Correlation of neutrophil to lymphocyte ratio to severity of coronary artery disease and in-hospital clinical outcomes in patients with acute coronary syndrome:A prospective observational study
2024-03-05VinodhkumarKandibendlaThiruvikramaPrakashSubashChandraBosePrafullDhewle
Vinodhkumar Kandibendla ,G.Thiruvikrama Prakash ,Subash Chandra Bose ,Prafull Dhewle
1Department of Cardiology,Prakriya Hospitals,Nagasandra,Banglore,India
2Department of Cardiology,E.S.Hospital,Villupuram,Tamil Nadu,India
3Department of Cardiology,Government Medical College,Ananthapuramu,Andhra Pradesh,India
4Department of Cardiology,Shrikrishna Hrudayalaya Hospital,Nagpur,Maharashtra,India
ABSTRACT Objective: To explore correlation of neutrophil-to-lymphocyte ratio (NLR) to severity of coronary artery disease (CAD) and in-hospital clinical outcomes in patients with acute coronary syndrome (ACS).Methods: In this prospective and observational study,we recruited 500 patients with ACS.For all the eligible patients,demographic details were collected,and laboratory parameters were evaluated.The CAD severity was evaluated in terms of the number of involved vessels.The NLR was calculated based on neutrophils and lymphocytes and the correlation of various risk factors and severity and outcome of CAD was performed.Results: 77.2% of Patients was male,and 52% of the patients aged between 55-70 years.Based on the type of ACS,396 out of 500 patients had ST-elevation myocardial infarction.An ascending trend in the white blood cell levels and NLR value was noted as the severity of the ACS increased and the highest white blood cell levels and NLR was noted among class Ⅳ patients.The mean NLR value among the non-survivors were higher compared to the survivors (9.52±5.72 vs.4.76±2.36;P<0.01).Receiver operating curve showed that the cut-off NLR value was 5.76 with a sensitivity of 75.0% and a specificity of 77.3%.Conclusions: The NLR can be used as an independent prognostic marker in ACS.An elevated NLR value serves as a reliable predictor for short-term complications,notably in-hospital mortality.
KEYWORDS: Acute coronary syndrome;Coronary artery disease;Coronary vessels;Hospital mortality;Lymphocytes;Neutrophils;Prognosis;Risk factors
Significance
Neutrophil-to-lymphocyte ratio (NLR) has recently been introduced as a prognostic marker of cardiovascular risk.Higher NLR levels have been observed in patients with acute coronary syndrome.The key findings of our study are elevation in NLR value among STEMI patients,having multi-vessel involvement and among non-survivors.The significant association of NLR with CAD severity makes NLR an independent prognostic indicator of various cardiovascular risk factors.Also,NLR proves effective in predicting in-hospital mortality.
1.Introduction
Coronary artery disease (CAD) is an inflammatory disease in which atherosclerosis plays an active role in development and progression of CAD and its complications[1].Atherosclerosis is a multifactorial disease.Dyslipidemia,diabetes mellitus,smoking,and other relevant etiological factors that cause endothelial injury and genetic mutations usually contribute to CAD[2].Inflammatory cells and pathways play a significant role in the onset of atherosclerosis.The initiation of repair after the injury is followed by plaque instability while rupture finally leads to the development of acute coronary events[3].Patients with acute coronary syndrome (ACS) are at higher risk of mortality and recurrent major adverse cardiovascular events[4].
Elevated white blood cells (WBC) play an important role in atherosclerosis progression and hence are considered independent risk factors and predictors of outcomes[5,6].Leukocytes and especially neutrophils have proven a central role in atherogenesis and atherothrombosis and are also found to be intimately involved with the adaptive healing process[2,5].An increase in the neutrophil levels is associated with the occurrence and severity of atherosclerosis and its elevation increases the blood viscosity and hypercoagulability as well as interact with platelets and endothelium,and hence induces reperfusion and microvascular injury[1].However,low lymphocyte counts have been observed in ACS patients or those with complications[5].Another hypothesis suggests that physiological stress and subsequent activation of neurohormonal system during ACS results in a release of cortisol which in turn also reduces the lymphocyte count[7].Neutrophil-to-lymphocyte ratio (NLR) is a simple ratio of the absolute number of neutrophils and lymphocytes and is one of the inflammatory markers which has been recently introduced as a prognostic marker in patients with ACS[8,9].Recent studies have determined the prognostic significance of NLR in ACS,which suggested that the higher the NLR value,the worse the prognosis of ACS patients[4].The NLR is an inexpensive,easily available test that is routinely performed in admitted patients and aids in risk stratification of ACS patients.Therefore,we aimed to evaluate whether NLR can be used to predict CAD severity and its adverse outcomes among patients with ACS.
2.Patients and methods
2.1.Study design
This was a single-center,hospital-based,prospective,observational study conducted at a tertiary care center in India.Patients were enrolled in the study after receiving prior approval from the institutional ethics committee and the study was conducted in accordance with the Declaration of Helsinki.All the patients provided written informed consent to participate in the study.
2.2.Inclusion and exclusion criteria
Patients who were diagnosed with ACS were eligible for inclusion in the study.Exclusion criteria were patients with acute febrile illness,infections,having a history of any chronic illness,or were on antiplatelet,steroids,statins,immunosuppressants,or non-steroidal anti-inflammatory agents.
2.3.Definition of cardiovascular risk factors
The patients with serum HbA1c levels ≥ 6.5% or having a history of diabetes mellitus (DM) or having hypoglycaemic agents were defined to have DM.Patients with hypertension were defined as having persistent elevated blood pressure or having a medical history of elevated blood pressure or receiving anti-hypertensive medications.Dyslipidemia in the study population was characterized by increased low-density lipoprotein (>160 mg/dL) or having a history or lipid-lowering agents.The patients with ACS were those having ST-elevation myocardial infarction,non-ST-elevation myocardial infarction,and unstable angina.The patient’s smoking status was recorded based on the medical history.
2.4.Laboratory tests
The participants were managed following standard protocol for ACS and were followed till discharge.Before providing any medical intervention,a venous blood sample was collected for all the patients.Hemogram profile was measured by flow cytometry method using a Sysmex XS-800i analyzer and NLR was calculated using absolute count method.
2.5.Assessment of the severity of CAD
The presence of CAD was characterized by narrowing of epicardial coronary artery (≥ 50%) and the severity of CAD was divided into four categories based on the number of diseased vessels,i.e.,insignificant,one,two,or three,and left main coronary artery.
2.6.Definition of a clinical cardiovascular disease (CVD) event
Cardiovascular outcomes included cardiac-related death,stroke,arrhythmias,cardiogenic shock,re-infarction,and post-myocardial infarction complications like left ventricular failure,and the patients were followed up till discharge.
2.7.Statistical analysis
All the statistical analyses were performed using SPSS software version 17.0 (SPSS Inc.,Chicago,IL,USA).Continuous variables were presented as mean±standard deviation while the categorical variables were expressed in terms of frequency and percentages.The statistical analysis was done using students’ t test and Chi-square test.Receiver operating curve (ROC) was constructed to obtain area under the curve (AUC) and to predict the cut-off values of NLR.All P-values were two-sided and P<0.05 was considered statistical significance.
3.Results
A total of 500 patients with ACS were enrolled in the study and all the enrolled patients were included in the final analysis.
3.1.Patient characteristics
Among 500 patients,77.2% were male,and more than half of the study population (52%) belonged to age group 55-70 years.Their baseline demographic characteristics are presented in Table 1.Among the eligible patients,52.8% were smokers,34.8% had hypertension,33.6% had diabetes mellitus and 6.4% had dyslipidemia.396 Out of 500 were diagnosed with STEMI,among them the most common type of STEMI was anterior wall myocardial infarction.On further classification based on Killip category,58.4% belonged to class I.The severity of CAD was determined based on the number of diseased vessels and 34.8% of patients had single vessel disease.
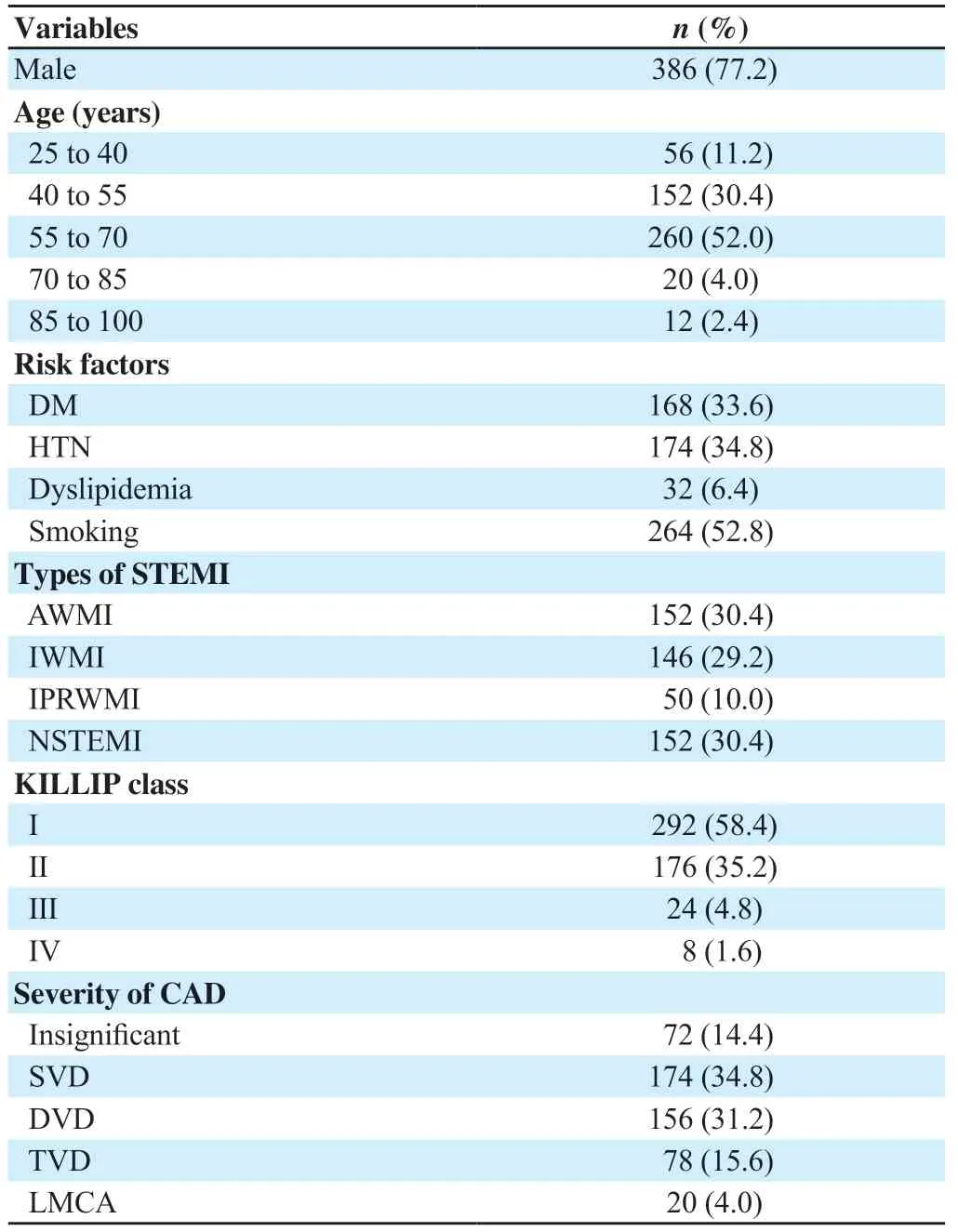
Table 1.Demographic characteristics (n=500).
3.2.Outcomes
The adverse events of ACS were observed in 64 patients,where cardiac-related death was noted in 16 (3.2%) patients.When followed up till discharge,12 (2.4%) patients were found to have left ventricular failure,and 10 (2.0%) patients developed ventricular tachycardia.Re-infarction and cardiogenic shock were observed in 8 (1.6%) patients with ACS.The least observed outcomes were stroke and complete heart block,which were noted in 6 (1.2%) and 4 (0.8%) patients,respectively.12 Out of 16 dead patients had NLR >5.76.
3.3.Risk factors of severity and mortality
The various risk factors for the severity are highlighted in Table 2,where the patients are categorized into four different Killip classes.The mean age was (55.5±11.5) years.However,no significant difference in the age among all the groups was noted.An ascending trend in the values of WBC was noted,as the severity increased the WBC levels tend to increase and the highest was observed among class Ⅳ patients.The NLR values were proportional to the severity of ACS suggesting that more severe the disease higher is the NLR,with significant difference among groups (P<0.01).While in the dead patients the WBC levels and NLR value were significantly higher while the lymphocytes were significantly lower compared to the survivors (Table 3).
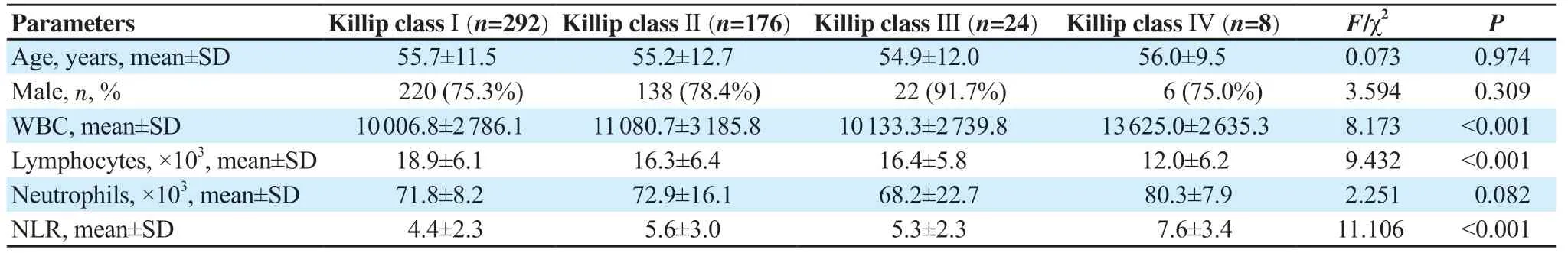
Table 2.Risk factors of severity (n=500).
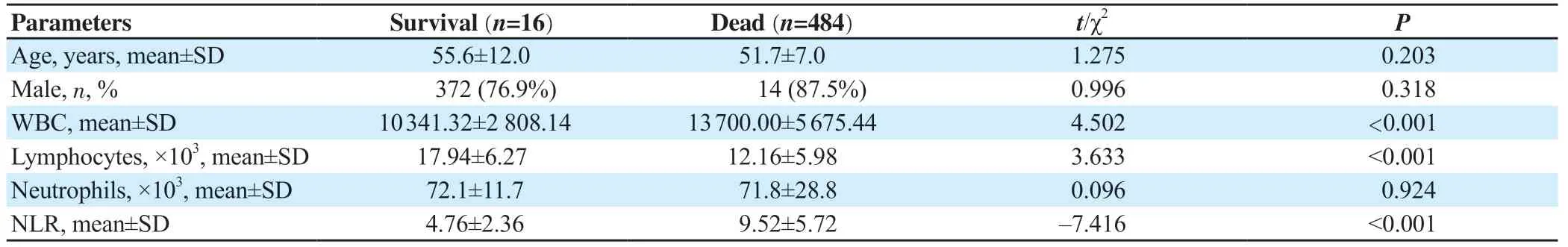
Table 3.Risk factors of mortality (n=500).
3.4.ROC analysis
ROC analysis shows that the cut-off of NLR in predicting inhospital mortality was 5.76 with a sensitivity of 75.0% and a specificity of 77.3%.The positive predictive value was 9.8% and negative predictive value was 98.9%.And the AUC was 0.746 (Figure 1).
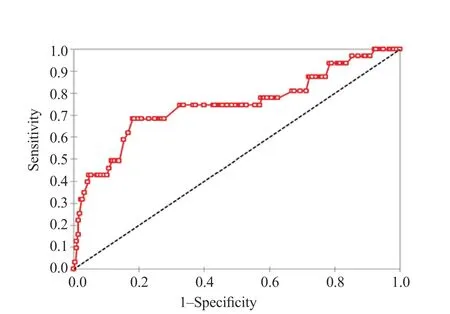
Figure 1.ROC of NLR predicting in-hospital mortality.
4.Discussion
Inflammation plays a vital role in all phases of development of atherosclerosis.WBC and its differential counts are the widely available markers in clinical practice.Neutrophils affect the progression by interacting in stages of inflammation while lymphocyte apoptosis is noticed as the atherosclerotic burden rises.Therefore,the combination of elevated neutrophils and low levels of lymphocytes in a single composite marker could provide additional information[10-14].The NLR is the simplest of inflammatory markers that are found associated with adverse outcomes in patients who underwent coronary angiography,in those with stable and unstable CAD,and in patients who were managed using invasive therapy like percutaneous coronary intervention or coronary artery bypass grafting.Hence,NLR provides additional information on CAD severity and its outcomes[5].However,we have conducted this study to address the knowledge gap and paucity of Indian studies evaluating NLR in ACS patients.
In our study,more than half of the study population belonged to the age group 55-70 years and the predominance of male gender was noted (77.2%).Various risk factors like hypertension,diabetes mellitus,dyslipidemia,and smoking were recorded.A meta-analysis also concluded that patients with hypertension had higher NLR values when compared to normotensive patients and NLR elevation in hypertension patients implicates immune system imbalance[15].Some studies compared NLR value and various risk factors among ACS patients and found no significant association between risk factors like diabetes mellitus,smoking,or hypercholesterolemia was noted[16,17].These results were similar to our study.
Consistent with our study,a study assessed NLR in the suspected ACS patients and found that patients diagnosed with non-cardiac pain reported the lowest NLR (n=45;3.0±1.6),followed by unstable angina (n=65;3.6±2.9),non-ST-elevation myocardial infarction (n=33;4.8±3.7) and the highest NLR was observed among STEMI patients (n=35;6.9±5.7;P<0.001)[18].In contrast,a study performed by Goktas et al.[19] showed that the NLR was higher among non-STelevation myocardial infarction patients compared to patients with ST-elevation myocardial infarction and unstable angina.
The severity of CAD was measured in terms of the number of vessels involved and a significant association (P<0.01) between the number of vessels and NLR was established in the current study.An ascending trend in the NLR value was noted as the number of involved vessels increased.Arbel et al.[5] compared NLR for CAD severity and found that NLR increased with an increase in the number of vessels.The odds ratio observed among the group of patients with NLR >3 was 1.52,1.73 and 2.45 in patients with one-vessel,two-vessel,and three-vessel involvement,respectively.Killip classification is a powerful independent predictor of allcause mortality in patients with ACS.In our study,NLRs were 4.39±2.32,5.60±2.97,5.27±2.33,and 7.62±3.36 for Killip class I-IV,respectively and this difference was significant (P<0.01).Bajari et al.[17] also found a higher incidence of acute left ventricular failure and cardiogenic shock among patients with higher NLR.Furthermore,in a parallel study,a significant association between higher NLR and increased morbidity like congestive heart failure was noted[16].
NLR is positively associated with adverse outcomes among 34 000 patients with ACS who underwent revascularization[20].In a review of 2 833 patients with ACS,patients with higher NLR (mean 9.5) had significantly higher in-hospital mortality(8.5% vs.1.8%) and 6-month mortality (11.5% vs.2.5%) when compared to the lowest NLR (mean 1.82)[21].These results were similar to the results of our study,where it was noted that the majority of the patients with adverse outcomes had higher NLR.Upon ROC analysis,the cut-off NLR value for predicting in-hospital mortality was found to be 5.76 with 75% sensitivity and 77.3% specificity,and negative predictive value was 98.9%.A similar cut-off of NLR for predicting mortality was determined in the study by Bajari et al.[17] and the NLR cut-off value was 5.25 with 89.36% sensitivity,75.07% specificity,32.4% positive predictive value,and negative predictive value of 98.1%.Another study conducted by Zazula et al.exhibited the NLR cut-off value as 5.7 with 91.1 % specificity[18].
Our study had several limitations.Firstly,the patients studied were from a single tertiary center among whom only the conventional risk factors were studied.Moreover,the study population was followed up till discharge and to determine the long-term outcomes of CAD,a long-term follow-up period is required.While a single baseline admission complete blood count sampling has the benefit of being readily available,serial sampling may potentially yield a better analytical time point.Also,the severity of CAD was not based on the percentage of stenosis,type of calcification,and severity of plaque while it was based only on the number of vessels involved.A larger multi-center study with larger population size and diversity is best to determine the future prognostic role of NLR,its precise predictive cut-off value,and sampling time.
In conclusion,our study shows a correlation between NLR and the severity of CAD,with elevated NLR values being particularly notable in patients experiencing STEMI and multiple vessel involvement.Moreover,high NLR serves as a reliable indicator for short-term complications,such as in-hospital mortality.Consequently,this readily available,cost-effective,and simple biomarker can play a pivotal role in identifying individuals at risk of developing severe CAD.Furthermore,it can assist in identifying those who may benefit from a more aggressive therapeutic approach.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors’ contributions
VK designed the study and concept of the study,performed literature search,data acquisition and manuscript preparation and editing.GTP designed the concept of the study,performed the data acquisition,analysis,statistical analysis and was involved in manuscript preparation and editing.SCB designed the concept of study,performed literature search,clinical and experimental studies and was did data collection and manuscript preparation.PD gave basic idea of study design and defined the intellectual content,did clinical studies,and was also involved in manuscript preparation and editing.All authors approved the final draft and are responsible for the content and similarity index of the manuscript.
杂志排行
Journal of Acute Disease的其它文章
- Cardiovascular risk factors affecting COVID-19 outcomes at a tertiary referral hospital in northwest Iran:A prospective cohort study
- A 10-year review and epidemiology of animal bite cases in Gerash city,south of Iran:A retrospective cross-sectional study
- Relationship between nutritional therapy and beneficial bacteria ratio in severe disease
- Clinical profile and risk factors of symptomatic and asymptomatic hypoglycemia in neonates admitted to NICU in a tertiary care center:A cross-sectional study
- Acute coalescent mastoiditis in a 16-month-old child due to Streptococcus pneumoniae infection
- Paradoxical systemic toxicity by inhaled paraquat poisoning:A case report
