Predicting short-term major postoperative complications in intestinal resection for Crohn’s disease: A machine learning-based study
2024-05-07FangTaoWangYinLinXiaoQiYuanRenYuanGaoXiaoCaiWuWeiWeiXuTianQiWuKaiXiaYiRanJiaoLuYinChunQiuChen
Fang-Tao Wang,Yin Lin,Xiao-Qi Yuan,Ren-Yuan Gao,Xiao-Cai Wu,Wei-Wei Xu,Tian-Qi Wu,Kai Xia,Yi-Ran Jiao,Lu Yin,Chun-Qiu Chen
Abstract BACKGROUND Due to the complexity and numerous comorbidities associated with Crohn’s disease (CD),the incidence of postoperative complications is high,significantly impacting the recovery and prognosis of patients.Consequently,additional studies are required to precisely predict short-term major complications following intestinal resection (IR),aiding surgical decision-making and optimizing patient care.AIM To construct novel models based on machine learning (ML) to predict short-term major postoperative complications in patients with CD following IR.METHODS A retrospective analysis was performed on clinical data derived from a patient cohort that underwent IR for CD from January 2017 to December 2022.The study participants were randomly allocated to either a training cohort or a validation cohort.The logistic regression and random forest (RF) were applied to construct models in the training cohort,with model discrimination evaluated using the area under the curves (AUC).The validation cohort assessed the performance of the constructed models.RESULTS Out of the 259 patients encompassed in the study,5.0% encountered major postoperative complications (Clavien-Dindo ≥ III) within 30 d following IR for CD.The AUC for the logistic model was 0.916,significantly lower than the AUC of 0.965 for the RF model.The logistic model incorporated a preoperative CD activity index (CDAI) of ≥ 220,a diminished preoperative serum albumin level,conversion to laparotomy surgery,and an extended operation time.A nomogram for the logistic model was plotted.Except for the surgical approach,the other three variables ranked among the top four important variables in the novel ML model.CONCLUSION Both the nomogram and RF exhibited good performance in predicting short-term major postoperative complications in patients with CD,with the RF model showing more superiority.A preoperative CDAI of ≥ 220,a diminished preoperative serum albumin level,and an extended operation time might be the most crucial variables.The findings of this study can assist clinicians in identifying patients at a higher risk for complications and offering personalized perioperative management to enhance patient outcomes.
Key Words: Crohn’s disease;Postoperative complications;Nomogram;Random forest;Ⅰntestinal resection
lNTRODUCTlON
Inflammatory bowel disease (IBD) exhibits a high incidence and prevalence in Western developed countries,being a more common gastrointestinal disease in Europe and North America.Since the beginning of the 21stcentury,the incidence of IBD in European and American countries has gradually stabilized,while in non-Western countries,particularly in Asia,South America,and Eastern and Southern Europe,the incidence of IBD has exhibited an upward trend[1,2].In China,the number of IBD cases has demonstrated a substantial growth trend over the past two decades[3].Particularly in densely populated developed cities,the incidence of Crohn’s disease (CD) has increased significantly,ranging from 0.07/100000 to 1.27/100000[4].
Despite advances in medical therapy,70% to 90% of patients with CD necessitate surgery in their lifetime[5],and postoperative complications are prevalent[6].Special attention should be directed towards major postoperative complications,including intra-abdominal sepsis complications (IASC),bleeding,anastomotic fistula,and intestinal obstruction.Such complications can result in prolonged hospital stays,heightened healthcare costs,and adverse patient outcomes[7].Identifying risk factors for these complications is crucial for optimizing the care of patients with CD undergoing surgery.
Several studies have explored the risk factors for postoperative complications in patients with CD,yet the results have been inconsistent,frequently constrained by heterogeneous patient populations.Additionally,these studies encompass a relatively broad inclusion period,during which medical therapy and management approaches have been enhanced[8-10].Furthermore,the mesentery in patients with CD tends to undergo thickening,significantly elevating the risk of intraoperative and postoperative bleeding.Nevertheless,the majority of prior studies examining the risk factors for postoperative complications concentrated solely on anastomotic fistula and IASC,neglecting postoperative bleeding[11-14].Furthermore,prior studies on the factors influencing postoperative complications in patients with CD were exclusively grounded in traditional regression models and did not employ advanced machine learning (ML) models.In recent years,ML technologies have gained widespread application in the field of intelligent healthcare,bearing significant practical and societal significance in clinical decision-making and clinical diagnosis[15,16].ML-based models have demonstrated high accuracy in predicting medical outcomes and identifying high-risk patients[17,18].
In this study,we aimed to identify factors that may elevate the risk of overall short-term major postoperative complications (Clavien-Dindo ≥ III) and prolonged hospital stays following intestinal resection (IR) for CD.Additionally,besides constructing a nomogram predictive model using the logistic model,we utilized an improved ML model,specifically random forest (RF) analysis,to identify key factors influencing short-term major postoperative complications in CD.Through enhancing the identification and management of postoperative complications,we can ultimately improve patient outcomes and alleviate the burden of CD on healthcare systems.
MATERlALS AND METHODS
Patients
A retrospective analysis of a surgical database involving CD patients who underwent IR at our center from January 2017 to December 2022 was conducted.Inclusion criteria required a diagnosis of CD confirmed by histology or clinical presentation.Exclusion criteria encompassed incomplete medical records.The study was registered in the Chinese clinical trial database with the registration number ChicTR-InR-16009321 and obtained approval from the Shanghai Tenth People’s Hospital Ethics Committee (SHSY-IEC-5.0/24K3/P01).The requirement for informed consent was waived due to the retrospective nature of this study.
Methods
Patient demographics,clinical characteristics,laboratory test results,surgical details,and postoperative outcomes were extracted from electronic medical records.The primary outcome was the occurrence of short-term major postoperative complications (Clavien-Dindo ≥ III),defined as surgical complications within 30 d,including anastomotic fistula,IASC,bleeding,and intestinal obstruction.The secondary outcome was the length of postoperative hospital stay.The dataset was randomly divided into a training cohort and a validation cohort in a 7:3 ratio.χ2tests or independent samplet-tests were used for univariate analysis to identify risk factors for major postoperative complications.Multivariate logistic regression analysis was performed to identify independent risk factors for major postoperative complications.Univariate and multivariate linear regression analyses were conducted to determine the independent factors affecting postoperative hospital stay.Models were constructed using the training cohort,including a nomogram predictive model based on logistic regression analysis and an improved ML approach,specifically a RF analysis model.The area under the curves (AUC) was utilized to evaluate the discriminatory performance of the model,while the validation cohort was employed to assess the overall performance.DeLong’s test was applied to compare differences between two AUCs.Additionally,calibration curve was performed to evaluate the calibrating ability of the nomogram model.SHapley Additive exPlanations (SHAP) were then utilized to quantify the importance of each feature in the RF analysis by calculating the contribution of each feature to the predicted outcome.Significance was considered forP< 0.05.All analyses were conducted using R software version 4.3.2.
RESULTS
Patients’ characteristics and surgical outcomes
A total of 259 CD patients who underwent IR during the study period were included in the analysis and randomly divided into a training cohort (n=181) and a validation cohort (n=78).All surgeries,including elective and emergency procedures,were performed by the same team of surgeons specializing in IBD surgery at our center.The indications for all CD patients to undergo surgery were the presence of one or more complications.Among the 259 patients,there were a total of 13 cases with major surgical complications,including 1 case (0.9% of all patients with anastomosis) of anastomotic leakage,5 cases (1.9%) of intra-abdominal sepsis,1 case (0.4%) of ileus,and 6 cases (2.4%) of bleeding.Intestinal obstruction and 2 cases of intra-abdominal bleeding were treated with reoperation,2 cases of intestinal bleeding were treated with endoscopic intervention,and anastomotic leakage and intra-abdominal sepsis were managed with irrigation,drainage,and antibiotics.The remaining postoperative complications were treated conservatively with symptomatic drugs.All patients were discharged after recovery.The average length of postoperative hospital stay for all patients was 9.8 ± 3.8 d.
Factors related to major postoperative complications and postoperative hospital stay
The patients in the training cohort were further divided into the major postoperative complication group and the nonmajor postoperative complication group.Univariate analysis identified that patients who developed major postoperative complications had a lower preoperative serum albumin level,and most experienced moderate to severe preoperative CD activity index (CDAI) staging (CDAI ≥ 220).Moreover,the conversion rate from laparoscopy to laparotomy was higher in the group with major postoperative complications,and they were more likely to have a longer operation time and more intraoperative blood loss (Tables 1 and 2;allP< 0.05).Additionally,multivariate logistic regression analysis was performed to identify independent risk factors for major postoperative complications.The results showed that a lower level of preoperative serum albumin [odds ratio (OR)=0.826,95% confidence interval (CI): 0.705-0.968],a preoperative CDAI of ≥ 220 (OR=10.084,95%CI: 1.011-100.626),conversion to laparotomy surgery (OR=7.000,95%CI: 1.118-41.244),and a longer operation time (OR=1.026,95%CI: 1.008-1.045) were all significantly correlated with the occurrence of major postoperative complications (Table 3).

Table 1 Demographic and Crohn’s disease data in patients undergoing intestinal resection

Table 3 Multivariate logistic regression analysis results of factors associated with major postoperative complications (Clavien-Dindo ≥ lll)
Univariate analysis of the entire data cohort showed several significant factors associated with a longer postoperative hospital stay.These were emergency surgery (P< 0.001),laparotomy approach (P< 0.001),small bowel segmentectomy (P=0.039,vsileocecal resection),longer operation time (P=0.001),and more intraoperative blood loss (P=0.004).The independent risk factors significantly associated with a longer postoperative hospital stay in the multivariate analysis included a lower level of preoperative hemoglobin (P=0.015),emergency surgery (P=0.001),laparotomy approach (P<0.001),and longer operation time (P< 0.001) (Table 4).

Table 4 Related factors of postoperative hospital stay
Construction and evaluation of nomogram predictive model for major postoperative complications
A nomogram predictive model was established based on these independent risk factors identified for the occurrence of major postoperative complications (Figure 1).In the training cohort,the AUC was 0.916 (95%CI: 0.853-0.978),with a sensitivity of 1 and a specificity of 0.743 (Figure 2A).In the validation cohort,the AUC was 0.960 (95%CI: 0.907-1.000),with a sensitivity of 1 and a specificity of 0.933 (Figure 2B).The calibration curve showed good consistency between the predicted and actual probabilities,indicating that the nomogram had good predictive performance (Figure 2C).

Figure 1 Nomogram construction. The possibility of major postoperative complications was estimated by summing the scores corresponding to each risk factor.CDAI: Crohn’s disease activity index.
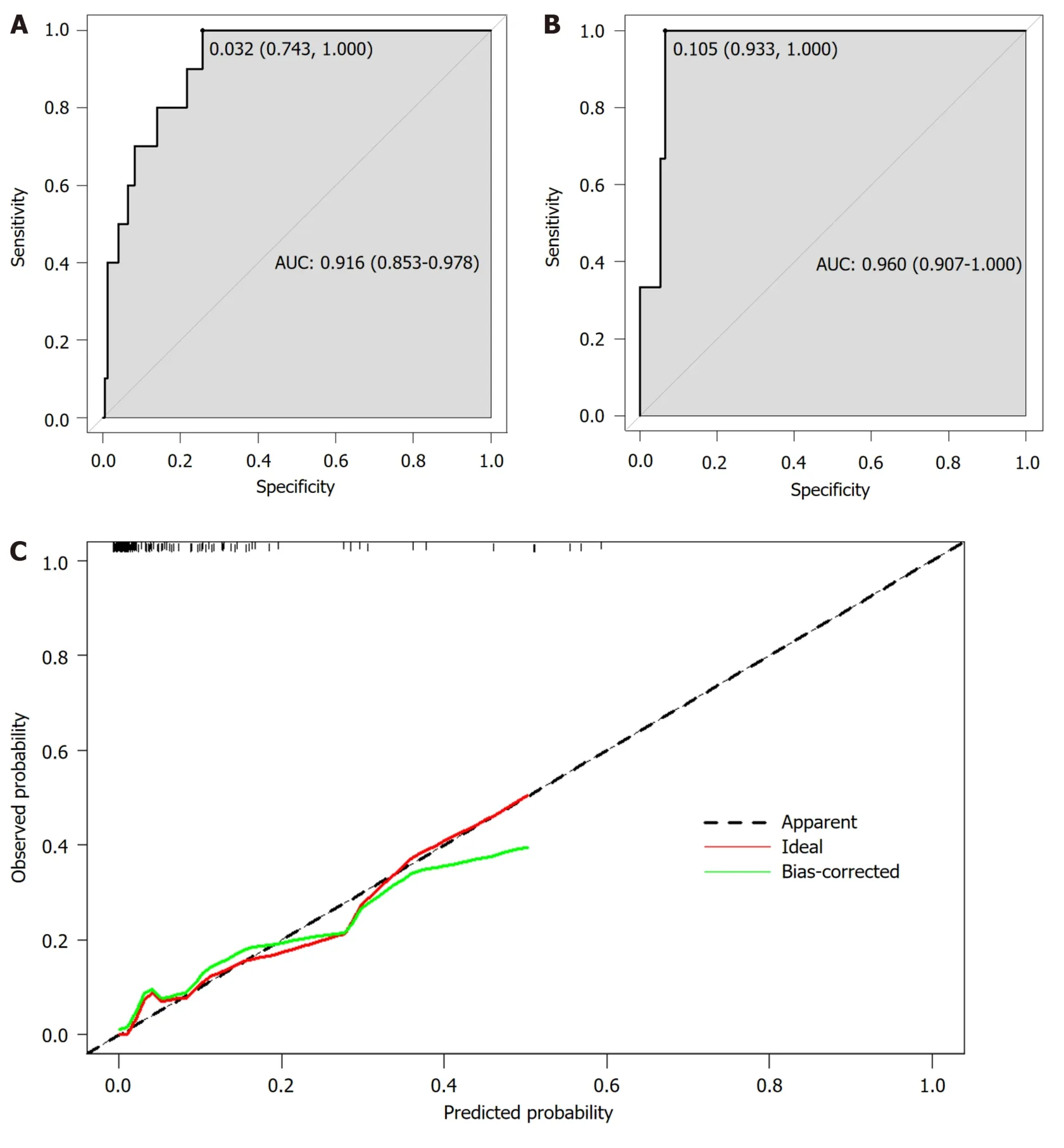
Figure 2 Evaluation of the nomogram predictive performance. A-C: Receiver operating characteristic (ROC) curves of the nomogram for predicting the probability of postoperative complications in the training cohort (A) and the validation cohort (B).The area under ROC curve of the training cohort and the validation cohort reached 0.916 and 0.960,respectively,indicating the high predictive value of the model.The calibration curve of the nomogram is close to the front diagonal,indicating that the nomogram had good prediction performance (C).AUC: Area under the curve.
RF model based on improved ML
In the RF model,the AUC for the training cohort reached 0.965 (95%CI: 0.942-0.988),with a sensitivity of 1.000 and specificity of 0.833 (Figure 3A),significantly outperforming the AUC of the traditional logistic regression model (P< 0.05).In the validation cohort,the AUC of the RF model reached 0.924 (95%CI: 0.855-0.993),with a sensitivity of 1.000 and specificity of 0.880 (Figure 3B).The feature importance was illustrated in Figure 4.Preoperative CDAI,operation time,serum albumin,and body mass index (BMI) were identified as the top four important variables,whereas the surgical approach held the seventh position.Preoperative CDAI,operation time,and serum albumin were visibly higher than other indicators and aligned with the variables included in the logistic regression model,highlighting their prominent predictive role.Finally,SHAP was used to interpret the RF model,as shown in Figure 5.It was also observed that serum albumin,operation time,and preoperative CDAI played the most crucial role in predicting and explaining the RF model.Specifically,low preoperative serum albumin,prolonged operation time,and preoperative CDAI of ≥ 220 were associatedwith an increased likelihood of short-term major postoperative complications.

Figure 3 Performance of random forest model. A: The receiver operating characteristic curves (ROC) of the random forest (RF) model in the training cohort;B: The ROC of the RF model in the validation cohort.AUC: Area under the curve.
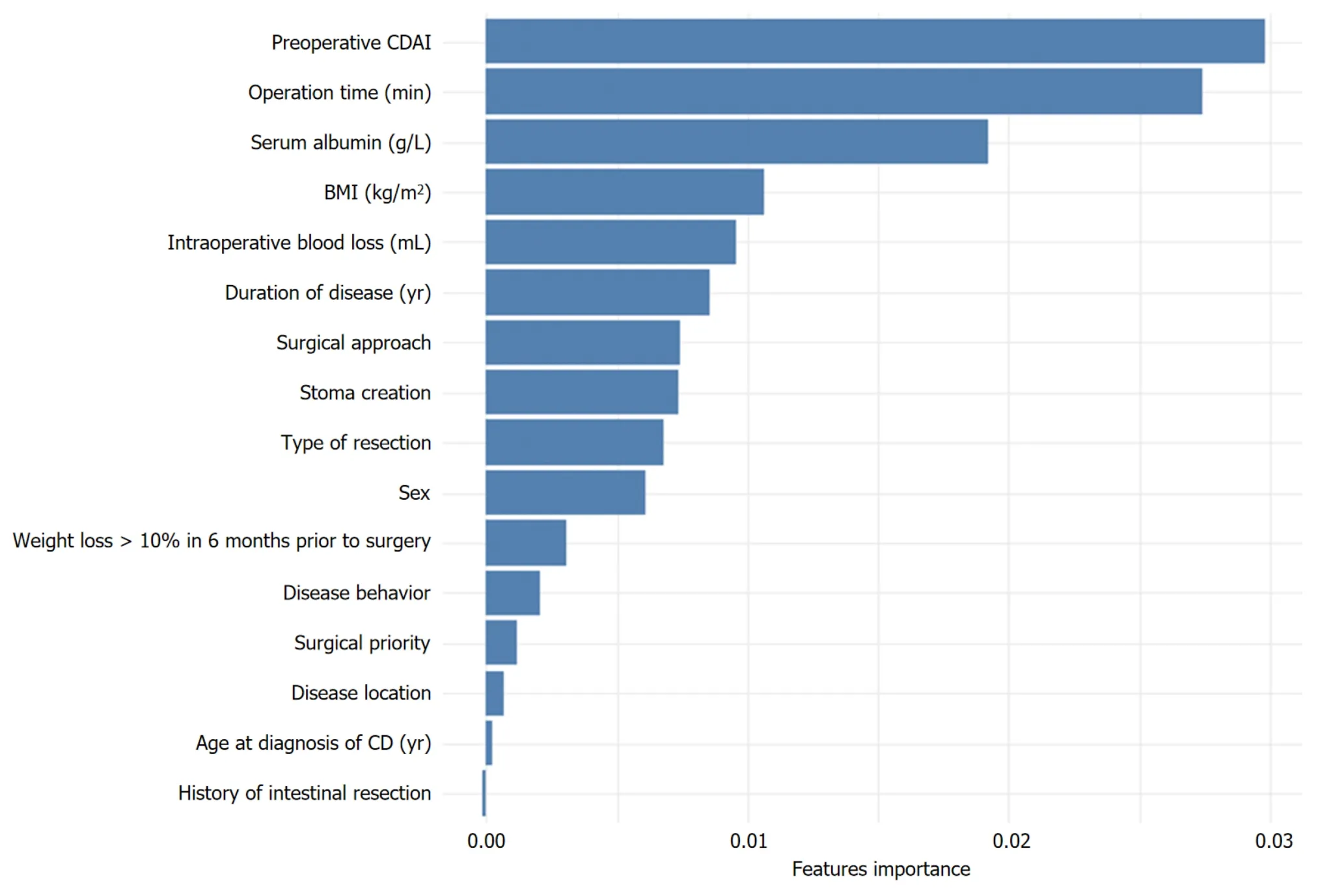
Figure 4 Feature importance ranking of the random forest model. CDAI: Crohn’s disease activity index;BMI: Body mass index;CD: Crohn’s disease.

Figure 5 SHapley Additive exPlanations summary plots of the random forest model. The y-coordinate of each point is determined by the feature it represents,while the x-coordinate is determined by its impact on the model’s output.The color of each point indicates its value from high to low,according to the color bar on the right.The features on the y-axis are ordered by their importance.CDAI: Crohn’s disease activity index;BMI: Body mass index;CD: Crohn’s disease;SHAP: SHapley Additive exPlanations.
DlSCUSSlON
ML has the advantages of dealing with big data,strong objectivity and reliability,and good repeatability.Previous studies have confirmed the application value of ML algorithms in clinical diagnosis and prognosis[19,20].Moreover,ML algorithms play a crucial role in constructing predictive models,especially in assisting clinical decision-makers to precisely identify high-risk patients and offer timely and accurate treatment,thereby enhancing patient prognosis[21,22].
Previous studies only discussed risk factors related to postoperative complications of CD,such as a low preoperative serum albumin level,a high preoperative CDAI score,and primary anastomosis[12,23,24].However,these studies didn’t build improved ML models for predicting postoperative complications for CD after surgery,although they might also build traditional logistic regression models.Therefore,this study is the first to use an improved ML algorithm,specifically the RF analysis model,to predict the likelihood of CD patients developing short-term major complications after IR.Multivariate logistic regression analysis determined that a preoperative CDAI of ≥ 220,a diminished preoperative serum albumin level,conversion to autotomy surgery,and an extended operation time were important risk factors for shortterm major postoperative complications in patients with CD.Although the prediction performance of the RF model isbetter than that of the logistic regression model,it is worth noting that three of the most important variables screened by the RF analysis are consistent with the logistic regression model,namely,serum albumin,preoperative CDAI,and operation time.
Hypoalbuminemia,indicative of malnutrition and systemic inflammation,can negatively impact wound healing,immune response,and overall recovery[25].Recognizing the importance of preoperative nutritional optimization can help mitigate this risk factor and improve patient outcomes[23,26-29].In our center,CD patients with poor nutritional status routinely receive enhanced nutritional support,including parenteral nutrition.This was also confirmed by the preoperative albumin level of 36.6 ± 5.5 g/L in this study cohort.However,the preoperative albumin level of patients undergoing emergency surgery was significantly lower than that of patients undergoing elective surgery (31.4 ± 4.4vs36.9 ± 5.4,P< 0.001).Therefore,in addition to doctors’ need to strengthen perioperative nutritional management of CD patients,patients themselves should also pay attention to disease monitoring to avoid emergency surgery.
In our cohort,preoperative moderate to severe CDAI staging emerged as a significant risk factor.The CDAI was developed in 1976 for the National Collaborative Study on CD[30].While CDAI has been widely used in clinical practice because of the simplicity of its evaluation methods,it is important to note that some of its indicators are relatively subjective,ignoring objective indicators of inflammation,such as albumin and erythrocyte sedimentation rate[31].Despite these limitations,CDAI remains a tool for assessing response to CD treatment and disease activity.Two recent studies have also shown that a higher preoperative CDAI score significantly increases postoperative complications[24,32].The CDAI is derived based on the patient’s disease symptoms and recent nutritional status in the past week,which once again emphasizes the influence of the disease status and the patient’s nutritional status on surgical treatment.Therefore,effective perioperative inflammation control and nutritional support are both strongly needed to reduce CDAI score in order to prevent postoperative complications.
Another identified risk factor was the prolonged operation time,which was consistent with a previous meta-analysis[33] that found a 14% increase in the likelihood of complications for every 30-min increase in operation time.Longer operation time was also considered to be a risk factor for postoperative complications in the treatment for CD with repeat ileocolic resection in a recent study[34],which also indicated that longer operation time was only significantly associated with a higher BMI in patients.The prolonged operation time associated with increased complications should be a multifaceted result,including prolonged exposure to microbial and anesthesia,as well as increased surgeon fatigue.Moreover,the longer the operation time,the more complicated or difficult the surgical procedure,with which higher rates of complications are expected.
Additionally,the conversion to laparotomy surgery was found to be a risk factor for complications,which was also associated with a longer postoperative hospitalization time.However,in the RF model,it didn’t rank high in importance.Laparotomy,a more invasive surgical approach involving a larger incision,can lead to greater tissue trauma,prolonged operation time,and increased postoperative pain[35,36].Previous studies have shown that laparoscopic surgery in patients with CD has a considerable or lower rate of postoperative short-term overall complications,including intraabdominal abscesses and/or anastomotic leakage,as well as a lower rate of reoperation and significantly shorter hospital stay,compared with traditional open surgery[37,38].Unlike previous studies,the logistic regression analysis in this study further indicated that the conversion to open surgery was more likely to result in postoperative complications,underscoring the importance of preoperative evaluation of the feasibility of minimally invasive surgery.Nevertheless,the safety and feasibility of minimally invasive techniques in CD patients has been affirmed by multiple studies[39-43],even in complex and repeat surgery cases.The experience at our center also confirmed that minimally invasive surgery was the first choice after adequate preoperative nutritional support and comprehensive preoperative examination[44],as it could accelerate postoperative recovery and reduce the incidence of abdominal adhesions,which was more conducive to the needs of CD patients for secondary abdominal surgery.
Surgical strategies for CD include IR with primary anastomosis or temporary stoma creation followed by delayed anastomosis.The latter is intended to reduce the occurrence of serious complications such as IASC and anastomotic fistula,especially for penetrating disease[45-47] and colonic CD[48,49].In the cases included in this study,59.1% of patients underwent staged surgery,and neither penetrating disease nor colectomy was found to be an independent risk factor for major postoperative complications,which again indicates that reasonable selection of staged surgery can effectively reduce postoperative IASC.
Some authors have found that repeat bowel resection increases the risk of postoperative anastomotic fistula in patients with CD[50,51],but as with two other recent studies[46,52],this did not appear in our study.We believe that even complex surgeries,including repeated bowel resection and anastomosis,can be performed with low postoperative morbidity,as long as perioperative preparations are made carefully.In most respects,the factors that affect postoperative complications and hospitalization time were consistent,but there were also some differences.In our cohort,a lower preoperative hemoglobin level,emergency surgery,laparotomy approach,and longer operation time were associated with longer hospitalization time.Although emergency surgery increased postoperative hospitalization time,it did not increase the risk of postoperative complications.However,this again emphasizes the importance of dynamic monitoring of patients with CD to avoid emergency procedure.
The nomogram model developed in this study provides a valuable tool for predicting the probability of major postoperative complications in patients with CD undergoing IR.By incorporating the identified risk factors into a visual and easily interpretable format,the nomogram enables clinicians to estimate an individual patient’s risk level.More importantly,in this study,we built a RF model based on an improved ML algorithm.Through combined analysis with the traditional logistic regression model,the risk factors affecting the short-term major complications of patients with CD can be more accurately identified.This personalized risk assessment enhances clinical decision-making and facilitates tailored perioperative management,including interventions and close monitoring for high-risk patients.This proactive approach can lead to improved patient outcomes,reduced morbidity,and enhanced overall healthcare quality.
It is essential to acknowledge the limitations of this study.The retrospective nature and single-center design may restrict the generalizability of the findings.External validation in diverse patient cohorts is necessary to assess the novel models’ reliability and applicability in different healthcare settings.Additionally,the study focused on short-term major postoperative complications within 30 d,and long-term complications were not considered.
CONCLUSlON
In conclusion,both nomogram model and RF model had good predictive ability in identifying high-risk CD patients with major short-term postoperative complications.ML models can help us filter out the most important influences more accurately and provide clinicians with a personalized risk assessment tool that can guide decision-making and optimize perioperative management.Implementing the novel models in routine clinical care can lead to improved patient outcomes,enhanced patient-centered care,and contribute to ongoing quality improvement efforts in surgical practice.
ARTlCLE HlGHLlGHTS
Research background
The high incidence of postoperative complications in Crohn’s disease (CD) has prompted an urgent need for predicting postoperative risks,especially in perioperative decision-making.The improved machine learning (ML)-based models have demonstrated high accuracy in predicting medical outcomes and identifying high-risk patients.
Research motivation
Short-term major postoperative complications in CD deserve particular attention to enhance the accuracy of perioperative decision-making and the expected patient recovery.
Research objectives
This study aimed to clearly identify the key risk factors for short-term major postoperative complications in CD patients,construct and verify the logistics regression model and random forest (RF) model based on ML,so as to enhance the accuracy of surgical decision-making.
Research methods
A retrospective analysis was conducted on surgical data from CD patients between 2017 and 2022.Patients underwent rigorous screening before being randomly assigned to training and validation groups.Independent risk factors for shortterm postoperative major complications were determined by logistic regression analysis,and a nomogram prediction model was constructed.Concurrently,RF analysis was conducted to screen important factors for short-term postoperative major complications.
Research results
Among the included 259 CD patients,it was observed that 5.0% experienced major complications within 30 d postoperatively.CD activity index ≥ 220,longer operation time,and reduced preoperative albumin levels were identified as significant factors influencing the occurrence of major postoperative short-term complications in both models.
Research conclusions
Both the nomogram model and the RF model established in this study demonstrated good predictive performance,offering practical individualized risk assessment for clinical decision-making.
Research perspectives
The application of ML-based predictive models to assist personalized medical decision making in CD surgery is valuable.Predictive models across diverse clinical practices necessitate further integration,improvement,and promotion.
FOOTNOTES
Author contributions:Wang FT contributed to the manuscript writing,data collection and analysis;Lin Y,Yuan XQ,Gao RY,Wu XC,Xu WW,Wu TQ,Xia K,and Jiao YR collected data;Yin L and Chen CQ were involved in the conceptualization and supervision of this manuscript;and all authors approved the final manuscript.
Supported byHorizontal Project of Shanghai Tenth People’s Hospital,No.DS05!06!22016 and No.DS05!06!22017.
lnstitutional review board statement:This study was reviewed and approved by the Ethics Committee of the Shanghai Tenth People’s Hospital (SHSY-IEC-5.0/24K3/P01).
lnformed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Fang-Tao Wang 0000-0003-3193-4108;Chun-Qiu Chen 0000-0002-4248-7414.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Xu ZH
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Alcohol associated liver disease and bariatric surgery: Current perspectives and future directions
- Applications of gastric peroral endoscopic myotomy in the treatment of upper gastrointestinal tract disease
- Ex vivo liver resection and auto-transplantation and special systemic therapy in perihilar cholangiocarcinoma treatment
- Evaluation of bacterial contamination and medium-term oncological outcomes of intracorporeal anastomosis for colon cancer: A propensity score matching analysis
- Rescue from complications after pancreaticoduodenectomies at a low-volume Caribbean center: Value of tailored peri-pancreatectomy protocols
- Comparison of prognosis and postoperative morbidities between standard pancreaticoduodenectomy and the TRlANGLE technique for resectable pancreatic ductal adenocarcinoma
