高强度聚焦超声辅助腹腔镜下妊娠病灶清除术治疗Ⅲ型剖宫产瘢痕妊娠的临床效果及对患者再生育的影响
2022-05-10熊翔鹏艾小燕王爽
熊翔鹏 艾小燕 王爽


【摘要】 目的:探讨高强度聚焦超声(HIFU)輔助腹腔镜下妊娠病灶清除术治疗Ⅲ型剖宫产瘢痕妊娠(CSP)的临床效果及对患者再生育的影响。方法:选择2017年6月-2018年12月江西省妇幼保健院妇科收治的有再生育要求的Ⅲ型CSP患者120例。根据患者知情原则随机分HIFU组、子宫动脉栓塞术(UAE)组、对照组,所有患者治疗后均随访24个月,10例失访。HIFU组(n=36)采用HIFU辅助腹腔镜下妊娠物清除+瘢痕修补术,UAE组(n=38)采用UAE辅助腹腔镜下妊娠物清除+瘢痕修补术,对照组(n=36)直接行腹腔镜下妊娠物清除+瘢痕修补术。比较三组手术时间、术中失血量、住院时间、术后高温率、术后疼痛视觉模拟评分法(VAS)评分、住院费用、术后第1天人绒毛膜促性腺激素(β-hCG)下降百分比、血β-hCG恢复正常时间、月经恢复时间及再次妊娠情况。结果:三组手术时间、术中失血量、术后VAS评分、住院费用、住院时间比较,差异均有统计学意义(P<0.05);HIFU组与UAE组手术时间均短于对照组(P<0.05);HIFU组术中失血量少于UAE组与对照组,且UAE组少于对照组,差异均有统计学意义(P<0.05);HIFU组术后VAS评分及住院费用均低于UAE组,HIFU组和UAE组均高于对照组,差异均有统计学意义(P<0.05)。三组住院时间比较,差异有统计学意义(P<0.05)。术后24个月随访三组妊娠情况,三组再次妊娠率及间隔时间比较,差异均有统计学意义(P<0.05),且HIFU组与对照组均优于UAE组(P<0.05)。结论:HIFU及UAE辅助腹腔镜下妊娠病灶清除术较直接手术治疗Ⅲ型CSP手术时间更短、术中出血量更少,但HIFU辅助腹腔镜下妊娠病灶清除术在经济性方面优于UAE,且其对Ⅲ型CSP患者后续妊娠结局并无不良影响,具有更高的临床应用价值。
【关键词】 高强度聚焦超声 剖宫产瘢痕妊娠 子宫动脉栓塞术 腹腔镜
Clinical Effect of High-intensity Focused Ultrasound-assisted Laparoscopic Removal of Pregnancy Lesions in the Treatment of Type Ⅲ Cesarean Scar Pregnancy and Its Impact on Patients’ Reproduction/XIONG Xiangpeng, AI Xiaoyan, WANG Shuang. //Medical Innovation of China, 2022, 19(10): 0-072
[Abstract] Objective: To investigate the clinical effect of high-intensity focused ultrasound (HIFU)-assisted laparoscopic removal of pregnancy lesions in the treatment of type Ⅲ cesarean scar pregnancy (CSP) and its impact on patient reproductive. Method: From June 2017 to December 2018, 120 cases of type Ⅲ CSP patients with reproductive requirements who admitted to the Department of Gynecology in Jiangxi Maternal and Child Health Hospital were collected. The patients were randomly divided into HIFU group, uterine artery embolization (UAE) group and the control group according to the patient informed principle, all patients were followed up for 24 months after treatment, 10 cases were lost to follow-up. HIFU group (n=36) was given HIFU-assisted laparoscopic gestation removal and scar repair, UAE group (n=38) was given UAE-assisted laparoscopic gestation removal and scar repair, and the control group (n=36) was given laparoscopic gestation removal and scar repair. The operation time, intraoperative blood loss, hospitalization time, postoperative high temperature rate, postoperative pain visual analogue scale (VAS) score, hospitalization expenses, percentage of β-hCG decrease on the first day after surgery, and time of β-hCG return to normal, menstrual recovery time and repeated pregnancy were compared among three groups. Result: There were statistically significant differences in operative time, intraoperative blood loss, postoperative VAS score, hospitalization cost and length of stay among three groups (P<0.05); the operation times of HIFU group and UAE group were shorter than that of the control group (P<0.05); the intraoperative blood loss in HIFU group was less than those in UAE group and the control group, and UAE group was less than that in the control group, the differences were statistically significant (P<0.05); the postoperative VAS score and hospitalization cost in HIFU group were lower than those in UAE group, and HIFU group and UAE group were higher than those in the control group, the differences were statistically significant (P<0.05). There was significant difference in hospital stay among three groups (P<0.05). The pregnancies of three groups were followed up 24 months after operation, there were significant differences in the rate and interval of second pregnancy among three groups (P<0.05), HIFU group and the control group were better than those of UAE group (P<0.05). Conclusion: Compared with direct surgical treatment for type Ⅲ CSP, HIFU and UAE -assisted laparoscopic removal of pregnancy lesion has shorter operative time and less intraoperative blood loss, but HIFU-assisted laparoscopic removal of pregnancy lesions is superior to UAE in terms of economy, and has no adverse effect on the subsequent pregnancy outcome of patients with type Ⅲ CSP and higher clinical application value.
[Key words] High-intensity focused ultrasound Cesarean scar pregnancy Uterine artery embolization Laparoscopy
First-author’s address: Jiangxi Maternal and Child Health Hospital, Nanchang 330000, China
doi:10.3969/j.issn.1674-4985.2022.10.017
剖宫产瘢痕妊娠(cesarean scar pregnancy,CSP)是指受精卵着床于前次剖宫产切口瘢痕处的一种异位妊娠。根据超声提示的着床于子宫瘢痕的妊娠囊的生长方向及位置,文献[1]将CSP分为3型,其中Ⅲ型剖宫产瘢痕妊娠最为凶险,因此,早期诊断治疗以减少并发症发生和保全患者生育能力显得尤为重要。临床上通常选择行CSP病灶清除术,在清除妊娠病灶的同时,切除子宫瘢痕组织,修复薄弱的肌层,以恢复正常的解剖结构[2]。近年来,高强度聚焦超声(high-intensity focused ultrasound,HIFU)和子宫动脉栓塞术(uterine artery embolization,UAE)越来越受到妇产科医生的青睐,并将此两项技术逐步应用于Ⅲ型CSP的预处理中。因此,本研究将HIFU辅助腹腔镜下妊娠病灶清除术与其他治疗方案进行比较,探讨其治疗Ⅲ型CSP的临床效果,同时为有再生育要求的Ⅲ型CSP患者的治疗提供临床依据。现报道如下。
1 资料与方法
1.1 一般资料 收集2017年6月-2018年12月江西省妇幼保健院妇科收治的Ⅲ型CSP患者120例,均有再生育要求。CSP的诊断标准参照《剖宫产术后子宫瘢痕妊娠诊治专家共识(2016)》[1],Ⅲ型CSP:妊娠囊完全着床于子宫瘢痕处肌层并外凸向膀胱方向;妊娠囊与膀胱之间的肌层变薄甚至缺失,厚度≤3 mm;宫腔与宫颈管空虚;彩色多普勒血流显像(CDFI):瘢痕处见滋养层血流信号(低阻血流)。(1)纳入标准:①综合术前超声、MRI、术中情况及术后病理确诊为Ⅲ型CSP;②无手术相关禁忌证;③本次手术后2年内能定期接受随访。(2)排除标准:①有严重肝、肾疾病;②有腹腔出血伴重度出血性休克;③有嚴重糖尿病、高血压等基础疾病;④在此之前接受其他治疗。根据患者知情原则随机分三组,每组40例,所有患者治疗后均随访24个月,10例失访,最终HIFU组36例、UAE组38例、对照组36例。本研究已经医院伦理学委员会批准,患者及家属均知情同意并签署知情同意书。
1.2 方法 所有手术由具有丰富手术经验的资深妇科医生完成。对照组直接行腹腔镜下妊娠物清除+瘢痕修补术,HIFU组采用HIFU辅助腹腔镜下妊娠物清除+瘢痕修补术,UAE组采用UAE辅助腹腔镜下妊娠物清除+瘢痕修补术。
1.2.1 对照组 患者取膀胱截石位,全麻后置入腹腔镜,采用简易举宫器经阴道举宫,暴露子宫下段,切开膀胱反折腹膜,下推膀胱,取肌层最薄处切开,清除绒毛蜕膜组织及血块。修剪瘢痕周围薄弱肌层,连续缝合创面。
1.2.2 HIFU组 选用重庆海扶医疗科技股份有限公司的聚焦超声肿瘤治疗设备。HIFU治疗在镇痛镇静下进行,患者取俯卧位,定点辐照胚囊着床部位,治疗功率300~400 W,层间距3~5层,治疗后病灶出现整体灰度。HIFU消融后24 h行腹腔镜下妊娠物清除及瘢痕修补术,步骤同对照组。
1.2.3 UAE组 患者取仰卧位,常规局麻后行股动脉置管。采用子宫动脉血管造影定位子宫瘢痕妊娠部位供血动脉,用可吸收性明胶海绵阻断双侧子宫动脉,治疗后血管造影显示子宫动脉闭塞。UAE后24 h行腹腔镜下妊娠物清除及瘢痕修补术,步骤对照组。
1.3 观察指标 比较三组手术时间、术中失血量、住院时间、术后高温发生情况(手术24 h后持续3次间隔3 h患者体温≥38.1 ℃,无感染证据)、术后疼痛视觉模拟评分法(VAS)评分、术后第1天β-hCG下降百分比、住院费用及围手术期并发症(盆腹腔脏器损伤、肠梗阻、肺栓塞、血栓、发热、疼痛、腹胀等)。术后1 d抽血查β-hCG,以后每周1次复查至正常。术后3、24个月进行随访,包括血清β-hCG恢复正常时间、月经恢复时间及再次妊娠情况。
1.4 统计学处理 采用SPSS 22.0软件对所得数据进行统计分析,符合正态分布的计量资料用(x±s)表示,采用完全随机样本方差分析进行比较,通过q检验进行两两比较;非正态分布计量资料中位数(四分位间距)表示,采用Kruskal-Wallis秩和检验进行比较,采用Nemenyi法进行两两比较。计数资料以率(%)表示,比较采用字2检验,通过Bonferroni法进行两两比较。以P<0.05为差异有统计学意义。
2 结果
2.1 三组术前临床资料比较 三组术前临床资料比较,差异均无统计学意义(P>0.05),具有可比性,见表1。
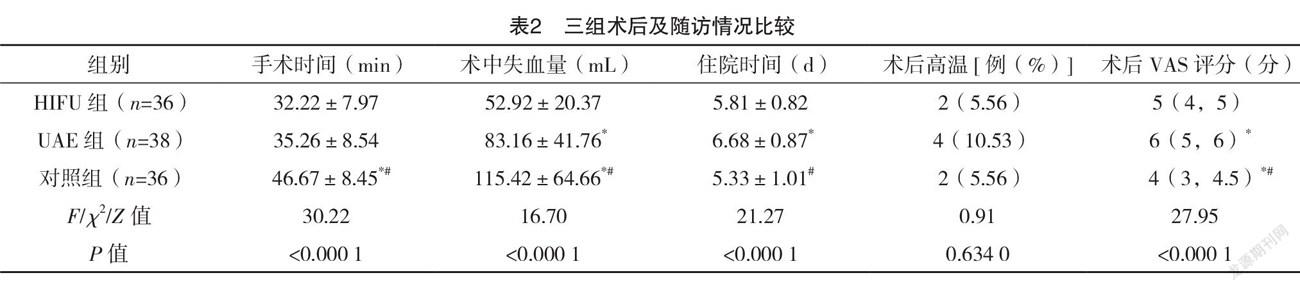
2.2 三组手术时间、术中失血量、住院时间、术后高温率、术后VAS评分、术后第1天β-hCG下降百分比、住院费用、血β-hCG恢复正常时间、月经恢复时间比较及围手术期并发症情况 三组手术时间、术中失血量、术后VAS评分、住院费用比较,差异均有统计学意义(P<0.05);HIFU组与UAE组手术时间均短于对照组(P<0.05);HIFU组术中失血量均少于UAE组与对照组,且UAE组少于对照组,差异均有统计学意义(P<0.05);HIFU组术后VAS评分及住院费用低于UAE组,均高于对照组,差异均有统计学意义(P<0.05)。三组术后高温率、术后第1天β-hCG下降百分比及月经恢复所需时间比较,差异均无统计学意义(P>0.05)。三组术后血β-hCG恢复正常时间比较,差异有统计学意义(P<0.05),其中UAE组短于对照组(P<0.05),但与HIFU组比较,差异无统计学意义(P>0.05)。此外,三组住院时间比较,差异有统计学意义(P<0.05),HIFU组与对照组相比,差异无统计学意义(P>0.05)。见表2。三组均未发生肺栓塞、血栓等严重并发症。HIFU组患者不良反应多为疼痛;UAE组患者不良反应主要表现为发热、疼痛,其中1例患者出现术后月经复潮时间明显延迟且经量减少;对照组患者主要表现腹胀,予对症治疗后均好转。
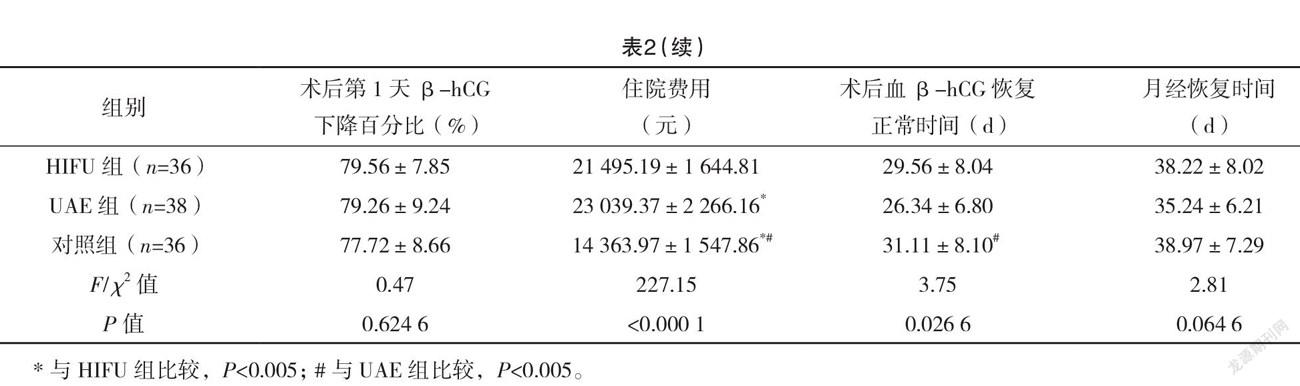
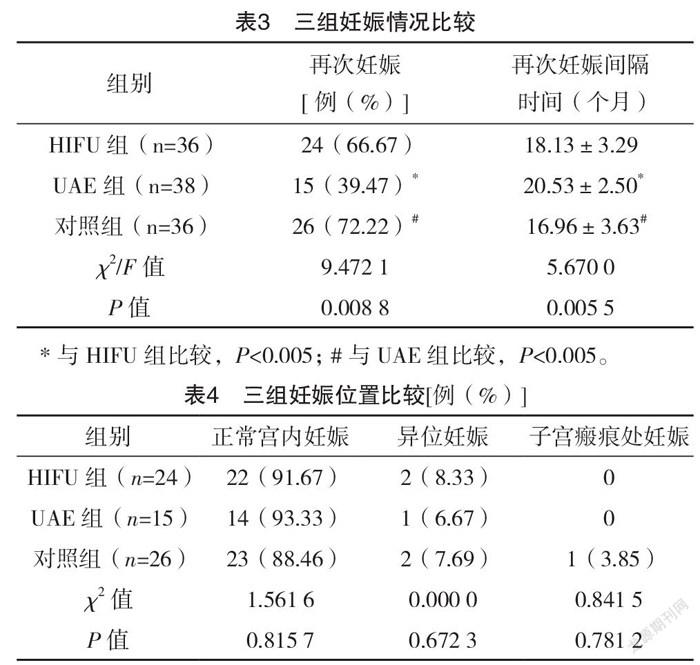
2.3 三组妊娠情况比较 术后24个月随访三组妊娠情况,三组再次妊娠率及间隔时间比较,差异均有统计学意义(P<0.05),HIFU组与对照组均优于UAE组(P<0.05),HIFU组与对照组比较,差异均无统计学意义(P>0.05),见表3。三组正常宫内妊娠、异位妊娠、子宫瘢痕处妊娠情况比较,差异均无统计学意义(P>0.05),见表4。
3 讨论
近年来随着剖宫产数量增多,CSP的发病率也逐渐增高[3-4]。目前CSP的发病机制尚不清楚,国内外CSP的诊治方案均无统一指南。其治疗方案包括药物保守治疗、UAE治疗、HIFU治疗、手术治疗或联合治疗等[5]。治疗方案的选择取决于孕囊大小、着床位置及β-hCG水平等因素[6]。其中,Ⅲ型CSP最为凶险,其子宫瘢痕处肌层菲薄,甚至可能穿透浆膜层,早期即可导致子宫破裂,出现难以控制的大出血,直接清宫或单纯宫腔镜手术的风险极大,因此临床上多选择腹腔镜下妊娠物清除+瘢痕修补治疗,另外,此术式尤其适用于有再生育要求的患者,其可在清除妊娠病灶的同时修补子宫瘢痕缺损,恢复正常的解剖结构。同时,为减少术中术后出血量、增加手术安全性,在临床上可采用HIFU、UAE等治疗进行预处理。
近年来,UAE辅助治疗CSP常用于临床[7-8]。在治疗CSP的过程中,UAE通过栓塞子宫动脉阻断子宫的主要血供以减少出血量,同时减少血供导致胚胎缺血性坏死,以减少胚胎脱落或进一步手术治疗时的出血,进而提高手术安全性[9]。Huang等[10]分析了31例接受UAE治疗的CSP患者,在UAE术后24~48 h行清宫术,发现术中失血量仅为2~20 mL。Qiu等[11]对62例接受UAE治疗的CSP患者行宫腔镜下清宫术,手术成功率高达95.7%。但是,UAE虽然能通过暂时阻断子宫灌注进而控制CSP出血,却并不能缩小CSP病灶[12],另外,其出现手术并发症的风险较大,包括盆腔感染、栓塞、子宫大面积坏死等,尤其是对卵巢功能及生育能力的影响[13]。
HIFU是使用精确聚焦的超声能量来治疗疾病的非侵入性辅助治疗技术,其疗效已经在子宫腺肌病和子宫肌瘤等妇科良性疾病的治疗上得到广泛验证,近些年也被用于CSP輔助治疗中[14-16]。HIFU治疗CSP的机制是将高强度的超声能量聚焦于孕囊及周边的滋养血管,通过瞬间产生高温,使局部出现凝固性坏死,导致血管内膜出现坏死,内皮细胞脱落,暴露血管弹性膜,进而激活内外源性凝血机制,最终导致血流动力学改变,以减少治疗过程中的出血量[17]。此外,CSP患者在HIFU治疗后行彩色多普勒超声检查发现,胎儿心脏活动消失,血流消失,CSP病灶明显减小[18]。因此,HIFU辅助治疗既有预防CSP出血的作用,又能缩小CSP病灶。此外,其对保全患者子宫、保留生育功能及提升生活质量具有重要意义[19]。Zhang等[20]通过回顾性分析154例CSP患者行HIFU联合B超下负吸术治疗的资料后发现,有再生育要求的患者妊娠率高达82.14%。
本研究结果显示,UAE及HIFU辅助腹腔镜下妊娠物清除+瘢痕修补术治疗Ⅲ型CSP,UAE组、HIFU组术中出血量均明显少于对照组(P<0.05)。表明两种预处理方法均能有效减少术中出血量。而在两种方法中HIFU组不仅术中失血量最少,且手术时间最短,虽然HIFU组与UAE组手术时间无明显统计学差异,这可能是由于样本量不足导致的。此外,HIFU组术后病率、术后第1天β-hCG下降百分比及月经恢复所需时间与另外两组无明显差异,但其术后VAS评分及住院费用均明显低于UAE组,说明HIFU组与UAE组相比,住院成本更低,患者术后生存质量更高。另外,三组均未发生肺栓塞、血栓等严重并发症。本研究中HIFU组患者不良反应多为疼痛,予对症治疗后均好转,但UAE组患者中出现疼痛及发热症状的患者更多,且有患者出现术后月经复潮时间明显延迟且经量减少,这可能是由于UAE栓塞子宫动脉,使子宫血供不足,子宫内膜缺血损伤所致。进一步随访中发现,HIFU组再次妊娠率及间隔时间均明显优于UAE组,但与对照组无明显差异,表明HIFU预处理后行腹腔镜下妊娠物清除+瘢痕修补术治疗有利于保留患者的生育能力,这可能得益于HIFU的精准聚焦,其除作用于妊娠病灶外,对周围正常组织损伤小,副作用亦小。在Xiao等[19]的研究中也已证实HIFU治疗具有保留子宫生育功能的优点,其对有再生育要求的Ⅲ型CSP患者和家庭具有重要意义。此外,再次妊娠的患者中,仅对照组再次出现剖宫产瘢痕处妊娠,但因标本量较小,差异无统计学意义。
综上所述,HIFU及UAE辅助腹腔镜下妊娠病灶清除术较直接手术治疗Ⅲ型CSP手术时间更短、术中失血量更少,但HIFU辅助腹腔镜下妊娠病灶清除术在经济性方面优于UAE,且其对Ⅲ型CSP患者后续妊娠结局并无不良影响,具有更高的临床应用价值。
参考文献
[1]中华医学会妇产科分会计划生育学组.剖宫产术后子宫瘢痕妊娠诊治专家共识[J].中华妇产科杂志,2016,51(8):568-572.
[2] QIAO B,ZHANG Z,LI Y.Uterine artery embolization versus methotrexate for cesarean scar pregnancy in a Chinese population:Ameta-analysis[J].J Minim Invasive Gynecol,2016,23(7):1040-1048.
[3] ZAHÁLKOVÁ L,KACEROVSKÝ M.Cesarean scar ectopic pregnancy[J].Ceska Gynekol[J].Winter,2016,81(6):414-419.
[4] LATA K,DAVIS A A,PANWAR A,et al.Laparoscopic Excision of Cesarean Scar Ectopic Pregnancy[J].J Obstet Gynaecol India,2020,70(5):397-401.
[5] HUDEČEK R,FELSINGEROVÁ Z,FELSINGER M,et al.
Laparoscopic Treatment of Cesarean Scar Ectopic Pregnancy[J].J Gynecol Surg,2014,30(5):309-311.
[6] DOROSZEWSKA K,MILEWICZ T,BEREZA T,et al.Cesarean scar pregnancy-various methods of treatment[J].Folia Med Cracov,2019,59(2):5-14.
[7] FU LI-PING.Therapeutic approach for the cesarean scar pregnancyc[J/OL].Medicine(Baltimore),2018,97(18):e0476.
[8] SINGHAL S,SINGH A,RAGHUNANDAN C,et al.Uterine artery embolization:Exploring new dimensions in obstetric emergencies[J].Oman Med J,2014,29(3):217-219.
[9] YANG X Y,YU H,LI K M,et al.Uterine artery embolisation combined with local methotrexate for treatment of caesarean scar pregnancy[J].BJOG,2010,117(8):990-996.
[10] HUANG Y,LI Y,XI R,et al.An application of uterine artery chemoembolization in treating cesarean scar pregnancy[J].Int J Clin Exp Med,2015,8(2):2570-2577.
[11] QIU J,FU Y,XU J,et al.Analysis on clinical effects of dilation and curettage guided by ultrasonography versus hysteroscopy after uterine artery embolization in the treatment of cesarean scar pregnancy[J].Ther Clin Risk Manag,2019,15(1):83-89.
[12] LIU J,CHAI Y,YU Y,et al.The value of 3-dimensional color Doppler in predicting intraoperative hemorrhage for cesarean scar pregnancy[J/OL].Medicine(Baltimore),2018,97(33):e11969.
[13]孫俊杰,郭素杰.子宫动脉栓塞术介入治疗剖宫产切口瘢痕妊娠的研究进展[J].医学综述,2019,25(13):2632-2637.
[14] VERPALEN INEZ M,DE BOER JOLIEN P,LINSTRA MARLOT,et al.The Focused Ultrasound Myoma Outcome Study(FUMOS);a retrospective cohort study on long-term outcomes of MR-HIFU therapy[J].Eur Radiol,2020,30(5):2473-2482.
[15] QING G,FENG X,ZHENZHEN D,et al.High intensity focused ultrasound treatment of adenomyosis:a comparative study[J].Int J Hyperthermia,2018,35(1):505-509.
[16] JUHUA X,ZHEN S,JINSHUI Z,et al.Cesarean Scar Pregnancy:Comparing the Efficacy and Tolerability of Treatment with High-Intensity Focused Ultrasound and Uterine Artery Embolization[J].Ultrasound Med Biol,2017,43(3):640-647.
[17] ORSI F,ARNONE P,CHEN W,et al.High intensity focused ultra-sound ablation:a new therapeutic option for solid tumors[J].J Cancer Res Ther,2010,6(4):414-420.
[18] ZHU X,DENG X,WAN Y,et al.High-intensity focused ultrasound combined with suction curettage for the treatment of cesarean scar pregnancy[J/OL].Medicine(Baltimore),2015,94(18):e854.
[19] XIAO J,SHI Z,ZHOU J,et al.Cesarean scar pregnancy:comparing the efficacy and tolerability of treatment with high-intensity focused ultrasound and uterine artery embolization[J].Ultrasound Med Biol,2017,4(3):640-647.
[20] ZHANG C,ZHANG Y,HE J,et al.Outcomes of subsequent pregnancies in patients following treatment of cesarean scar pregnancy with high intensity focused ultrasound followed by ultrasound-guided dilation and curettage[J].Int J Hyperthermia,2019,36(1):926-931.
(收稿日期:2021-09-28) (本文编辑:程旭然)
