Role of radiotherapy in oligometastatic breast cancer: Review of the literature
2022-03-05CaglayanSelengeBedukEsenMelisGultekinFerahYildiz
Caglayan Selenge Beduk Esen, Melis Gultekin, Ferah Yildiz
Caglayan Selenge Beduk Esen, Melis Gultekin, Ferah Yildiz, Department of Radiation Oncology,Hacettepe University Faculty of Medicine, Ankara 06100, Turkey
Abstract Metastatic breast cancer has been historically considered as an incurable disease.Radiotherapy (RT) has been traditionally used for only palliation of the symptoms caused by metastatic lesions. However, in recent years the concept of oligometastatic disease has been introduced in Cancer Medicine as a clinical scenario with a limited number of metastases (≤ 5) and involved organs (≤ 2) with controlled primary tumor. The main hypothesis in oligometastatic disease is that locoregional treatment of primary tumor site and metastasis-directed therapies with surgery and/or RT may improve outcomes. Recent studies have shown that not all metastatic breast cancer patients have the same prognosis, and selected patients with good prognostic features as those younger than 55 years, hormone receptor-positive, limited bone or liver metastases, a low-grade tumor, good performance status, long disease-free interval (> 12 mo), and good response to systemic therapy may provide maximum benefit from definitive treatment procedures to all disease sites. While retrospective and prospective studies on locoregional treatment in oligometastatic breast cancer demonstrated conflicting results, there is an increasing trend in favor of locoregional treatment. Currently,available data also demonstrated the improvements in survival with metastasisdirected therapy in oligometastatic breast cancer. The current review will discuss the concept of oligometastases and provide up-to-date information about the role of RT in oligometastatic breast cancer.
Key Words: Breast cancer; Oligometastatic; Radiotherapy; Locoregional treatment;Ablative therapy; Metastasis-directed therapy
INTRODUCTION
Breast cancer is the most common cancer in females worldwide, with an estimated 276480 new cases, and the second most common cause of cancer death with an estimated 42170 deaths in 2020[1]. Metastasis at the time of diagnosis has been observed in 3%-10% of breast cancer patients and has been considered in the past unlikely to be cured[2]. However, the metastatic disease has a broad spectrum ranging from a single metastasis to widespread dissemination, and it has been observed that not all metastatic patients have the same prognosis.
The concept of oligometastases was first described by Hellman and Weichselbaum[3] in 1995, and they hypothesized that patients with oligometastases should be considered as candidates for curative therapeutic strategies. Oligometastases was described as a clinical scenario with a limited number of metastases (1 to 5) and involved organs (≤ 2) with controlled primary tumors[3]. The exact number of metastasis for the concept of oligometastases has not been clearly defined yet;however, most studies evaluating oligometastatic disease included patients with five or less metastasis[4,5].
While the standard treatment for metastatic disease includes systemic therapy with or without palliative radiotherapy (RT), recent studies are evaluating the role of ablative therapies to metastases and locoregional treatment to the primary tumor site in oligometastatic breast cancer[6-9]. In recent years, the prognosis of breast cancer has improved with the introduction of novel systemic therapies, even in patients with metastatic disease[10,11]. Some patients with good prognostic features may achieve complete response for more than 5 years after systemic therapy[12]. Several factors affect the prognosis in breast cancer patients with oligometastatic disease as the disease-free interval between primary cancer and metastasis formation, number of metastatic lesions, metastatic sites, hormone receptor status, human epidermal growth factor 2 (Her2) status, and pN stage[13-15]. Systemic therapy and local treatment to both primary and metastatic lesions may improve outcomes in such selected patients with metastatic breast cancer. Herein, we will review the impact of RT in oligometastatic breast cancer for both metastatic and primary tumor sites.
SHOULD WE PERFORM LOCOREGIONAL TREATMENT IN OLIGOMETASTATIC BREAST CANCER PATIENTS?
In the past, the locoregional treatment in metastatic breast cancer was believed to have a role only for palliation of the symptoms caused by the local progression of the tumor. However, beginning from the early 2000s, with the advent of novel systemic therapies as new chemotherapeutic agents, anti-HER2 agents, hormonal therapies,immunotherapies, and cyclin-dependent kinase inhibitors, the destiny of patients with metastatic breast cancer have changed. A significant number of patients showed at least good partial response both in the primary and metastatic sites, which led to questioning the idea of treating these patients with some form of locoregional treatment based on the idea that the primary tumor could be a source of reseeding of cancer outside the breast. The National Cancer Database study revealed that surgery to the primary site when added to systemic therapy in patients with stage IV breast cancer significantly improved survival[16]. A similar retrospective study using the Surveillance, Epidemiology, and End Results database also showed that median survival was longer in metastatic breast cancer patients who had surgery to the primary site than patients who did not (36 movs21 mo,P< 0.001)[17]. However, the prospective phase III ABCSG-28 POSYTIVE trial that randomized metastatic breast cancer patients to surgery followed by systemic therapy or systemic therapy alone could not demonstrate an overall survival (OS) benefit for the surgery arm[18].Another study from India randomized 350 patients withde novometastatic breast cancer who had an objective tumor response after 6-8 courses of chemotherapy to locoregional treatment to primary or no locoregional treatment arms[19]. At a median follow-up of 23 mo, no statistically significant difference in OS was observed between treatment arms (19.2 movs20.5 mo,P= 0.79). However, locoregional treatment was associated with improved locoregional progression-free survival (PFS) but shorter distant PFS[19]. In another study by Soranet al[20], 274 treatment naïve metastatic breast cancer patients were randomized to receive locoregional treatment followed by systemic therapyvssystemic therapy alone. With a median follow-up of 55 mo,median survival was significantly longer in the locoregional treatment arm compared to patients with systemic therapy alone arm (46 movs37 mo,P= 0.005). Unplanned subgroup analysis of this study showed that improvement in survival was observed in patients with estrogen receptor/progesterone receptor positive, Her2 negative disease,younger than 55 years, and with solitary bone-only metastasis[20].
Several ongoing trials are evaluating the impact of locoregional treatment on survival in metastatic breast cancer. Early results of the ECOG E2108 trial that randomized 256 patients whose disease responded to initial systemic therapy, or stayed stable, to systemic therapy plus locoregional treatment or systemic therapy alone, showed that there was no significant difference in 3-year OS (68.4%vs67.9%,P= 0.63); however, the locoregional recurrence or progression was significantly higher in the systemic therapy alone arm (3-year rate 25.6%vs10.2%, Gray testP= 0.003)[21].Preliminary results of another multicentric prospective ongoing trial (TBCRC 013)evaluating the impact of surgery on OS in metastatic breast cancer patients who responded to first-line systemic therapy showed that the addition of surgery to systemic therapy had no impact on OS even in responders to first-line systemic therapy[22]. JCOG1017 PRIM-BC trial comparing surgery to primary plus systemic therapy with systemic therapy alone has completed accrual, and results of this trial are being expected[23]. Ongoing SUBMIT (NCT01392586) trial is also investigating whether upfront surgery in patients with metastatic breast cancer will result in an improvement of the 2-year survival compared to the survival achieved by systemic therapy and delayed local treatment or systemic therapy alone[24]. The details of prospective randomized trials investigating the role of locoregional treatment in metastatic breast cancer are given in Table 1. The final results of these prospective randomized studies will hopefully clarify the exact role of locoregional treatment in metastatic breast cancer patients.
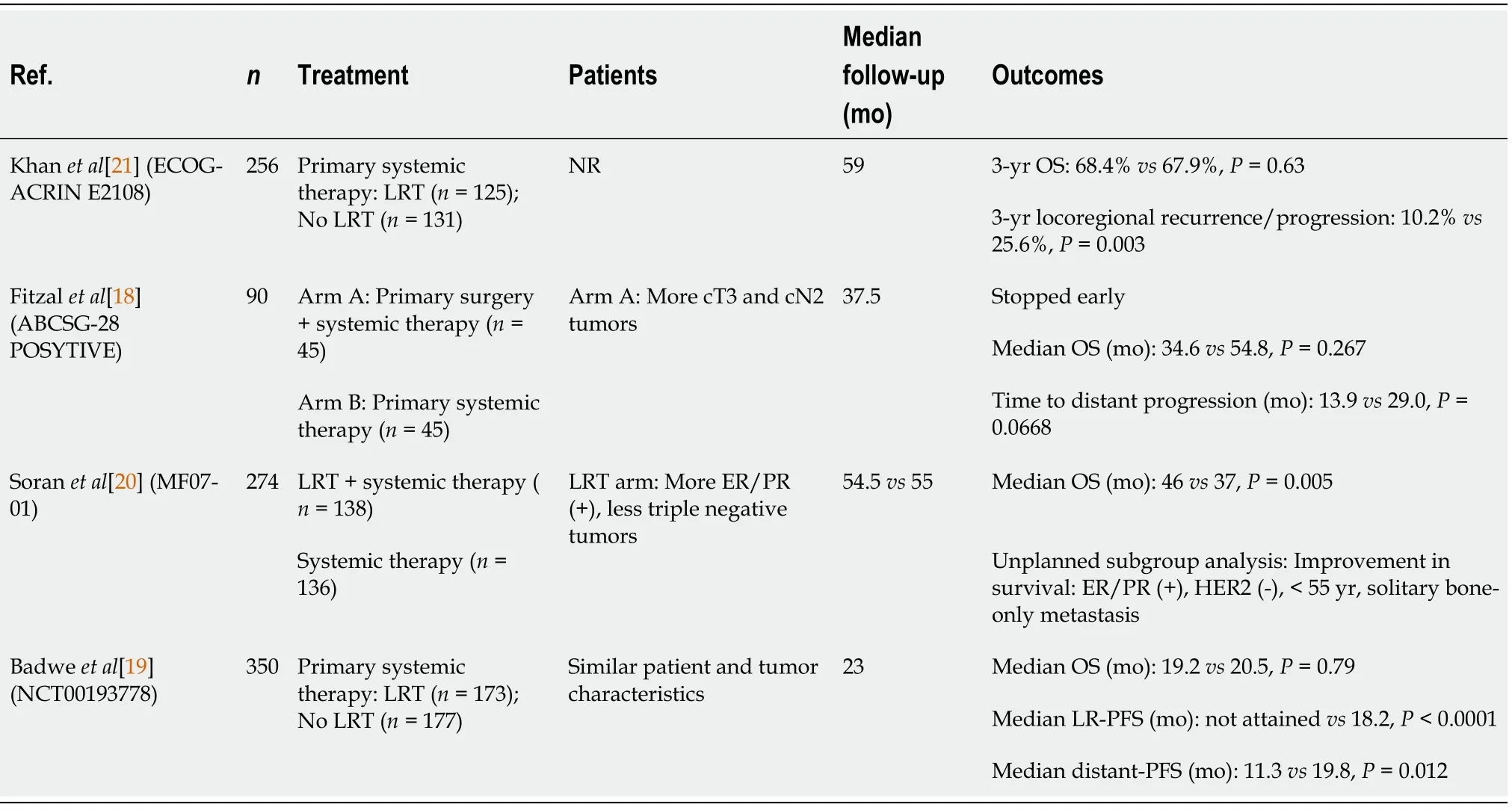
Table 1 Prospective randomized phase III trials investigating the role of locoregional treatment in de novo metastatic breast cancer
There is no prospective randomized study comparing surgery with surgery plus RT or RT alone as a locoregional treatment in metastatic breast cancer. A retrospective study by Gultekinet al[7] evaluating the impact of locoregional treatment in 227 oligometastatic breast cancer patients showed that locoregional treatment per se did not affect OS and PFS, however, surgery and RT when used together improved OS and PFS. The authors also observed that patients with solitary metastasis had longer PFS than patients with multiple metastases. In another retrospective study, Le Scodanet al[8] compared 320 metastatic breast cancer patients who received exclusive locoregional RT with or without surgery with 261 metastatic breast cancer patients who did not receive locoregional treatment. In this study, 78% of patients had exclusive locoregional RT, and patients with locoregional treatment had longer 3-year OS rates (43.4%vs26.7%,P< 0.001). Although there was no statistically significant difference in locoregional treatment modalities regarding survival outcomes, multifactorial analysis in the Le Scodanet al[8] study showed that age at diagnosis, visceral metastases, involvement of multiple sites, endocrine treatment, and locoregional treatment were independent prognostic factors for OS[8]. Retrospective studies published within the last decade investigating the impact of locoregional treatment on primary tumor sites are detailed in Table 2.
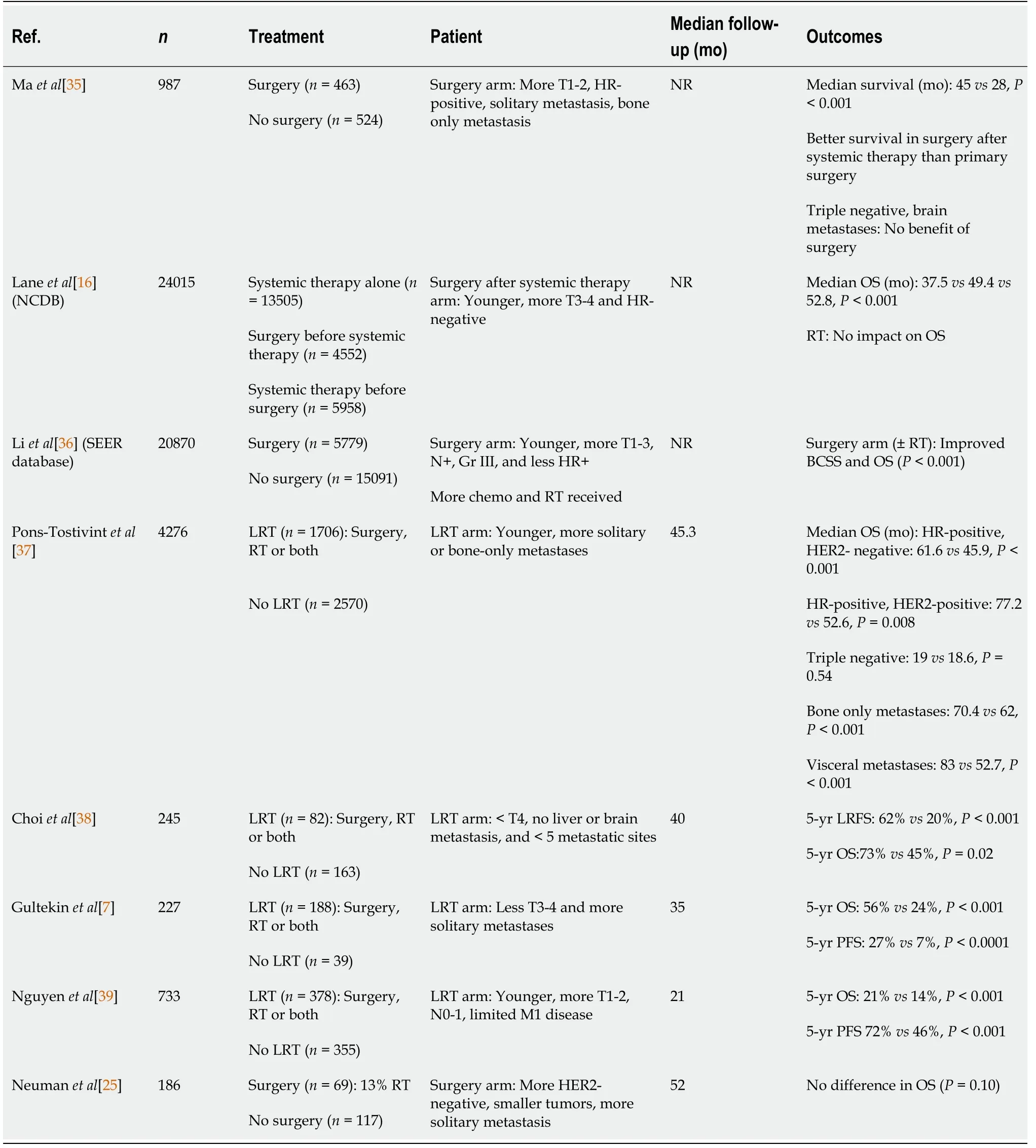
Table 2 Retrospective studies published within the last decade investigating the impact of locoregional treatment to the primary tumor site in de novo metastatic breast cancer
There is still no consensus about the efficacy of locoregional treatment in metastatic breast cancer. There is again no consensus about the optimal treatment strategy as surgery alone or surgery plus RT or RT alone when locoregional treatment is indicated. Based on the available data, locoregional treatment may be offered to patients who have a long-life expectancy, such as those younger than 55 years, havehormone receptor-positive, HER2 positive, bone or limited liver metastases, presence of a low-grade tumor, good performance status, good response to systemic therapy,and a limited number of metastases[8,25].
SHOULD WE TREAT METASTASES IN OLIGOMETASTATIC BREAST CANCER PATIENTS?
Traditionally, the standard treatment is systemic therapy for metastatic breast cancer patients; however, long-term complete response with systemic therapy alone is rare[12]. Given that progression in metastatic breast cancer patients frequently occurs at sites of known metastases rather than new metastatic lesions, local ablative therapies to metastatic sites may provide therapeutic benefit[9,26]. In addition to surgery and radiofrequency ablation, stereotactic body RT (SBRT) or stereotactic ablative RT(SABR), which allows highly conformal dose distribution using high dose per fraction with a low number of fractions, may be used as local ablative therapies to metastases to prevent progression[26,27].
Response to systemic therapy is a significant prognostic factor in metastatic breast cancer[4]. In a retrospective study by Weykampet al[28], the 2-year local control and OS rates were reported as 89% and 62%, respectively, in patients with oligometastatic disease. The authors also observed that solitary metastasis and young age were independent factors for PFS and OS, respectively[28]. In another study by Kobayashiet al[29],75 oligometastatic breast cancer patients who had a complete or partial response after systemic therapy and treated with local therapy were retrospectively evaluated,and it was demonstrated that complete response or no evidence of disease rates were significantly better in patients with a single organ metastasis than with two organ metastases (P= 0.002)[29]. In this retrospective study, the multidisciplinary treatment improved OS compared to systemic therapy alone[29].
Few studies have investigated the role of SBRT as a local treatment of metastases in oligometastatic disease including metastatic breast cancer patients (Table 3)[4-6,9,26,28,30,31]. Studies in the literature showed that the maximum benefit from SBRT to all metastatic sites was provided in young patients whose primary breast cancer was controlled, with a limited number of metastases, low tumor volume, only bone metastases, good response to systemic therapy, long disease-free interval (> 12 mo),and hormone receptor-positivity[4,29,30].

Table 3 Retrospective studies investigating the role of radiotherapy as a local treatment of metastases in oligometastatic disease
The prospective studies exploring the role of SBRT to metastatic sites in oligometastatic breast cancer are limited (Table 4)[5,6,9,26,30,31]. Milanoet al[9] performed hypofractionated stereotactic radiation (50 Gy in 10 fractions) to all sites of disease in 48 breast cancer patients with 1-5 extracranial metastases. The authors observed that some patients who have only bone metastases rather than visceral metastases and with low tumor burden (volume and number of lesions) survived longer than 10 years[9].Five- and ten-year OS rates after hypofractionated stereotactic radiation was 83% and 75%, for patients with only bone metastasesvs31% and 17%, respectively, for patients with not only bone metastases[9]. Trovoet al[6] in a prospective phase II trialadministered SBRT (30-45 Gy in 3 fractions) or intensity-modulated RT (60 Gy in 25 fractions) to all metastatic sites in 54 oligometastatic breast cancer patients whose primary tumor was controlled. The authors reported that 2-year local control, OS, and PFS rates with a median follow-up of 30 mo were 97%, 95%, and 53%, respectively,and no ≥ grade 3 toxicity was documented[6]. The first randomized phase II study in metastatic cancer is the SABR-COMET study in which 99 patients with the oligometastatic disease were randomized to receive systemic therapy plus palliative RT (8 Gy in 1 fraction or 30 Gy in 10 fractions) or systemic therapy plus SABR to all metastatic sites. Only 18% of the patients were with breast cancer in this study. There was a significant improvement in terms of 5-year OS (17.7%vs42.3%,P= 0.006), 4-year PFS(3.2%vs21.6%,P= 0.001), and local control rates (46%vs63%,P= 0.039) in patients treated with SABR without any significant adverse events[5]. Results of three ongoing prospective randomized studies (SABR-COMET 10, STEREO-SEIN, and NRG-BR002)are being expected to clarify the role of SBRT to all metastatic sites in oligometastatic breast cancer[32-34].

Table 4 Prospective studies exploring the role of radiotherapy to metastatic sites in oligometastatic disease including primary breast cancer
CONCLUSION
Metastatic breast cancer includes a wide spectrum of disease ranging from oligometastatic to disseminated disease. There has been growing interest during the last 20 years in the curative treatment of oligometastatic breast cancer with the advances in systemic therapy. Aggressive local treatment of primary tumor and metastasesdirected therapies may improve survival in selected patients, and should especially be suggested to young patients with limited number of metastases. The results of ongoing trials specific to breast cancer will be more helpful in the future.
杂志排行
World Journal of Clinical Oncology的其它文章
- Update on the treatment of metastatic renal cell carcinoma
- New approaches for patients with advanced radioiodine-refractory thyroid cancer
- Immunotherapy: A new standard in the treatment of metastatic clear cell renal cell carcinoma
- Association of cancer with comorbid inflammatory conditions and treatment in patients with Lynch syndrome
- Late recurrence of localized pure seminoma in prostate gland: A case report
