Expanding beyond endoscopy: A review of non-invasive modalities in Barrett’s esophagus screening and surveillance
2022-09-14DariushShahsavariPraneethKudaravalliJohnEriksonYapKennethVega
Dariush Shahsavari, Praneeth Kudaravalli, John Erikson L Yap, Kenneth J Vega
Abstract Barrett’s esophagus (BE) is a condition that results from replacement of the damaged normal squamous esophageal mucosa to intestinal columnar mucosa and is the most significant predisposing factor for development of esophageal adenocarcinoma. Current guidelines recommend endoscopic evaluation for screening and surveillance based on various risk factors which has limitations such as invasiveness, availability of a trained specialist, patient logistics and cost.Trans-nasal endoscopy is a less invasive modality but still has similar limitations such as limited availability of trained specialist and costs. Non-endoscopic modalities, in comparison, require minimal intervention, can be done in an office visit and has the potential to be a more ideal choice for mass public screening and surveillance, particularly in patents at low risk for BE. These include newer generations of esophageal capsule endoscopy which provides direct visualization of BE, and tethered capsule endomicroscopy which can obtain high-resolution images of the esophagus. Various cell collection devices coupled with biomarkers have been used for BE screening. Cytosponge, in combination with TFF3, as well as EsophaCap and EsoCheck have shown promising results in various studies when used with various biomarkers. Other modalities including circulatory microRNAs and volatile organic compounds that have demonstrated favorable outcomes. Use of these cell collection methods for BE surveillance is a potential area of future research.
Key Words: Barrett’s esophagus; Screening; Surveillance; Non-endoscopic; Cytosponge;Esophacap; Esocheck
lNTRODUCTlON
The esophagus is normally lined by stratified squamous epithelium. The mucosa of the esophagus is regularly exposed to gastric acid and bile through reflux from the stomach which can result in mucosal damage. The injury is usually repaired by regeneration of the squamous mucosa. However, in some patients, the mucosal damage is repaired resulting in a metaplastic columnar epithelium with gastric and intestinal features. The condition is termed Barrett’s esophagus (BE) and is recognized as the major risk factor for the development of esophageal adenocarcinoma (EAC)[1]. It is estimated that as many as 5.6% of United States adults have BE based on modeling using EAC rates[2]. Of note, endoscopic prevalence is widely variable based on geographic location of the population studied[3-6]. Current estimates are likely an underrepresentation given that upper endoscopy is required for diagnosis. Mean age at BE identification is approximately 55 years and is two to threefold more common in men than in women[7,8]. Among patients undergoing upper endoscopy, compared to Caucasians, African Americans have a significantly lower BE prevalence[9,10]. Accepted BE risk factors besides Caucasian race include age > 50, male, chronic (> 5 years) or frequent (> once weekly) gastroesophageal reflux disease (GERD), smoking, obesity (Body mass index > 35), and family history of BE or EAC (first degree relative)[11].
Endoscopy is currently the mainstay for BE diagnosis and management. An endoscopic approach is inappropriate for mass screening as it is not cost effective resulting in missed opportunities to discover patients with undiagnosed BE. Current screening guidelines target individuals with GERD and multiple risk factors for endoscopy to detect BE then enroll those with it into a surveillance program. However,this approach does not take into consideration that most EAC cases do not have a diagnosis of BE prior[12]. This provides an excellent opportunity for non-endoscopic techniques to be used as a public health tool for screening (identification of disease) and surveillance. Individuals belonging to the low risk BE strata are best suited for non-endoscopic modalities as they require minimal intervention whereas the high risk BE group would require more precise but also more invasive endoscopic based technologies[13]. Non-endoscopic techniques provide cost-effective, less invasive screening tools and more importantly increase the ease of accessibility to screening opportunities.
WHO DO WE SCREEN
Screening for BE is recommended in patients with multiple known risk factors including chronic or frequent GERD, age greater than 50 years, male sex, Caucasian race, smoking, obesity along with family history of a 1stdegree relative with BE or EAC. Currently, screening the general population with only GERD symptoms is not recommended per society guidelines[14,15].
ESOPHAGEAL lMAGlNG DEVlCES
Currently, high-definition white light endoscopy is the mainstay of BE screening and surveillance.Despite being safe and well-tolerated, it is invasive and associated with higher costs and side effects[16]. Trans-nasal endoscopy (TNE, Figure 1) has been proposed as a less invasive alternative to screen for BE. TNE is an ultra-thin endoscope (diameter < 6 mm) used in the outpatient setting to directly visualize the distal esophagus. This has occurred in primary care offices[17,18] and mobile vans for community BE screening[19]. Drawbacks of TNE are limited availability, cost, decontamination facility for reuse, and need for trained operators.

Figure 1 Trans-nasal endoscopy. Courtesy: Image obtained from public domain.
ESOPHAGEAL CAPSULE ENDOSCOPY
Esophageal capsule endoscopy (ECE), similar to small bowel capsule endoscopy, consists of a wireless capsule containing a camera, battery, and radio transmitter. Images are transmitted to a digital receiver and transferred to a computer for analysis[20]. A meta-analysis of 9 studies comprising of 618 patients showed a pooled sensitivity of 78% and specificity of 86% (EGD as the reference had sensitivity and specificity of 78% and 90% respectively)[21]. The suboptimal diagnostic accuracy is contributed to rapid esophageal transit time. Newer versions of ECE have been developed to overcome this issue and allow prolonged imaging. PillCam ESO (Medtronic Inc, Minneapolis, MN) was initially approved by Food and Drug Administration in 2004 and a second-generation device (PillCam ESO2, Figure 2A) with cameras at both ends of the capsule. The second-generation device captures images (PillCam ESO2,Figure 2B) at a rate of 18 frames per seconds (fps)[22]. A third-generation capsule (PillCam UGI) with a wider angle of view (174°) and higher recording rate (35 fps) is under investigation with pilot data suggesting inferiority to standard endoscopy regarding BE detection[23].Another solution for the rapid esophageal transit issue is the detachable string magnetically controlled capsule endoscopy (also known as wireless magnetically controlled capsule endoscopy or WMCCE) which has been shown to be feasible and well tolerated in various studies[24-26]. A recent prospective multicenter study showed sensitivity of 92% and specificity of 80% for high-risk esophageal varices[27]. With regards to cost-effectiveness of ECE compared to traditional endoscopy, the results have been equivocal[28-30]. More studies are needed to determine of this modality is viable and cost-effective for BE screening.
TETHERED CAPSULE ENDOMlCROSCOPY
Another variant of ECE is optical coherence tomography tethered capsule endomicroscopy (OTC-TCE,Figure 3) which uses optical-frequency domain imaging technology that rapidly acquires highresolution, 3-dimensional, cross-sectional images of the entire esophagus[31,32]. In a proof-of-concept study of 13 subjects (7 normal volunteers and 6 with known BE), no complications were reported, and 12/13 patients reported preference of this method over conventional endoscopy[33]. The feasibility and safety of this method was further demonstrated in a recent multi-center study of 147 patients with known BE, and a blinded comparison of maximum extent of BE measured by OTC-TCE and EGD showed a strong correlation (r= 0.77-0.79,P< 0.05)[34]. In this study, high-quality microscopic images of the entire esophageal wall were obtained in the majority of the cases (93.7%). Larger prospective studies are needed to assess diagnostic yield and cost-effectiveness in the general population setting.
CELL COLLECTlON DEVlCES WlTH BlOMARKERS
Various devices have been designed for esophageal cell collection. These samples can be analyzed cytologically and coupled with various biomarkers.
CytospongeTM—Trefoil Factor Family Protein 3
The Cytosponge (Medtronic, Minneapolis, MN, Figure 4) is a 30 mm polyurethane sponge, compressed withing a gelatin capsule and attached to a string[13]. Once patient swallows the capsule and it reaches the stomach, the capsule opens up and reveals the sponge. As the string is pulled back, the Cytosponge collects cells from the lining of the entire esophagus and oropharynx. Although several biomarkers have been used with Cytosponge including a multi-gene next-generation sequencing panel, differentially methylated genes, and microRNAs, the most well-established biomarker used with Cytosponge has been trefoil factor family protein 3 (TFF3) immunohistochemical staining[35-37].

Figure 2 PillCam ESO2 and image. A: PillCam ESO2; B: PillCam ESO2 images showing normal, esophagitis, suspected Barrett’s and varices. Courtesy: Image obtained from public domain.
In a multicenter case-control study of 11 United Kingdom hospitals (total subjects = 1,110; 463 dyspepsia controls and 647 BE patients), Cytosponge-TFF3 was performed prior to endoscopy[38]. BE was diagnosed with specificity of 92.4% and sensitivity of 79.9% (87.2% in patients with larger circumferential BE than 3 cm). Fitzgeraldet al[39] in the BEST3 trial, a multicenter RCT study in 109 United Kingdom general practice clinics, demonstrated in patients with GERD symptoms, Cytosponge-TTF3 results in improved detection of BE, treatable dysplasia, and early cancer. In a systematic review of 13 studies, this method was shown to be cost-effective and well-tolerated through multiple patient populations[40]. Another patient-level review of 5 prospective trials assessing Cytosponge performance in patients with reflux disease, BE and eosinophilic esophagitis, also showed tolerability and safety of this device [41].
The advantage of Cytosponge is that it is not operator-dependent, it is quick, and does not require specialized equipment or extensive training, so it could easily be applied to a primary care setting[40].
EsophaCapTM

Figure 3 Tethered capsule endomicroscopy. Courtesy: Image obtained from public domain.

Figure 4 Cytosponge (Medtronic, Minneapolis, MN). Courtesy: Image obtained from public domain.

Figure 5 EsophaCap (CapNostics, Concord, NC). Courtesy: Image obtained from public domain.
EsophaCap (CapNostics, Concord, NC, Figure 5) is a sponge on string device similar to Cytosponge,albeit smaller and softer[42]. EsophaCap has been used in a pilot trial using a panel of 2 methylated DNA markers (MDM), 3-VAV2 and zinc finger protein 682-ZNF682, on whole esophageal brushings (49 BE case and 36 controls),and in 40 subjects(20 BE cases and 20 controls)randomly assigned to swallow EsophaCap[42]. Overall, 80% of MDM candidates showed high accuracy for BE (AUCs 0.84-0.94) with sensitivity and specificity of 100%. The EsophCap was swallowed and withdrawn in 98% of subjects with no reported major complications, and 32% had minimal abrasions. More recently, in the same group conducted a multi-center case-cohort study of 268 subjects swallowed the capsule, but 201 met the inclusion criteria (112 cases and 89 controls) using the two previously mentioned MDMs and included 3 additional markers (NDRG4, FER1L4, and ZNF568)[43]. Cross-validated sensitivity and specificity were 92% and 94% respectively. EsophaCap was well tolerated in most patients (performed mostly by non-physicians) and 95% preferred the device over endoscopy. Currently a case-control trial is ongoing to identify potential biomarkers for the early detection of BE, esophageal carcinoma (both adenocarcinoma and squamous cell carcinoma) using EsophaCap (ClinicalTrial.gov ID: NCT04214119).
EsoCheckTM
EsoCheck (Lucid Diagnostics, New York, NY, Figure 6) is a balloon-based sampling device which consists of a collapsible balloon attached to thin silicone catheter connected to a syringe[13]. Once EsoCheck is swallowed and is in the stomach, the balloon is inflated by injecting air into the catheter and withdrawn through the distal 3-6 cm of the esophagus, collecting epithelial cells. After sampling the area described above, the balloon is deflated which leads to its retraction into to the capsule, thereby protecting the sample from bio-contamination from the mid or proximal esophagus as well as oropharynx.
Several biomarkers including MDMs have been used with EsoCheck. In a pilot study, Moinovaet al[44] performed a genome-wide screening and identified high-frequency methylation within the CCNA1 DNA locus. They tested CCNA1 and VIM DNA methylation (already an established BE biomarker)using EsoCheck in 173 individuals with or without BE and showed an AUC = 0.95 for discriminating metaplasia and neoplasiavsnormal individuals for both, and with both biomarkers combined, the panel had a sensitivity of 95% and specificity of 91%. The results were replicated in an independent validation cohort of 149 subjects. The device was generally well-tolerated but 28 (18%) of subjects could not swallow the pill and 9% had poor DNA yield.
A new multi-center, single-arm trial is underway to study of the screening efficacy of a new generation EsoCheck device in combination with EsoGuard (2-marker MDM panel) in at risk population(ClinicalTrial.gov ID: NCT042293458).
OTHER METHODS
Circulatory MicroRNAs
MicroRNAs (miRNAs) are short (approximately 18-25 nucleotides in length) non-coding RNAs which regulate gene expression by binding to mRNAs to inhibit their translation or facilitate their degradation[45]. miRNAs play role in cell growth, differentiation and migration and can be dysregulated in malignancy[46]. Several miRNAs have been shown to be differently expressed in patients with BE. In a quantitative real-time PCR analysis of 60 disease/normal-paired tissues from 30 patients with esophagitis or BE, miR-143, miR-145, miR-194, and miR-215 were significantly higher, while miR-203 and miR-205 were lower in BE tissues[47]. Analysis on circulating miRNA levels confirmed that miR-194 and miR-215 were significantly upregulated in BE patients. Additionally, serum miR-130a was also shown to be elevated in BE and EAC patients[48]. Pavlovet al[49] in a study of 69 patients showed serum miR-320e and miR-199a-3p to be significantly lower in BE compared to patients with normal epithelium. Investigators have recently reported miR-4485-5p as a novel biomarker of esophageal dysplasia worthy of continued investigation[50]. These markers provide a non-invasive method,requiring only a patient’s peripheral blood sample and likely increasing acceptability and tolerability,but validation studies are needed in larger cohorts to demonstrate adequate sensitivity as well as specificity for widespread use.
Volatile Organic Compounds
Detection of cancer through exhaled breath using volatile organic compounds (VOC) has shown promising results for various cancers[51,52]. Two techniques have been used in patients with BE or esophageal cancer, which are gas chromatography-mass spectrometry and electronic nose (E-nose)apparatus[53-56]. The gas chromatography method was used to analyze exhaled breath samples from 81 patients (including 48 esophageal cancer patients) and 129 controls (including 16 patients with BE), and although this method was able to discriminate esophageal cancer from controls (AUC = 0.97), it was not able to identify patients with BE[56]. The drawback of this method is that it is costly and labor-intensive.The electronic nose apparatus, which consists of an array of 3 metal oxide sensors, uses a chemical to electrical interface to measure VOC profiles associated with various diseases and can be combined with machine learning[57]. In cross-sectional study of 122 patients with dysplastic BE, breath samples while in a fasting state were analyzed in real-time using the e-nose device[54]. Subjects were at various stages of treatment or surveillance. The data was introduced into an artificial neuronal network to discriminate differences in subjects stratified by the presence or absence of BE on biopsies. The test showed the ability to detect BE with a sensitivity of 82%, specificity of 80%, and accuracy of 81% (AUC = 0.79). In another proof-of-concept study of 402 patients (129 patients with BE and 141 patients with GERD symptoms), 5-minute breath samples were collected, and the test was able to identify BE patients with a sensitivity of 91% and specificity of 74%[53]. Other advantages of E-nose compared to the gas chromatography-mass spectrometry is cost and portability. More validation studies at the general population level are needed for use as a potential BE screening method.
FUTURE TRENDS
Circulatory tumor DNA (CtDNA), miniscule amounts of fragmented DNA originating from tumor cells,has been proposed as a part of multi-cancer early detection (MCED) project. The Circulating Cell-free Genome Atlas trial in a prospective, case-controlled observational study showed that a blood-based MCED test using CtDNA in combination with machine learning could detect cancer signals for multiple cancer types and predict cancer signal origin with promising accuracy[58]. Most recently, a large multicenter MCED trial called PATHFINDER study began recruiting participants across 31 United States sites to examine DNA methylation patterns in blood samples to detect various cancers including esophageal cancers[59]. Since BE is a pre-malignant condition, more specific studies need to be conducted in the future to assess feasibility.
SURVElLLANCE
Patients with BE are currently recommended to enter a surveillance endoscopic program based on histological findings and degree of dysplasia[14,60]. This has been associated with a significant mental burden on these patients, presenting as various forms of anxiety and stress related to thoughts of disease progression as well as potential implications of the test, with many finding the program physically burdensome and intrusive[61]. This opens up opportunity for non-invasive surveillance options, which could even be performed in the setting of regular outpatient clinic visits. These modalities can potentially facilitate access to care for a larger population of patients and increase compliance similar to non-invasive tests for colorectal cancer screening programs[62]. As such, nonendoscopic cell collection methods have the potential for use in BE surveillance but so far, no studies have compared their use with conventional endoscopy for the purpose of BE surveillance, leaving this important area ripe for future investigation.
CONCLUSlON
Despite advances in screening and surveillance programs for BE, their lack of efficiency is demonstrated by the fact that only one in ten cases of EAC is diagnosed within a surveillance program. Upper endoscopy remains the gold standard but barriers exist to function as an effective screening tool which include high cost, invasiveness, possible complications, need for a trained specialist, and patient desirability. Screening guidelines have been published by several societies that are based on risk factors and do not include the general population. Less invasive modalities have been proposed for BE screening (Table 1). TNE has been used in outpatient settings including offices and mobile medical vans with some success. ECE has shown promising results, and newer generations have attempted to circumvent the issue of rapid esophageal transit with higher frame rates, wider angle view, and magnetic control. OTC-TCE is capable in acquiring high-resolution, 3-dimensional cross-sectional esophageal images with safety and feasibility been demonstrated in multi-center studies. Various cell collection devices coupled with biomarkers have been used for BE screening. Cytosponge, in combination with TFF3, is a cost-effective and well-tolerated method. Similar devices including EsophaCap and EsoCheck have shown promising results when used with various biomarkers and multi-center large-scale trials are currently underway. Circulatory MicroRNAs have been proposed for BE screening as they are expressed differently in this population. VOC using gas chromatography-massspectrometry and electronic nose have been used to identify BE or EAC with varying success. Finally,CtDNA is now being used as a part of “multi-cancer early detection” campaign which may play a role in detection of pre-cancer states such as BE. Using these non-invasive methods could also play a role as a surveillance tool once patients are identified with BE. Large future studies are desired to demonstrate the efficacy and feasibility for the BE surveillance population.
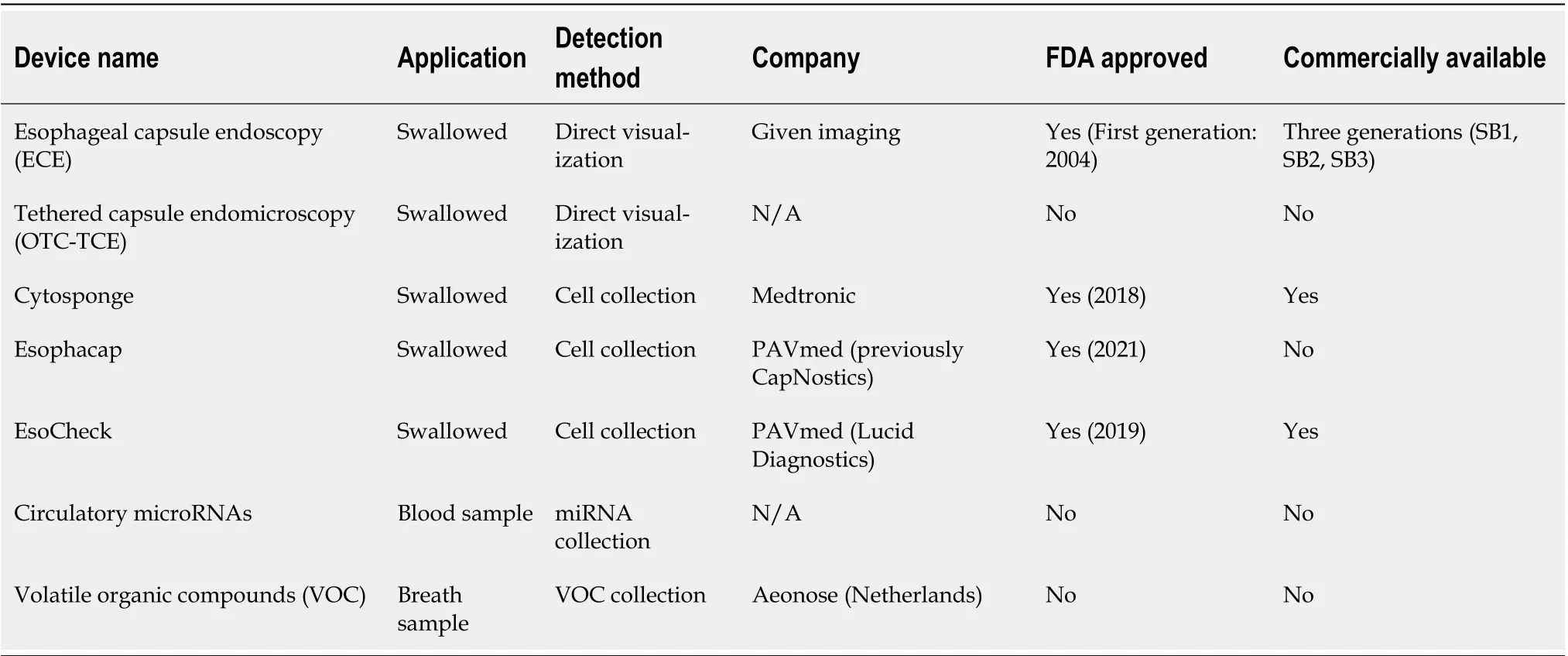
Table 1 Non-endoscopic methods for detection of Barrett’s esophagus
FOOTNOTES
Author contributions:Shahsavari D performed the majority of the writing and prepared tables, Kudaravalli P contributed to writing and prepared figures; Yap JEL provided input in writing the paper; Vega KJ designed the outline, coordinated the writing of the paper, edited the paper for intellectual content and is the guarantor.
Conflict-of-interest statement:No conflict of interest exists for any author of this manuscript.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORClD number:Dariush Shahsavari 0000-0002-4514-6973; Praneeth Kudaravalli 0000-0001-8242-8729; John Erikson L Yap 0000-0002-0441-3211; Kenneth J Vega 0000-0002-2432-6123.
Corresponding Author's Membership in Professional Societies:American Gastroenterological Association; American College of Gastroenterology; American Society for Gastrointestinal Endoscopy.
S-Editor:Chang KL
L-Editor:A
P-Editor:Chang KL
杂志排行
World Journal of Gastroenterology的其它文章
- The mechanism of Yinchenhao decoction in treating obstructivejaundice-induced liver injury based on Nrf2 signaling pathway
- Anoctamin 5 regulates the cell cycle and affects prognosis in gastric cancer
- Effects of Granule Dendrobii on chronic atrophic gastritis induced by N-methyl-N'-nitro-N-nitrosoguanidine in rats
- Machine learning predicts portal vein thrombosis after splenectomy in patients with portal hypertension: Comparative analysis of three practical models
- Sirolimus increases the anti-cancer effect of Huai Er by regulating hypoxia inducible factor-1α-mediated glycolysis in hepatocellular carcinoma
- lnternational patterns in incidence and mortality trends of pancreatic cancer in the last three decades: A joinpoint regression analysis
