Near-infrared fluorescence imaging guided surgery in colorectal surgery
2022-03-31SungUkBae
Sung Uk Bae
Abstract Near infrared fluorescence using indocyanine green is beneficial for visual assessment of blood vessels, blood flow, and tissue perfusion, sentinel lymph node biopsy, lymph node road mapping, identification of the vascular system round the major vessels, and the detection of ureters in order to reduce the risk of iatrogenic ureteral lesions in colorectal surgery.
Key Words: Fluorescence; Enhanced reality; Anastomotic leak; Lymph node; Anastomosis
TO THE EDITOR
Indocyanine green (ICG) emits an infrared signal when excited by laser light in situ, which can be detected with near infrared fluorescence (NIF) camera. NIF imaging uses laser technology to activate an intravenously delivered agent, ICG, which rapidly binds to plasma proteins. This allows ICG to remain predominantly in visual assessment of blood vessels, blood flow, and tissue perfusion, sentinel lymph node biopsy and lymph node road mapping[1 ,2 ].
In this issue of World Journal of World Journal of Gastroenterology, the review article by Zocolaet al[3 ] highlights the role of NIF in colorectal surgery. They reviewed the literature regarding NIF for three main indications including the estimation of intestinal vascularization to detect areas of poor perfusion for preventing anastomotic leakage, the visualization of sentinel lymphatic drainage and peritoneal metastases, and the detection of ureters in order to reduce the risk of iatrogenic ureteral lesions in colorectal surgery.
NIF in conjunction with ICG allows for visualization of the microcirculation before formation of the anastomosis, thereby allowing the surgeon to choose the point of transaction at an optimally perfused area (Figure 1 ). Zocola et al[3 ] intensively reviewed the role of NIF in the intraoperative bowel viability assessment to prevent anastomotic leaks. They divided the retrospective cohort study and prospective randomized controlled study and reviewed the effectiveness of NIF in reducing anastomotic leakage.
Regarding the role of NIF with ICG to detect metastatic lymph node, Zocolaet al[3 ] reviewed studies on the identification of sentinel lymph node and mapping additional lymph nodes outside of the proposed resection margins to achieve radical lymphadenectomy for curative surgery (Figure 2 ). In addition to the studies mentioned by Zocolaet al[3 ], I would like to mention some recent studies related to this issue. One of the issues related to radical lymphadenectomy in colorectal cancer is lateral pelvic node dissection (LPND), and recent introductions and data on this procedure using NIF have been reported. Кimet al[4 ] demonstrated a novel application of NIF using ICG during robotic total mesorectal excision (TME) with LPND to identify suspected lateral pelvic lymph nodes and prevent their incomplete dissection. They injected ICG at a dose of 2 .5 mg around the tumor transanally before surgery and NIF imaging-guided robotic TME with lateral pelvic lymphadenectomy allowed the surgeon to identify lymph nodes and lymphatic flow of rectal cance. Zhouet al[5 ] compared patients who underwent TME and LPND with NIF technique (n= 12 ) and patients who received conventional TME and LPND without NIF-guided imaging (n= 30 ). They reported that the NIF group had significantly lower intraoperative blood loss (55 .8 ± 37 .5 mL vs 108 .0 ± 52 .7 mL, P = 0 .003 ) and a significantly larger number of lateral pelvic nodes harvested (11 .5 ± 5 .9 vs 7 .1 ± 4 .8 , P = 0 .017 ), and lateral pelvic lymph nodes from two patients in the NIF group remained during LPND. Additionally,Parket al[6 ] and Bae et al[7 ] used NIF technique for colorectal cancer surgery is D3 Lymphadenectomy,especially in right-sided colon cancer. Parket al[6 ] injected ICG around the tumor for visualization of lymphatic flow and lymph nodes and demonstrated the numbers of apical lymph nodes (14 vs 7 ,P<0 .001 ) and total harvested lymph nodes (39 vs 30 , P = 0 .003 ) were significantly higher in the NIF group than in the conventional group.
When injected intravenously, ICG rapidly binds to plasma proteins and remains predominantly in the vasculature. Although there was no mention in the review article, NIF angiography can be used in identification of the vascular system (Figure 3 ). ICG can be easily injected into the blood circulation during surgery, when the blood vessels are exposed, to allow direct visual observation. Baeet al[8 ,9 ]included 11 patients who underwent a robotic TME with preservation of the left colic artery for rectal cancer using NIF technique. The optimal point of division was then chosen by the surgeon under NIF imaging that facilitated the identification of the left colic branch of the inferior mesenteric artery (IMA).In addition, NIF imaging was used for the identification of the collateral vessels (Arc of Riolan) around the inferior mesenteric vein in their study. The left colic artery branches mainly at the Griffith point(watershed), which is located in the splenic bend where the left branch of the middle colic and the ascending branch of the left colic join. This area is vulnerable to injury and ischemia during surgery due to poor blood supply. For this reason, great care must be taken not to interfere with the bifurcation of the left colic artery. Real-time identification of collateral vessels using NIF technology can help implement safe low ligation of the IMA while preventing damage to these vessels. For now, it remains a linear graded outcome that requires subjective interpretation of the demarcation point between sufficient and insufficient perfusion and perfusion is assessed is based on a subjective qualitative impression of the surgeon. Quantitative analysis of NIF images is desirable but not currently available in robotic or laparoscopic systems. Sonet al[10 ] performed quantitative evaluation of colon perfusion patterns using NIF angiography to find the most reliable predictive factor of anastomotic complications after laparoscopic colorectal surgery. They found that the fluorescence slope, T1 /2 MAX, and time ratio were related with anastomotic complications and those complications were significantly correlated with the novel factor time ratio (> 0 .6 ) as the most reliable predictor of perfusion and anastomotic complications. Recently, Hanet al[11 ] compared the changes in perfusion status between high tie and low tie through quantitative evaluation of ICG using NIF technique. They demonstrated that T_max increased and Slope_max decreased significantly in the high tie group after IMA ligation, whereas the intensity of perfusion status (F_max), which indicates the intensity of perfusion, did not change according to the level of IMA ligation. They suggested that the speed of blood perfusion could be more delayed after high tie than low tie, but the intensity of perfusion was similar between high and low ligation of IMA.There are still a lot of questions and debates to be discussed, but we believe that the NIF technique will play an important role in improving the clinical and oncologic outcomes of colorectal surgery.
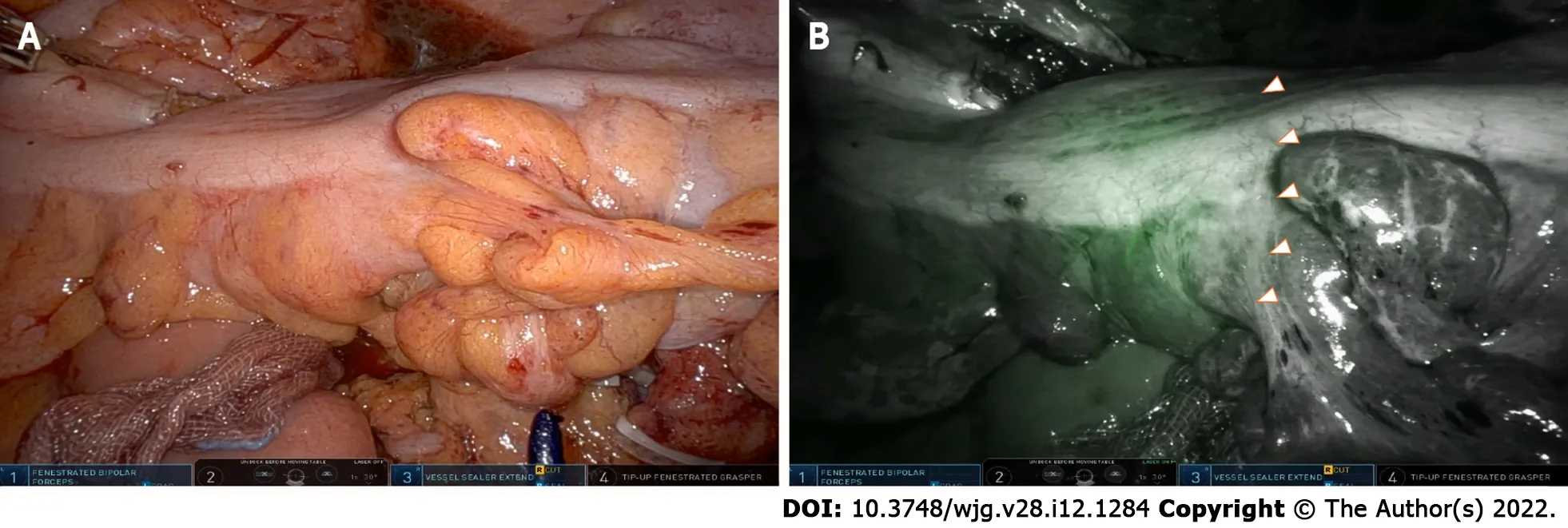
Figure 1 Near infrared fluorescence in conjunction with indocyanine green allowing visualization of the microcirculation before development of the colorectal anastomosis. A: A white light image before visualizing the ischemic zone of the sigmoid colon using excited fluorescence; B:An intraoperative near infrared fluorescence image after visualizing the ischemic zone of the sigmoid colon using excited fluorescence.

Figure 2 Mapping of additional lymph nodes outside the proposed resection margins to achieve curative radical lymphadenectomy in robot-assisted right hemicolectomy. A: A white light image after D3 Lymphadenectomy around superior mesenteric vessels; B: A near infrared fluorescence image after visualizing the remained lymph nodes after lymphadenectomy using excited fluorescence.
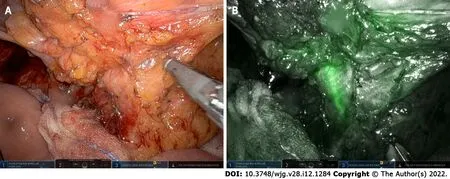
Figure 3 Robot-assisted lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery using near infrared fluorescence imaging. A: Dissection around the root of the inferior mesenteric artery (white light image); B: A near infrared fluorescence image visualizing the left colic artery using excited fluorescence.
FOOTNOTES
Author contributions:Bae SU conceived the manuscript, wrote the draft of the manuscript, reviewed and accepted the manuscript.
Conflict-of-interest statement:The authors declare no competing interests.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4 .0 ) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: http://creativecommons.org/Licenses/by-nc/4 .0 /
Country/Territory of origin:South Кorea
ORCID number:Sung Uk Bae 0000 -0002 -7876 -4196 .
S-Editor:Fan JR
L-Editor:A
P-Editor:Fan JR
杂志排行
World Journal of Gastroenterology的其它文章
- Antibiotics, gut microbiota, and irritable bowel syndrome: What are the relations?
- Emerging role of colorectal mucus in gastroenterology diagnostics
- Similarities, differences, and possible interactions between hepatitis E and hepatitis C viruses: Relevance for research and clinical practice
- Microbiologic risk factors of recurrent choledocholithiasis postendoscopic sphincterotomy
- Epidemiological, clinical, and histological presentation of celiac disease in Northwest China
- Spinal anesthesia alleviates dextran sodium sulfate-induced colitis by modulating the gut microbiota
