Effects of acupuncture combined with Brunnstrom staging on upper-limb motor function, cerebral arterial blood flow velocity, and brain function remodeling after stroke
2022-02-24WANGYanhui王延辉
WANG Yanhui (王延辉)
Department of Rehabilitation Medicine, Shenyang 242 Hospital, Liaoning 110034, China
Abstract
Keywords: Acupuncture Therapy; Cerebral Infarction; Poststroke Syndrome; Hemiplegia; Cerebrovascular Circulation; Blood Flow Velocity
Apoplexy, or stroke, is summarized as a disease caused by brain blood circulation disorder due to various reasons, resulting in insufficient blood and oxygen supply to the brain tissue. The subsequent restrictive or diffuse brain dysfunctions due to hypoxia necrosis may be complicated by a series of obvious neurological deficit symptoms such as facial paralysis, limb dysfunction, and language disorder, bringing a heavy burden to the patient’s family and the society[1]. Traditional Chinese medicine (TCM) believes that apoplexy is caused by deficiency of healthy Qi and disorder of Zang-Fu organs,which leads to the blockage of brain vessels or bleeding.Acupuncture therapy has definite curative effects and is safe for promoting recovery and improving limb function after stroke[2]. Brunnstrom staging therapy is to respectively formulate a rehabilitation program for each stage according to the characteristics of muscle tone and physical movements at six stages after stroke[3]. In this study, we explored the effects of acupuncture combined with Brunnstrom staging on the upper-limb motor function, cerebral arterial blood flow velocity, and brain function remodeling after stroke.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
This study referred to the diagnostic criteria of ischemic stroke in theChinese Guidelines for Diagnosis and Treatment of Acute Ischemic Stroke 2018[4]published by the Chinese Society of Neurology. There may be risk factors for atherosclerosis or evidence of systemic atherosclerosis; focal or general neurological deficits manifested as acute onset; brain CT/MRI examination shows the diameter of cerebral infarction more than 1.5 cm, and cerebral artery imaging confirms corresponding vulnerable atherosclerotic plaques or stenosis >50%; or brain CT/MRI examination shows isolated infarction in the perforator artery supply area,and high-resolution MRI confirms that the blood supply artery has atherosclerotic plaques blocking the opening of perforator artery; non-ischemic causes are excluded.
1.1.2 Criteria for syndrome differentiation of TCM
This study referred to theStandard for Diagnosis and Therapeutic Effect Evaluation of Stroke(Trial)[5]published by the Collaborative Group of Acute Encephalopathy of State Administration of Traditional Chinese Medicine.Primary symptoms are hemiplegia, dizziness or unconsciousness, language disorder or aphasia, half body paresthesia, and wry mouth and tongue.Secondary symptoms are headache, vertigo, squint and unable to wink, change of pupil, choking when drinking,and ataxia. Acute onset, mostly in people over 40 years old, with predisposing factors or aura symptoms.Diagnosis could be confirmed by meeting at least two items of the primary symptoms or one primary symptom plus two secondary symptoms together with the onset age, risking factor, aura symptom, or imaging features.
In the criteria for disease staging, within two weeks since the onset (the longest to one month for apoplexy involving Zang-Fu organs) is the acute stage, two weeks to six months is the recovery period, and six months later is the sequelae period.
1.2 Inclusion criteria
Patients with ischemic stroke diagnosed by the above diagnostic criteria in TCM and Western medicine and imaging examinations such as head CT and MRI examination; first onset, and the course of the disease was in the recovery stage no longer than six months;those with a certain degree of unilateral upper-limb motor dysfunction; with stable vital signs; without comorbidity of other neurological disorders or musculoskeletal diseases; those who had no contraindications to acupuncture treatment; who had no mental disorders, with clear consciousness, had the ability to understand and answer questions, and could communicate normally; signed informed consent.
1.3 Exclusion criteria
Those who had severe organ failure, malignant tumors,endocrine diseases or other diseases that were not suitable for participating in this study; those with cerebrovascular diseases caused by cerebral trauma,cerebral embolism, or craniocerebral operations; those who could not effectively control blood pressure during treatment; who was unable to cooperate with rehabilitation training; those who had wounds or infections at the acupoints; women during pregnancy or lactation.
1.4 Statistical methods
All data involved in this study were processed and analyzed by the SPSS version 23.0 statistical software.The counting data were analyzed by Chi-square test. For measurement data in normal distribution and having homogeneous variance, the independent samplet-test was applied to the comparisons between the groups,and the pairedt-test was applied to the intra-group comparisons. For measurement data in non-normal distribution or without homogeneous variance, the nonparametric test was applied. The rank-sum test was used for rank data.P<0.05 was considered to indicate a statistically significant difference.
1.5 General data
A total of 77 patients with stroke were selected from our hospital between January 2017 and December 2019 to perform a prospective study. This study was reviewed and approved by the Ethics Committee of our hospital(Approval No. 2018-00154). All the patients were randomly divided into two groups by the random number table method, with 39 cases in the observation group and 38 cases in the control group. During the trial,there was no case of dropout in either group. There were no significant differences in the general data between the two groups (P>0.05), indicating that the two groups were comparable (Table 1).
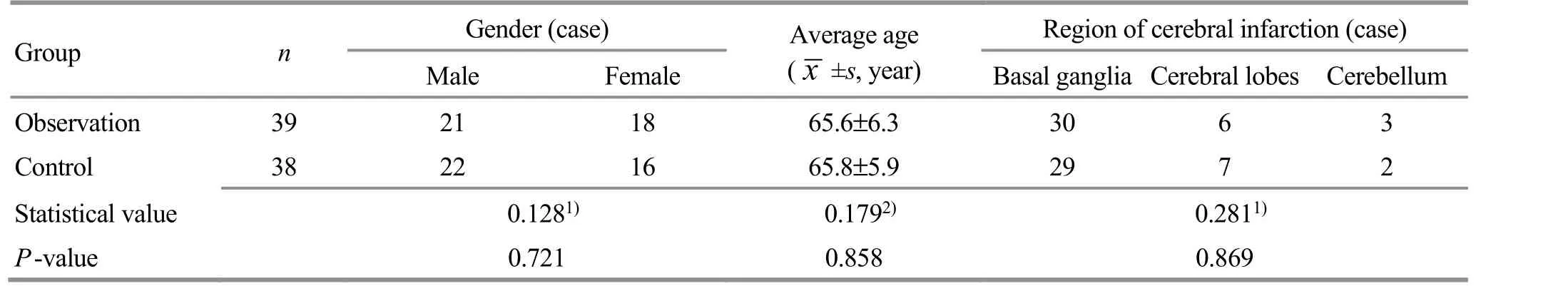
Table 1. Comparison of the general data between the two groups
2 Treatment Methods
2.1 Control group
The control group was treated with conventional symptomatic treatment for stroke combined with Brunnstrom staging functional exercise.
2.1.1 Conventional symptomatic treatment
Control of blood pressure. Amlodipine besylate tablets[specification: 5 mg, State Food and Drug Administration(SFDA) Approval No. H10950224, Pfizer Pharmaceutical Co., Ltd., USA], 5 mg/time, once a day.
Antiplatelet aggregation. Aspirin enteric-coated tablets (specification: 100 mg, SFDA Approval No.J20130078, Bayer Health Care Co., Ltd., Germany),100 mg/time, once a day; clopidogrel bisulfate tablets[specification: 75 mg, SFDA Approval No. J20130083,Sanofi (Hangzhou) Pharmaceutical Co., Ltd., China],150 mg/time, once a day.
Blood lipid regulation. Atorvastatin calcium tablets(specification: 10 mg, SFDA Approval No. H19990258,Beijing Jialin Pharmaceutical Co., Ltd., China),10 mg/time, once a day.
Control of a reasonable daily diet and rest. Less oil and salt, and avoid staying up late.
2.1.2 Brunnstrom staging functional exercise
The Brunnstrom staging consists of six stages[6], and different rehabilitation training methods are adopted for each stage. In stage Ⅰ, the patient is unable to control limbs or move voluntarily, with a low muscle tone and weakened tendon reflexes. At stage Ⅱ, the patient manifests increased muscle tone, tendon hyper-reflexia,associated reactions, and associated movements. In stage Ⅲ, the patient may have some voluntary associated movements like joint movements, but the degree of spasticity is relatively high. At stage Ⅳ, the degree of patient’s spasticity is gradually reduced, and the patient has begun to break away from the associated movement mode. At stage Ⅴ, the spasm of the patient begins to weaken or disappear, and there are more movements separated from the associated movement mode. Stage Ⅵ is manifested as the disappearance of spasm, and coordination or normality of the movement.
As shown in Figure 1-Figure 3, the rehabilitation exercise program for stage Ⅰ to stage Ⅱ is bed turning and the application of associated reactions and associated movements. The program for stage Ⅲ is mainly to control the flexion and extension of the upper limbs, increase the range of joint motion, uplift the scapula in a small range, and promote the associated reactions of the lower limbs to the external stimuli by using the Raimiste phenomenon. In stage Ⅳ, the main exercise purpose is to put the affected limb to the back waist, flex the shoulder by 90°, extend and flex the hand,and rotate the forearm while bending the elbow. StageⅤ mainly trains the scapular region, inhibits the associated reactions of pectoralis major and triceps brachii, and exercises the hand function. In stage Ⅵ, it is to train the daily life abilities and the fine movements of the hand.
2.2 Observation group
The observation group received the same conventional symptomatic treatment and Brunnstrom staging functional exercise as the control group, together with additional acupuncture therapy.
Main acupoints: Shenting (GV24), Baihui (GV20),Sishencong (EX-HN1), and Sanyinjiao (SP6).
Adjunct acupoints and methods: The adjunct acupoints were selected according to the Brunnstrom staging. The depth of acupuncture depends on the patient’s tolerance and muscle thickness. In stage Ⅰ,Neiguan (PC6), Chize (LU5), and Shouwuli (LI13) were selected. Neiguan (PC6) was perpendicularly punctured by 30-35 mm in depth, and twirling-reducing manipulation was performed. Shouwuli (LI13) and Chize(LU5) were perpendicularly punctured by 15-40 mm in depth, and lifting-thrusting reducing manipulation was performed. The manipulation was performed for 1-3 min,and the needles were retained for 15 min. In stages Ⅱ-Ⅳ, the point-toward-point acupuncture method was applied, including Jianyu (LI15) toward Binao (LI14),Yangxi (LI5) toward Pianli (LI6), Naohui (TE13) toward Tianjing (TE10), and Sidu (TE9) toward Waiguan (TE5).Needles were quickly punctured with the tip of the needles toward the target acupoints. Each pair of acupoints were punctured toward each other by a depth of about 40-50 mm. The lifting-thrusting and twirling manipulations were performed to produce needling sensations (Deqi). The needles were retained for 30 min.In stages Ⅴ-Ⅵ, Jianyu (LI15), Waiguan (TE5), and Shenmen (HT7) were selected. The conventional acupuncture method was performed with a depth of 15-50 mm, and even reinforcing-reducing manipulation was applied. The needles were retained for 30 min after Qi arrival (Deqi).

Figure 1. Brunnstrom stages Ⅰ-Ⅱ training method
The acupuncture treatment was performed once a day for six consecutive weeks in total.
3 Observation of Curative Efficacy
3.1 Observation items
3.1.1 TCM symptom score
According to theGuiding Principles for Clinical Study of New Chinese Medicines[7], the symptom classification and quantification scale of stroke was used to evaluate and quantify the symptoms of the two groups before and after the treatment, respectively. The clinical signs such as dizziness, headache, numbness of limbs, and language disorders were scored 0, 2, and 4 points according to the severity of mild, moderate, and severe. The sum of each item was the TCM symptom score. The lower the score,the milder the symptoms.

Figure 2. Brunnstrom stages Ⅲ-Ⅳ training method

Figure 3. Brunnstrom stages Ⅴ-Ⅵ training method
3.1.2 Fugl-Meyer motor function assessment (FMA)
Before and after the treatment, FMA was used to score the limb motor function of the two groups. FMA scale includes five parts: balance ability, joint activity,sensation, upper and lower limbs movement, and pain.The full score of the upper limb part is 66 points, and the higher the score, the better the limb motor function.
3.1.3 Transcranial Doppler (TCD) examination
TCD examination was performed in the two groups before and after the treatment to detect the mean systolic blood flow velocities of the anterior cerebral artery (ACA), middle cerebral artery (MCA), and posterior cerebral artery (PCA).
3.1.4 Modified Edinburgh-Scandinavia stroke scale(MESSS)
MESSS was used to evaluate the neurological function of the two groups before and after the treatment. The lower the MESSS score, the better the recovery of neurological function.
3.1.5 National Institute of Health stroke scale (NIHSS)
There are 12 items in the NIHSS, and the total score is 42 points. The higher the score, the more serious the disease.
3.2 Criteria for curative efficacy
According to the criteria for clinical efficacy of cerebral infarction established by theKey Diagnostic Points for Cerebrovascular Diseases[8], the efficacy was assessed.NIHSS score reduction rate = (NIHSS score before treatment - NIHSS score after treatment) ÷ NIHSS score before treatment × 100%.
Basically cured: NIHSS score reduction rate >90.0%.
Markedly improved: NIHSS score reduction rate >45.0%, but ≤90.0%.
Improved: NIHSS score reduction rate >18.0%, but≤45.0%.
No change or aggravated: After the treatment, the
NIHSS score did not decrease or even increased.
3.3 Results
3.3.1 Comparison of the therapeutic efficacy
As showed in Table 2, the efficacy ranking result of the observation group after the treatment was significantly better than that of the control group (P<0.05), and the total effective rate of the observation group was significantly higher than that of the control group(P<0.05).

Table 2. Comparison of the therapeutic efficacy between the two groups (case)
3.3.2 Comparison of the TCM symptom score
Before the treatment, there were no significant differences in the scores of dizziness, headache, limb numbness, or language disorders between the two groups (P>0.05). After the treatment, the scores of the above four items in both groups decreased, and the intra-group differences were statistically significant(P<0.001). The score of each item in the observation group was lower than that in the control group, and the differences were statistically significant (P<0.05),(Table 3-Table 6).
Table 3. Comparison of the score of dizziness between the two groups ( ±s, point)

Table 3. Comparison of the score of dizziness between the two groups ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 39 3.72±1.24 1.47±0.38 10.834 <0.001 Control 38 3.68±1.17 2.33±0.76 5.965 <0.001 t-value 0.146 6.305 P-value 0.885 <0.001
Table 4. Comparison of the score of headache between the two groups ( ±s, point)

Table 4. Comparison of the score of headache between the two groups ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 39 3.51±0.84 1.56±0.43 12.905 <0.001 Control 38 3.57±0.92 2.14±0.61 7.986 <0.001 t-value 0.299 4.832 P-value 0.766 <0.001
Table 5. Comparison of the score of limb numbness between the two groups ( ±s, point)

Table 5. Comparison of the score of limb numbness between the two groups ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 39 3.43±0.72 1.64±0.48 12.918 <0.001 Control 38 3.39±0.85 2.07±0.55 8.037 <0.001 t-value 0.223 3.658 P-value 0.824 <0.001
Table 6. Comparison of the score of language disorders between the two groups ( ±s, point)

Table 6. Comparison of the score of language disorders between the two groups ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 39 3.39±0.93 1.72±0.54 9.698 <0.001 Control 38 3.46±1.05 2.23±0.51 6.496 <0.001 t-value 0.310 4.258 P-value 0.758 <0.001
3.3.3 Comparison of the upper-limb FMA score
Before the treatment, there was no significant difference in the upper-limb FMA score between the two groups (P>0.05). After the treatment, the upper-limb FMA score in both groups increased, and the intra-group differences were statistically significant (P<0.001). The score in the observation group was significantly higher than that in the control group (P<0.05), (Table 7).
3.3.4 Comparison of the cerebral artery blood flow velocities by TCD
Before the treatment, there were no significant differences in the mean systolic blood flow velocities of ACA, MCA, or PCA between the two groups (P>0.05).After the treatment, the mean systolic blood flow velocities of the ACA, MCA, and PCA in both groups increased, and the intra-group differences were statistically significant (P<0.001). The blood flow velocities in the observation group were significantly higher than those in the control group (P<0.001), (Table 8-Table 10).
3.3.5 Comparison of the MESSS score
Before the treatment, there was no significant difference in MESSS score between the two groups(P>0.05). After the treatment, the MESSS scores in both groups decreased, and the intra-group differences were statistically significant (P<0.001). The score in the observation group was significantly lower than that in the control group (P<0.05), (Table 11).
Table 7. Comparison of the upper-limb FMA score between the two groups before and after the treatment ( ±s, point)

Table 7. Comparison of the upper-limb FMA score between the two groups before and after the treatment ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 39 36.76±7.54 48.37±7.24 6.918 <0.001 Control 38 37.19±7.23 43.85±6.63 4.185 <0.001 t-value 0.256 2.855 P-value 0.799 0.006
Table 8. Comparison of the anterior cerebral artery blood flow velocity between the two groups ( ±s, cm/s)

Table 8. Comparison of the anterior cerebral artery blood flow velocity between the two groups ( ±s, cm/s)
Group n Before treatment After treatment t-value P-value Observation 39 37.08±5.12 49.43±5.38 10.385 <0.001 Control 38 36.59±4.71 43.37±5.24 5.932 <0.001 t-value 0.437 5.005 P-value 0.664 <0.001
Table 9. Comparison of the middle cerebral artery blood flow velocity between the two groups ( ±s, cm/s))
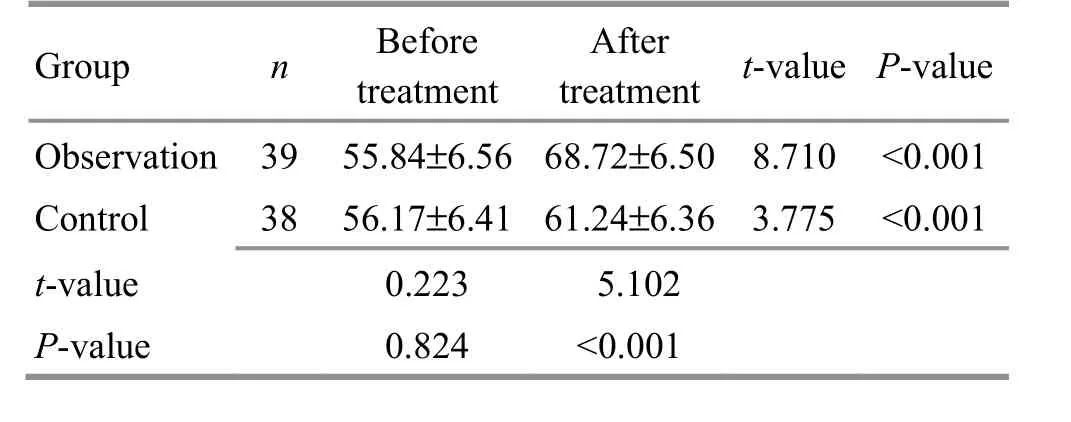
Table 9. Comparison of the middle cerebral artery blood flow velocity between the two groups ( ±s, cm/s))
Group n Before treatment After treatment t-value P-value Observation 39 55.84±6.56 68.72±6.50 8.710 <0.001 Control 38 56.17±6.41 61.24±6.36 3.775 <0.001 t-value 0.223 5.102 P-value 0.824 <0.001
Table 10. Comparison of the posterior cerebral artery blood flow velocity between the two groups ( ±s, cm/s)

Table 10. Comparison of the posterior cerebral artery blood flow velocity between the two groups ( ±s, cm/s)
Group n Before treatment After treatment t-value P-value Observation 39 35.84±4.86 68.72±6.50 25.301 <0.001 Control 38 37.48±4.55 44.86±5.13 6.635 <0.001 t-value 0.262 9.755 P-value 0.794 <0.001
Table 11. Comparison of the MESSS score between the two groups ( ±s, point)

Table 11. Comparison of the MESSS score between the two groups ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 39 28.79±5.32 13.36±4.58 13.727 <0.001 Control 38 28.43±5.29 16.84±4.75 10.049 <0.001 t-value 0.298 3.273 P-value 0.767 0.002
3.3.6 Comparison of the NIHSS score
Before the treatment, there was no significant difference in NIHSS score between the two groups(P>0.05). After the treatment, the NIHSS scores in both groups decreased, and the intra-group differences were statistically significant (P<0.001). The score in the observation group was significantly lower than that in the control group (P<0.001), (Table 12).
Table 12. Comparison of the NIHSS score between the two groups ( ±s, point)

Table 12. Comparison of the NIHSS score between the two groups ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 39 32.15±5.42 19.80±3.37 12.084 <0.001 Control 38 31.78±6.10 23.65±4.50 6.611 <0.001 t-value 0.282 4.257 P-value 0.779 <0.001
4 Discussion
Stroke is a type of brain blood supply disorder caused by abnormal blood flow, changes in blood composition,and vascular injuries such as cerebral atherosclerosis.After vascular injury, thrombus is formed under the action of platelet adhesion and aggregation to block the cerebral vessels, causing insufficient local blood supply to the brain tissue and leading to hypoxia and ischemia.Over time, irreversible damages such as encephalomalacia will occur. At the same time, nerve cells will also undergo apoptosis due to ischemia and hypoxia[9]. Patients after stroke will have dysfunctions such as hemiplegia and language disorders, and poststroke limb dysfunction is one of the most common sequelae. In the early stage, the patient usually manifests flaccid paralysis due to loss of muscle strength.Nevertheless, during the recovery process, increased muscle tone and abnormal long-term movement patterns can cause spastic paralysis[10].
Most of the stroke patients are elderly people who often have aura symptoms such as dizziness, headache,limb numbness, and stiffness before the onset. The etiology is mostly related to physical deficiency, chronic strain, and deficiency of healthy Qi in the elderly. TCM believes that most middle-aged and elderly people have Yin deficiency of liver and kidney, and insufficiency of Qi and blood. Excessive fatigue, improper diet, and emotional disturbance can all lead to disorders of meridians and Zang-Fu organs, adverse flow of Qi and blood, and obstruction of blood stasis and phlegmturbidity in the brain, invading the clear orifices and resulting in apoplexy (stroke). Meanwhile, the disorder of Qi and blood movement caused by the imbalance of Zang-Fu organs and Yin-Yang can also lead to malnutrition of tendons and meridians, and uncontrolled dystonia of limbs, thus presenting as hemiplegia and stiff limbs[11]. Acupuncture therapy is effective in improving cerebral blood circulation and limb motor function in stroke patients. The pathological mechanisms of stroke in different stages are also different. Combining modern rehabilitation medicine with different acupuncture protocols according to different stages can further improve the efficacy of acupuncture. The theoretical basis of acupuncture therapy is meridians and acupoints. Acupoints at the head are dense, among which Shenting (GV24) can refresh the brain and open the orifices, and harmonize Yin and Yang. Baihui (GV20) and Sishencong (EX-HN1)can raise Yang Qi upward to the brain, filling the marrow and strengthening the brain. Sanyinjiao (SP6) is the crossing point of three Yin meridians of foot, with the effect of harmonizing and balancing Yin and Yang of the body. From the anatomical point of view, Shenting(GV24), Baihui (GV20), and Sishencong (EX-HN1) are located in the projection areas of brain functional areas,among which Baihui (GV20) and Sishencong (EX-HN1)are located in the parietal projection area. The parietal lobe is the primary sensory center and the formation area of spatial perception, thus playing an important role in improving cerebral circulation and regulating brain function. Therefore, they are commonly used for the treatment of stroke[12-14].
Brunnstrom staging theory believes that limb motor dysfunction after stroke is also a sensory disorder to a certain extent. Consciousness and sensation play a critical role in the recovery process. Using sensory stimulation to induce synergistic actions and associated responses can promote muscle contractions of the affected limbs. Breaking down the actions and repeated training can effectively improve the motor function of limbs. The core is to adopt different exercise programs for different stages such as flaccid period, spastic period,and isolated movement period[15]. The flaccid period corresponds to Wei-Flaccidity syndrome in TCM. During this period, the patient has a low muscle tone and disabled limbs. Neiguan (PC6), Chize (LU5), and Shouwuli(LI13) are selected to promote Qi for activating collaterals, unblock meridians for dispelling blood stasis,and harmonize Qi and blood, to improve muscle strength and muscle tone[16]. In the spastic stage, the muscle tone of patients gradually recovers, but due to the long course of disease and long-term abnormal movement patterns,the body has lost the balance of Yin and Yang, and the tendons and meridians have lost nourishment.Acupuncture should focus on the acupoints of the Shaoyang Meridian and Taiyang Meridian of Hand and Foot. In this study, point-toward-point acupuncture method was applied, including Jianyu (LI15) toward Binao (LI14), Yangxi (LI5) toward Pianli (LI6), Naohui(TE13) toward Tianjing (TE10), and Sidu (TE9) toward Waiguan (TE5). Among them, Jianyu (LI15), Binao (LI14),Yangxi (LI5), and Pianli (LI6) have the effects of unblocking the meridians and collaterals and relieving spastic pain. Naohui (TE13), Waiguan (TE5), Tianjing(TE10), and Sidu (TE9) are located in antagonists, so that they can harmonize Yin and Yang to inhibit spasms and coordinate muscle movements[17]. During the improving period, puncturing Jianyu (LI15), Waiguan (TE5), and Shenmen (HT7) can dredge Qi and blood, promote isolated movements, and consolidate the curative effect[18-19].
The results of this study showed that the total effective rate of the observation group was 94.9%, which was significantly higher than 79.0 % of the control group(P<0.05). The TCM symptom scores of dizziness,headache, limb numbness, and language disorders in both groups decreased, and the scores in the observation group were significantly lower than those in the control group (P<0.05). These results suggest that acupuncture combined with Brunnstrom staging can better improve the clinical symptoms of the patients. The FMA is an evaluation method for physical motility dysfunction. The FMA scores of the upper limbs in both groups increased, and the score in the observation group was significantly higher than that in the control group(P<0.05), indicating that the recovery of the upper-limb motor function in the observation group is more significant. TCD is an effective method to determine the degree of intracranial vascular stenosis and blood circulation in stroke patients. After the treatment, the mean blood flow velocities of the ACA, MCA, and PCA in both groups increased, and were significantly higher in the observation group than in the control group (P<0.05),indicating that acupuncture combined with Brunnstrom staging can effectively increase the blood flow velocity of the cerebral artery and improve cerebral microcirculation. Remodeling of brain function refers to the repair of damaged nerves through neural circuit reorganization and the use of nerve plasticity after brain injuries. ZHU W Z,et al[20]found in experiments on rats with focal cerebral infarction that scalp acupuncture can effectively increase the positive expression of microtubule-associated protein 2 in the ischemic cortex of rats, suggesting that acupuncture therapy has a certain effect on nerve plasticity. In this study, the MESSS and NIHSS scores in both groups decreased, and the scores in the observation group were significantly lower than those in the control group (P<0.05), indicating that acupuncture combined with Brunnstrom staging has a good effect in improving the advanced central nervous function and promoting brain function remodeling in stroke patients.
In summary, acupuncture combined with Brunnstrom staging is effective for stroke. It can effectively improve the upper-limb motor function, increase cerebral artery blood flow velocity, restore neurological function, and promote brain function remodeling.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Key Science and Technology Project of Traditional Chinese Medicine of Liaoning Provincial Department of Health (辽宁省卫生厅中医重点科技项目, No. 2018NS00238).
Statement of Informed Consent
This work was approved by the Ethics Committee of Shenyang 242 Hospital (Approval No. 2018-00154).Informed consent was obtained from all individual participants.
Received: 14 September 2020/Accepted: 27 April 2021
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture with different frequencies on hippocampal neuronal apoptosis and JNK signaling pathway in rats with vascular dementia
- Effects of electroacupuncture pretreatment on M1 polarization of alveolar macrophages in rats with acute lung injury
- Clinical observation on row needling at the Governor Vessel on the head for poststroke insomnia
- Effects of Tuina combined with graded motor imagery on the upper-limb motor function and quality of life of patients with hemiplegia after stroke
- Observation of the efficacy and safety of the Song-Relaxing and Zhen-Vibrating abdomen manipulation for patients with prediabetes
- Clinical study on Tuina plus Shen Ling Bai Zhu San in treating children with diarrhea due to spleen deficiency
