Outcomes of half-width vertical rectus transposition augmented with posterior fixation sutures for sixth cranial nerve palsy
2021-12-17OrtalFogelTempelhofAnatBacharZiporiChaimStolovitchOrielSpierer
Ortal Fogel-Tempelhof, Anat Bachar Zipori, Chaim Stolovitch, Oriel Spierer
1Department of Ophthalmology, Tel Aviv Sourasky Medical Center, Affiliated to the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv 6423906, Israel
2Pediatric Ophthalmology and Strabismus Unit, E. Wolfson Medical Center, Affiliated to the Sackler Faculty of Medicine,Tel Aviv University, Tel Aviv 6423906, Israel
Abstract
● KEYWORDS: vertical rectus muscles transposition; sixth nerve palsy; abducens nerve palsy; esotropia; strabismus surgery
INTRODUCTION
Six cranial nerve palsy usually manifests as an incomitant esotropia that increases on ipsilateral gaze due to lateral rectus (LR) weakness and limitation in abduction. Various procedures have been suggested for the treatment of the esotropia and diplopia. Hummelsheim was the first to describe vertical rectus transposition (VRT) over a century ago. He transposed the lateral halves of the vertical rectus muscles temporally to the LR insertion, enhancing the abduction vector and preserving anterior ciliary artery perfusion. Over the years,many modifications have been proposed to treat paralytic strabismus, such as the Jensen procedure, in which the transposition is made without disinsertion, or the full tendon transposition. Ipsilateral combination surgeries with resection of the transposed muscles, medial rectus (MR) recession or botulinum injection to the MR have also been described[1]. In 1997, Foster introduced the posterior fixation sutures for fulltendon transposition, known as the Foster’s augmentation sutures[2], which increase the horizontal tonic force vector,thus enhancing the range of abduction once the antagonist(MR muscle) relaxes[3]. Foster showed a 93.8% reduction in esotropia from a mean of 58 prism diopter (PD) to 3.6 PD and elimination of face turn, with only minimal vertical deviation.These technique has possible benefits, including a lower risk for post-operative vertical deviation, decreased need for MR recession with the reduced risk for adduction limitation and anterior segment ischemia[2].
Foster’s sutures were originally described for full-tendon VRT. However, the Foster’s posterior augmentation sutures can also be applied for partial tendon VRT, while sparing the ciliary arteries’ blood supply[4-5]. In this report, we present our experience with the Hummelsheim’s procedure (partial VRT)augmented with Foster’s posterior fixation sutures, with or without MR recession, for sixth nerve palsy.
SUBJECTS AND METHODS
Ethical Approval Study design and data collection confirmed with all local laws and complied with the principles of the Declaration of Helsinki. The study was approved by the Tel Aviv Medical Center Institutional Review Board. As this was a retrospective study, an informed consent was waived by the Institutional Review Board.
The medical records of all patients who underwent half-width VRT augmented with Foster’s posterior fixation sutures for esotropia associated with sixth nerve palsy from January 2003 to December 2018, were retrospectively reviewed. Included in the study were patients who had completed a minimal postoperative follow-up of six weeks. The angle of deviation was measured using the prism cover test for distance (6 m) and near (30 cm) fixation with the appropriate refractive correction.For each patient, pre- and post-operatively, the largest measured angle was used for the calculations, usually resulting with the angle for distance, except in young infants, where measurements were made at near fixation using the Krimsky test. For very large angles, a prism was placed in front of each eye simultaneously, and the sum of the two prisms was calculated according to a standardized table. Ductions and versions were also documented. Abduction deficit was graded on a scale of 0, indicating full duction, to -4 for an eye that reaches but does not cross the midline, and -5 if eye remained in esotropia in attempted abduction.
The following parameters were obtained during data collection:age at diagnosis and at surgery, gender, etiology of sixth nerve palsy and the presence of amblyopia. Visual acuity, refractive error, the angle of deviation in primary position, the presence of abnormal head position (obtained to avoid diplopia and achieve fusion), and abduction deficit were also collected from the ocular examination performed at the pre-operative visit and at 6wk, 6mo and last follow-up visit over 1y. Improvement in abduction was considered as at least 1 grade improvement on the abduction deficit scale, and a significant improvement as 2 grades or more, or an eye abducting to the midline when preoperatively could not.
(1)资本结构,用资产负债率(XAL)替代。计算公式为:资产负债率=负债总额/资产总额。资产负债率是衡量银行负债水平及风险程度的重要指标。过高,说明银行面临较大的财务风险;过低,说明银行吸收存款的能力不足,营利性较差。
Success was defined if two of the following conditions occurred: head position improvement, resolution of diplopia at primary position and a residual deviation of ≤10 PD without a vertical deviation, for near and far.
Surgical Technique Surgeries were performed through a fornix-based incision, supero-temporally and inferotemporally. Each vertical muscle was split in half with a small hook posteriorly, sparing the anterior ciliary arteries. A doublearmed 6/0 polyglactin 910 (Vicryl) suture was passed through the temporal half of each vertical recti, allowing its disinsertion from sclera and temporal transposition. The isolated halves were then accordingly reattached along the spiral of Tillaux to the superior and inferior border of the lateral rectus insertion as previously described[4-5]. Posterior fixation sutures were placed 8 mm from the LR insertion passing through sclera using a non-absorbable suture. The decision whether to add a recession of the MR or not, was affected by three variables:1) The preoperative angle of esotropia; 2) The results of a forced duction test which was done at the beginning of every surgery; 3) Was the MR muscle already recessed in a previous surgery. If the forced duction test was positive, then the MR was recessed. However, if the forced duction test was negative then MR recession was performed if the angle of esotropia was large, upon surgeon’s discretion.
Statistical Analysis Categorical variables are presented as frequency and percentage. Continuous variables are presented as mean±standard deviation and range. The Wilcoxon signedrank test was used for matched pairs. An association between success and categorical variables was evaluated using Fisher’s exact test. Association between success and continuous/ordinal variables was evaluated using Mann-Whitney 2-sided test.Analyses were two-tailed, and significance was set at the 5%level. Statistical analysis was performed using SPSS (IBM SPSS statistics for windows, version 25.0, IBM Corp. Armonk,NY, USA, released 2017).
RESULTS
Fifteen patients (11 females, 73.3%) met the study’s inclusion criteria. Mean age at diagnosis was 30.6±19.6y (range 1mo-65.1y). Patients’ characteristics are presented in Table 1. Mean time from initial diagnosis of sixth nerve palsy to surgery was 43.4±71.8mo (range 7-286mo). Three patients (20.0%) had previous ipsilateral MR recession and LR resection surgery.MR recession was combined with the transposition surgery in 9 patients (60.0%) without prior surgeries. There were no intraoperative complications. Mean follow-up after the surgery was 21.4±23.2mo (range 1.5-82mo). All except two patients had a mean follow-up of more than 6mo. Abnormal head position was noted in 6 patients (40.0%) upon presentation.Postoperative outcomes are summarized in Table 1 at 6wk,6mo and at more than 1y of follow-up. Nonetheless, because a few patients were lost to follow-up and did not reach ≥1y of follow-up, we decided to present the results in the following paragraph at 6wk postoperatively, 6mo postoperatively and as a total summary of our patients at their final followup. Preoperative mean angle of deviation was 51.3±19.7 PD(range 20-90 PD). Mean angle of deviation improved to 5.21±21.21 PD (range -35 to 35 PD,P=0.001) 6wk postoperatively, 6.7±20.5 PD (range -40 to 25 PD,P=0.002)6mo postoperatively, and 7.7±20.2 PD (range -40 to 35 PD,P=0.001) on final follow-up. Undercorrection of over 10 PD was seen in 6/15 (40%), 7/12 (58.3%) and 8/15 (53.3%) of patients at 6wk, 6mo and on final follow-up examination,respectively. Overcorrections (exotropia of more than 10 PD)was seen in 3/15 (20%), 2/12 (16.7%) and 2/15 (13.3%) of the patients at 6wk, 6mo and on last follow-up, respectively.Surgical success was achieved in 33.3% of our patients on final follow-up visit, and 50% of the patients who completed more than one year of follow-up. Improvement in diplopia, for near and far, was reported by 10 patients (66.7%). Improvement in abduction limitation was seen at 6wk and 6mo and last followup visits (P=0.002, 0.017, and 0.002, respectively), with 10 patients (66.7%) achieving mild improvement in abduction on final follow-up, 7 of them reaching significant improvement.

Table 1 Pre- and post-operative data for patients with esotropia associated with sixth nerve palsy undergoing half-thickness VRT augmented with Foster’s posterior fixation sutures n=15
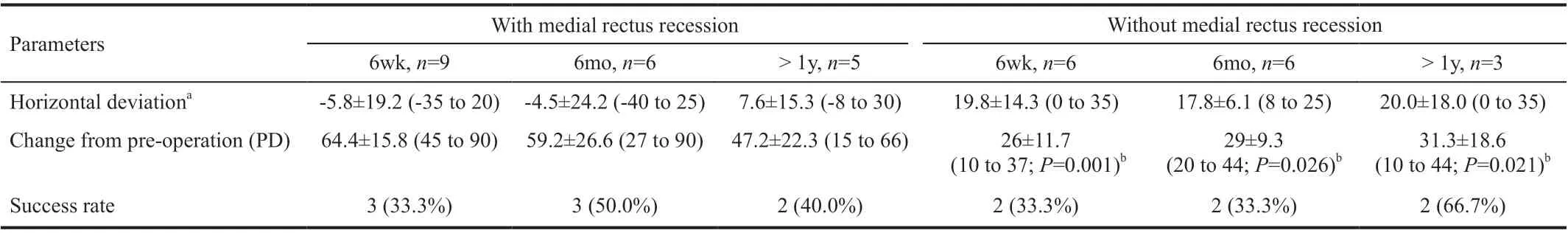
Table 2 Post-operative results for patients with esotropia associated with sixth nerve palsy who underwent augmented half-thickness VRT with or without medial rectus recession n=15
Two patients developed vertical deviation immediately after surgery. In one patient it had resolved 2y post-surgery, while in the other it did not resolve 2mo postoperatively (patient was lost to follow up). One patient developed a small vertical deviation more than a year following surgery and was managed with prisms. Post-operative anterior segment ischemia did not occur in any of the patients.
All patients with overcorrection had a combined partial VRT with MR recession, as depicted in Table 2. Combined partial VRT with MR recession was correlated with a larger change in postoperative horizontal deviation from baseline compared to partial VRT devoid of MR recession at 6wk (P=0.001), at 6mo(P=0.026) after surgery and on last follow-up appointment(P=0.021). Table 3 shows the amount the of MR recession that was done combined with the half-width VRT in each patient compared to the amount of correction that was achieved at final follow-up visit. The amount of correction that was achieved compared to 1 mm of recession in this cohort of patients ranged from 3 PD per 1 mm of MR recession in combination with partial VRT to 16.4 PD of change per 1 mm of MR recession.Patient 7 had a very large overcorrection resulting in 40 PD exotropia. In this patient, soon after the surgery the brain tumor recurred. A force generation test and a forced duction test were performed 3mo postoperatively and demonstrated reduced muscle activity in the field of action of the MR with no signs of lateral rectus restriction. The possible cause was slipped MR muscle or oculomotor nerve palsy due to recurrent brain tumor.The patient refused another surgery.

Table 3 Post-operative change in prism diopters and amount of medial rectus recession in patients with sixth nerve palsy who underwent augmented half-thickness VRT with medial rectus recession n=9
DISCUSSION
The current study results indicate that partial-width VRT with posterior fixation sutures is a safe and effective procedure for esotropia associated with sixth nerve palsy with a third of our patients achieving surgical success at final follow-up. A substantial reduction in the esotropia angle was noted after the surgery in all our patients.
Comparing our surgical results with previous reports on esotropia associated with sixth cranial nerve palsy is quite challenging. Table 4 summarizes most of these studies with a minimum of 5 patients. Many of the earlier studies had a small sample size, comprising of a diverse group of patients (e.g., Duane type 1, sixth nerve palsy, gaze palsy).In addition, numerous combination of surgical techniques were used[2,4-24]. As in some of the previous studies[4,10,12-14,17], a few of our patients had previous strabismus surgery, which further complicates comparison between studies. All three of them had an uncombined VRT surgery: 1 was orthophoric on final examination, and 2 remained with a large esotropic deviation.Another obstacle for comparison is the difference in the follow-up periods between the different studies. We used a very strict definition of surgical success, incorporating several parameters in both near and distance, to indicate improved fusional range. We included head position improvement and/or resolution of diplopia in primary position with residual horizontal deviation in primary position of ≤10 PD with no vertical deviation. However, many of the previous papers defined success according to the magnitude of the postoperative angle or the improvement in abduction. In this cohort, the improvement in abduction was significant, with 66.7% of the patients achieving improvement on last follow-up visit. We did not include improvement in abduction as a key to define surgical success as it is prone to surgeon’s bias.Improvement in the range of single binocular vision was only implied by the lack of diplopia in primary position, and postoperative head position was noted but not measured. Despite its relative importance when reporting on the efficacy of a transposition procedure[2,18,25], this data was not available for this retrospective review.
Contraction of the ipsilateral MR necessitates further intervention with MR weakening procedure, either by MR recession or by botulinum injection[2,5,13,26]. According to some reports, this additional procedure enhances the exoshift by 12-45 PD[5,17,27],allowing for large angle esotropia correction and better alignment in primary position. However, overcorrection with final significant exotropia is a substantial possible complication[12,14,17]. A significantly higher overcorrection rate was demonstrated with MR recession in our study, as compared to the surgeries without MR recession. Our results indicate that the risk of overcorrections is quite low when halfwidth VRT with Foster augmentation sutures is performed as a single procedure and that this procedure alone can correct up to 45 PD of esotropia in patients with sixth nerve palsy.Nonetheless, for larger angles, an additional procedure should be considered. Unfortunately, from our analysis of the results we could not form a rule regarding the amount of recession that is necessary to achieve corrections of larger esotropias, as the amount of correction that was achieved per one mm of MR recession varied widely.
Previous reports had shown undesirable new vertical deviation in 5%-32% of the patients undergoing VRT(Table 4)[2,5,7-8,12-15,19-20], with no apparent association to muscle width (partialvsfull width transposition) or to posterior fixation sutures location. Phamonvaechavanet al[14]noted that even the use of crossed-adjustable transposition technique,cannot eliminate completely postoperative vertical deviation.We demonstrated a comparable incidence of vertical deviation of 12.5%-16.7% during follow-up period. None of our patients required further surgery to correct their vertical diplopia. One patient with preoperative hypotropia had resolution by the end of follow up and the others were treated with prisms and did not require further surgery.

Table 4 Studies on different recti muscles transposition surgeries for esotropia associated with sixth cranial nerve palsy
One major concern when operating on multiple extraocular muscles is anterior segment ischemia. Partial thickness VRT spares the anterior ciliary arteries allowing simultaneous intervention on the MR when needed. However, care must be taken not to harm the arteries while splitting the vertical muscle as anterior segment ischemia has been previously reported with partial thickness VRT combined with MR recession[28].None of our patients had this complication.
In general, VRT does not cause adduction limitation postoperatively. There are only two reports in the literature of significant limitation in adduction after VRT[14,29]. In the current study, 3 patients had a mild adduction deficit that was associated with MR recession (either simultaneous or a previous recession). Only one patient had a severe adduction limitation attributed to oculomotor nerve palsy due to recurrent brain tumor, or slipped MR muscle.
The retrospective nature of our study is its main limitation.The small heterogenous sample size is another limitation.However, this surgical procedure is very uncommon. Some of the other notable limitations are previous ipsilateral strabismus surgery in some patients, and the short follow-up period of few of them, which may influence the measurements due to temporary post-operative changes, such as rectus muscle swelling. Nevertheless, as opposed to some other studies, we have included only patients with sixth cranial nerve palsy and excluded all patients with Duane syndrome, thus reporting a homogenous group of patients.
In conclusion, half-width VRT with posterior fixation sutures for complete sixth nerve palsy, is a safe procedure with a relatively favorable outcome. It is suitable as a standalone procedure for correction of up to 45 PD of esotropia.Combination with MR recession can be considered for very large esotropia but may cause overcorrection. Vertical deviation is a complication which may resolve spontaneously over time or be corrected with prisms. All these aspects should be discussed with the patient when considering surgery.
ACKNOWLEDGEMENTS
Conflicts of Interest:Fogel-Tempelhof O, None;Bachar Zipori A, None; Stolovitch C, None; Spierer O,None.
猜你喜欢
杂志排行
International Journal of Ophthalmology的其它文章
- Upregulation of ASPP2 expression alleviates the development of proliferative vitreoretinopathy in a rat model
- Mesenchymal stem cell-derived exosomes inhibit the VEGF-A expression in human retinal vascular endothelial cells induced by high glucose
- Protective effects of umbilical cord mesenchymal stem cell exosomes in a diabetic rat model through live retinal imaging
- New technique for removal of perfluorocarbon liquid related sticky silicone oil and literature review
- Quantitative analysis of retinal vasculature in normal eyes using ultra-widefield fluorescein angiography
- Evaluation of the long-term effect of foldable capsular vitreous bodies in severe ocular rupture
