography, ultrasound, or barium enema) was obtained during the same ED visit. Cases were excluded if any of the following criteria was present: (1) No formal radiology study obtained during the ED visit to evaluate for intussusception; (2) No BUS images recorded for quality assurance; (3) Undocumented bedside interpretation of BUS performed. A cut-off date of October 3, 2012 was chosen because of the transition of our ED to a new electronic medical record system on that date.
Potential cases for the study were identi fi ed using the following search strategy. Two of the investigators (SL, AW) fi rst queried the EMR looking for "intussusception" or first 4 letters of the word in the ED Final Diagnosis field to identify the "positive" cases. Afterwards, all ED visits within the specified age and time range with a documented BUS impression (on any type of study) were identified to ensure inclusion of the "negative" cases, i.e. patients whose treating clinicians suspected intussusception based on history and physical examination but whose ED workup was negative. As a duplicate measure, the ED BUS archive was reviewed by a third investigator (CY) to identify potentially missed cases. After the screening was complete, the ED record of each potential case was then reviewed for inclusion in the study based on the aforementioned inclusion and exclusion criteria. Particular attention was paid to the time stamps of BUS impressions in the EMR and dictated radiology reports to ensure that former precede the later, to avoid inadvertent bias by physicians performing BUS.
Information extracted from the selected cases included patient demographics, BUS interpretation by emergency physicians, radiology department study results, discrepancy between bedside BUS interpretation and over-reading at weekly quality assurance sessions, and discharge diagnosis. Extracted data were entered into aspreadsheet and analyzed by SPSS version 20.0 (IBM Corp., Armonk, NY, USA). The sensitivity, specificity, positive predictive value, negative predictive value, and overall accuracy of ED BUS studies were calculated using radiology department study results as the gold standard.
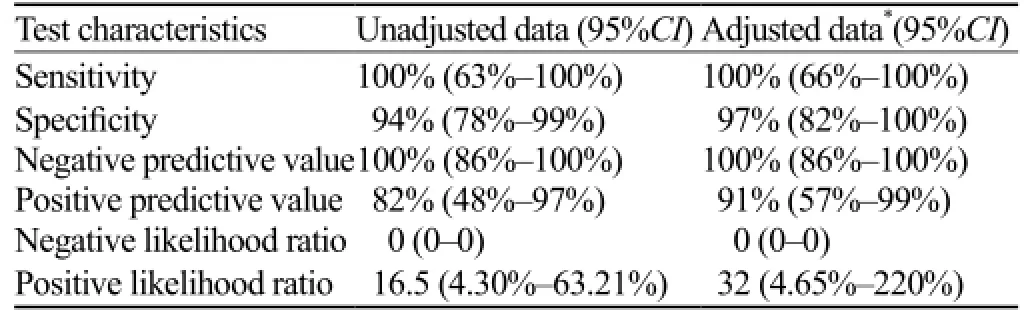
Table 1. Test characteristics of BUS
RESULTS
A total of 1 631 charts were reviewed, with 49 cases meeting the inclusion criteria. Five of those were later excluded for incomplete procedural documentation or lack of saved BUS images. Of the remaining cases, there were 12 BUS studies interpreted as positive for intussusception, and 32 studies negative. Seven physicians performed these BUS studies. The prevalence of intussusception was 23%. Thirty of the 44 patients were male (68%). The mean age of the patients was 31 months. There was no difference in demographic characteristics between the patients with and without intussusception. None of the intussusception cases had a pathological lead point, and all were successfully reduced by barium, air, or gastrograf fi n enema.
There were 2 false positive and no false negative BUS studies. One of the false positives was determined to be transient intussusception after review of the BUS images by the pediatric radiologist. This patient was discharged home after his symptoms spontaneously subsided in the ED and he tolerated oral intake. The other BUS was interpreted as positive for intussusception at the bedside but subsequently over-read as a negative study during image review. He was also discharged from the ED and had no further visit for related complaints. None of the patients with negative BUS was subsequently treated at our institution for intussusception. Calculated test characteristics of BUS in intussusception diagnosis are listed in Table 1. Alternative values were also calculated if the transient intussusception case was considered true positive.
DISCUSSION
Our study demonstrated that physicians with limited training could diagnose pediatric intussusception by ultrasound with a high degree of accuracy. This is consistent with the results of various published studies.[6–8]
With a negative likelihood ratio of 0 and a positive likelihood ratio of over 16, BUS results are likely to be helpful in clinical decision-making in the emergency department. In other words, along with clinical suspicion, treatment decisions might be made based on negative or positive BUS results. This is especially true in cases of medium or low clinical suspicion, or in cases of atypical presentation of intussusception. A review of our con fi rmed intussusception cases revealed that none of these patients presented with the classic triad of colicky abdominal pain, vomiting, and "currant jelly" stool. One patient had intermittent vomiting and abdominal pain for over a week. Another patient was 7 years old at presentation. Some of these patients could have required prolonged and convoluted workups, perhaps even been subjected to unnecessary ionizing radiation before the correct diagnosis was made, had they not had BUS performed. In all of the cases, BUS likely led to timely diagnosis of the patients, and facilitated their workup in the emergency department.
Reports on the use of BUS by emergency physicians to diagnose pediatric intussusception have only begun to appear in the medical literature over the last 5 years.[7–10]Though these study results have been encouraging, a recent review concluded that the value of BUS to rule out intussusception has yet to be proven due to "clinically unacceptable" reported sensitivities, and that further studies would be necessary due to relatively small sample sizes.[11]Our results were similar to the conclusions of the two published trials, in which emergency physicians with focused training could diagnose pediatric intussusception accurately with BUS.[7,8]Although the total number of our cases was less than that of the existing studies, the number of intussusception cases included was compatible. Furthermore, our case series also yielded a better BUS sensitivity. Thus our results may complement the existing literature, and serve as a rebuttal to the aforementioned comment of limited utility of BUS in ruling out intussusception. Because of the relative rarity of intussusception and the paucity of physician sonographers, future studies on the topic may require multi-institutional collaboration in order to accumulate suf fi cient positive cases and achieve adequate power.
Transient intussusception is not an uncommon condition in young children, for which conservative treatment is generally recommended.[12]Hence we feel that our single case of such should really be classi fi ed as a true positive instead of a false positive BUS. Interestingly, one of the false negative cases in Riera's study also seemedto suffer from transient ileocolic intussusception, and reclassifcation of the case would have greatly improved their reported BUS sensitivity.[7]
The major limitation of our study is its retrospective design and the potential for errors and omissions.[13]Despite our efforts to define our inclusion/exclusion criteria as explicitly as possible and to cross-check two different databases, it is possible that some potential cases were inadvertently omitted. Similarly, abstractor bias is likely present in spite of efforts to minimize it, since abstraction was unblinded. False negative rate may be underestimated in our study, as only single institutional data were reviewed, and subjects might have presented to other emergency departments with undetected intussusception or complications. In addition, it is also possible that some BUS studies were not recorded, particularly those that were nondiagnostic or incongruent with radiology department results. Our departmental BUS credentialing policy explicitly states that all BUS studies performed for the purpose of clinical decision-making at the bedside are required to have saved images and bedside impression documented in the chart. To minimize the incentive for under-documentation, BUS images are stored separately from the hospital-wide Picture Archiving and Communication System (PACS), and discrepancy with radiology results are routinely reviewed but not penalized. Historically, noncompliance with the BUS policy has been uncommon among credentialed physicians, and mostly unintentional if they do occur. A review of the 5 excluded cases also did not reveal any obvious discrepancy between the BUS and the radiology department study results. All of our physician sonographers had performed more than 500 studies in various BUS applications, and most of them were emergency ultrasound fellowship-trained or emergency ultrasound fellows at the time of the study. Hence our results may not be typical of less experienced sonographers. Except for the presence of stool, we did not encounter any patient with conditions that might be falsely interpreted as intussusception on BUS such as inflammatory bowel disease, Meckel diverticulum, and appendicitis. Thus the test characteristics might be different in a patient population with more diverse pathology.
In conclusion, from our single-site retrospective review, emergency physician performed BUS was highly sensitive and specific for the diagnosis of pediatric intussusception, and would likely be helpful in clinical decision-making at the bedside. Future prospective study with a larger sample size might be needed to confirm these fi ndings.
Funding:The study was not supported by any funding.
Ethical approval:The study was approved by the Advocate Health Care Institutional Review Board.
Conflicts of interest:The authors have no financial or other con fl icts of interest relevant to the content of this manuscript.
Contributors:Lam S proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
1 Waseem M, Rosenberg HK. Intussusception. Pediatr Emerg Care 2008; 24: 793–800.
2 Bruce J, Huh YS, Cooney DR, Karp MP, Allen JE, Jewett TC Jr. Intussusception: evolution of current management. J Pediatr Gastroenterol Nutr 1987; 6: 663–674.
3 Hryhorczuk AL, Strouse PJ. Validation of US as a firstline diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol 2009; 39: 1075–1079.
4 Bhistkul DM, Listerncik R, Shkolnik A, Donaldson JS, Hendricks BD, Feinstein KA, et al. Clinical application of ultrasonography in the diagnosis of intussusception. J Pediatr 1992; 121: 182–186.
5 Verschelden P, Filiatrault D, Garel L, Grignon A, Perreault G, Boisvert J, et al. Intussusception in children: reliability of US in diagnosis-a prospective study. Radiology 1992; 184: 741–744.
6 Eshed I, Gorenstein A, Serour F, Witzling M. Intussusception in children: can we rely on screening sonography performed by junior residents? Pediatr Radiol 2004; 34: 134–137.
7 Riera A, Hsiao AL, Langhan ML, Goodman TR, Chen L. Diagnosis of intussusception by physician novice sonographers in the emergency department. Ann Emerg Med 2012; 60: 264–268.
8 Zerzan J, Arroyo A, Dickman E, Vazquez V. Diagnosing intussusception by bedside ultrasonography in the pediatric emergency department. Acad Emerg Med 2012; 19 (Suppl 1): S151.
9 Kairam N, Kaiafis C, Shih R. Diagnosis of pediatric intussusception by an emergency physician-performed bedside ultrasound: a case report. Pediatr Emerg Care 2009; 25: 177–180.
10 Halm BM, Boychuk RB, Franke AA. Diagnosis of intussusception using point-of-care ultrasound in the pediatric ED: a case report. Amer J Emerg Med 2011; 29: 354e1–354e3.
11 Raymond-Dufresne E, Ghanayem H. BET 2: Can emergency physicians safely rule in or rule out paediatric intussusception in the emergency department using bedside ultrasound. Emerg Med J 2012; 29: 854–855.
12 Kornecki A, Daneman A, Navarro O, Connolly B, Manson D, Alton DJ. Spontaneous reduction of intussusception: clinical spectrum, management and outcome. Pediatr Radiol 2000; 30: 58–63.
13 Gilbert EH, Lowenstein SR, Koziol-McLain J, Barta Dc, Steiner J. Chart review in emergency medicine research: where are the methods? Ann Emerg Med 1996; 27: 305–308.
Received March 23, 2014
Accepted after revision August 20, 2014
World J Emerg Med 2014;5(4):255–258
10.5847/wjem.j.issn.1920–8642.2014.04.002
杂志排行
World journal of emergency medicine的其它文章
- Current pre-hospital traumatic brain injury management in China
- How to secure the connection between thoracostomy tube and drainage system?
- Clinical probability and risk analysis of patients with suspected pulmonary embolism
- Thyroid hormone alterations in trauma patients requiring massive transfusion: An observational study
- The incidence of oxygen desaturation during rapid sequence induction and intubation
- A single subcutaneous dose of tramadol for mild to moderate musculoskeletal trauma in the emergency department
