COVID-19 : Effect on gastroenterology and hepatology service provision and training: Lessons learnt and planning for the future
2021-12-06MuhammadRaheelAnjumJodieChalmersRizwanaHamidNeilRajoriya
Muhammad Raheel Anjum, Jodie Chalmers, Rizwana Hamid, Neil Rajoriya
Abstract In late 2019 , reports arose of a new respiratory disease in China, identified as a novel coronavirus, severe acute respiratory syndrome coronavirus 2 . The World Health Organisation named the disease caused by the virus ‘coronavirus disease 2019 (COVID-19 )’. It was declared a pandemic in early 2020 , after the disease rapidly spread across the world. COVID-19 has not only resulted in substantial morbidity and mortality but also significantly impacted healthcare service provision and training across all medical specialties with gastroenterology and Hepatology services being no exception. Internationally, most, if not all ‘nonurgent’ services have been placed on hold during surges of infections. As a result there have been delayed diagnoses, procedures, and surgeries which will undoubtedly result in increased morbidity and mortality. Outpatient services have been converted to remote consultations where possible in many countries.Trainees have been redeployed to help care for COVID-19 patients in other settings, resulting in disruption to their training - particularly endoscopy and outpatient clinics. This has led to significant anxiety amongst trainees, and risks prolongation of training. It is of the utmost importance to develop strategies that continue to support COVID-19 -related service provision, whilst also supporting existing and future gastroenterology and Hepatology services and training.Changes to healthcare provision during the pandemic have generated new and improved frameworks of service and training delivery, which can be adopted in the post-COVID-19 world, leading to enhanced patient care.
Key Words: COVID-19 ; Gastroenterology; Hepatology; Training; Service provision
INTRODUCTION
In December 2019 , China’s regional World Health Organisation (WHO) office was informed of a new respiratory disease of unknown cause[1 ], detected in Wuhan, Hubei Province, China. It was characterised as a novel coronavirus strain, severe acute respiratory syndrome coronavirus 2 ; the WHO subsequently designated the disease caused by the virus as ‘coronavirus disease 2019 (COVID-19 )’. The virus spread rapidly and a Public Health Emergency of International Concern was declared at the end of January 2020 , followed by pronouncement of a global pandemic in March 2020 .The WHO asked for global preparedness to detect and manage COVID-19 [1 ], urging countries to ensure they had adequate hospital resources and functional test-and-trace systems. The epicentre of the pandemic shifted to Europe in March 2020 and cases began to rise exponentially in the United Kingdom. The first United Kingdom case of COVID-19 was in a 75 -year-old lady on February 21 , 2020 , identified through a retrospective analysis of sputum samples by the University of Nottingham[2 ]. At the time of writing, COVID-19 has claimed over 128000 Lives in the United Kingdom[3 ]and over 3 .9 million worldwide[4 ]. These figures from United Kingdom pertain to individuals that died within 28 d of a positive test; they do not consider the likely substantial number of indirect deaths. With the global spread of COVID-19 , there has been an unprecedented impact on healthcare services. Wards and intensive care units(ICUs) have been inundated with COVID-19 patients, and healthcare staff have been redeployed from their base specialities to help care for COVID-19 patients. Resource scarcity, in addition to the risk of virus transmission with face-to-face interaction means that speciality services have been decimated. In the field of gastroenterology and hepatology, many different aspects of service provision have been affected such as a significant reduction in diagnostic and therapeutic endoscopy. Out-patient clinics have been cancelled or moved to remote consultations; liver transplantation programmes have been temporarily halted or limited to only super-urgent transplantation at times. These changes, combined with the redeployment of trainees to COVID-19 wards and ICUs, have resulted in restricted gastroenterology and hepatology training, and an associated impact on trainees’ morale. This article will review the available evidence regarding gastroenterology and hepatology service provision and training during the pandemic. We will provide an overview of the disruption caused by the COVID-19 , and also review recommendations to minimise the impact of this disruption. The United Kingdom will be used as a reference, as it is familiar to the authors; other countries will be compared and contrasted throughout.At time of writing, the United Kingdom healthcare system is dealing with a further peak of infections (January/February 2021 ).
THE EFFECT OF COVID-19 ON GASTROENTEROLOGY AND HEPATOLOGY SERVICES
An overview of the disruption
Worldwide, most countries imposed national lockdowns to tackle rising COVID-19 cases. In the United Kingdom, this was first implemented on March 23 , 2020 . In the NHS most elective medical and surgical work was halted in an attempt to increase availability of bed spaces for COVID-19 patients requiring hospital admission. Staff were redeployed to departments with increasing pressures - primarily ICUs, Acute Medicine and Respiratory wards with doctors often required to fill other staffing vacancies such as ICU nursing. In gastroenterology and hepatology, the effects from COVID-19 have not been discriminatory; all ranks of staff, from junior doctors to consultants, have been affected[5 -8 ]. In the United Kingdom, the British Society of Gastroenterology (BSG) issued consensus guidelines on endoscopy service provision,and the management of specific disease patient cohorts, including: Inflammatory bowel disease (IBD), chronic liver disease, immunosuppressed patients, coeliac disease, and on transjugular intrahepatic portosystemic shunt service provision[9 ].Similarly, gastroenterology and hepatology associations and experts worldwide have issued consensus opinions and guidelines regarding the management of patients during the pandemic[10 -15 ]; which will be expanded upon throughout this article.
Endoscopy
During the peak of the pandemic, a number of major gastroenterology societies worldwide advised to postpone non-urgent examinations[16 ] including: The European Society of Gastrointestinal Endoscopy[17 ], the World Endoscopy Organisation[18 ], the American College of Gastroenterology, the American Society for Gastrointestinal Endoscopy[19 ], the Canadian Association of Gastroenterology[20 ], joint statements from Indian Gastroenterology societies[21 ], and the Gastroenterological Society of Australia[22 ]. Recommendations from major organisations have been summarised in Table 1 .
In conjunction with other position statements and expert opinions[16 ,17 ,23 ,24 ], the BSG issued a statement during the first wave of the pandemic stating that ‘all non emergency Gastrointestinal (GI) endoscopic procedures should stop immediately’[25 ],for an initial period of six weeks. The recommendation included the Bowel Cancer Screening Programme (BCSP), symptomatic two-week-wait (2 WW) and Urgent Suspected Cancer (USC) referrals. The statement concluded that very few patients were likely to come to harm from the pause, highlighting that the lack of ICU beds and potential risk of higher surgical mortality during the initial COVID-19 peak may in fact cause harm if endoscopy was continued as before. The BSG accepted that a small number of patients may have a delay in their diagnosis[26 ]; and advised that 2 WW and USC referrals should be individually triaged and risk-assessed by gastroenterology consultants. An ‘Urgent Deferred Waiting List’ was created, so as to prioritise follow-up and investigations when services resumed. Of note, urgent 2 WW referrals by primary care physicians, primarily for patients with suspected cancer, decreased by up to 80 % during the first peak of the infections[27 ]. Endoscopy service disruption occurred worldwide. Alboraieet al[7 ] obtained data from 163 participating centres,across 48 countries and 6 continents. The majority (93 .9 %) of the centres were hospitalbased endoscopy units, affiliated with teaching hospitals. The centres reported a significant reduction in their procedural numbers during the pandemic: 85 % reported that procedure volume decreased by > 50 %, with only emergency services being continued, and four endoscopy units (2 .45 %) completely suspended procedures. The top three indications for endoscopic procedures included upper GI bleeding (89 .6 %),lower GI bleeding (65 .6 %), and cholangitis (62 .6 %)[7 ]. A study from Melbourne,Australia also demonstrated that significantly fewer procedures were performed during the peak of COVID-19 , as compared to the pre-pandemic era[28 ]. A survey of 123 North American gastroenterology practices, comprising of 1379 Gastroenterologists in 32 United States states and 4 Canadian provinces observed a 90 % decrease in endoscopy volume during the COVID-19 pandemic[29 ]. A further survey of 252 centres from 55 countries, reported a consistent reduction in endoscopic activity across all continents[30 ]. The United Kingdom’s BSG issued guidance on the resumption ofGI endoscopic services in the United Kingdom[31 ] during the recovery phase after the pandemic’s first peak in 2020 . In addition to restoring specialist staff, it was advised that there needed to be increased infection control to minimise peri-procedural infection spread[32 ], including additional time and space for procedures, secure supplies of personal protective equipment (PPE), and the need for COVID-19 -minimised facilities, where COVID-19 positive patients, are separated from those that are unlikely to have the infection. To accurately separate patients, individuals were screened for symptoms and tested for COVID-19 prior to endoscopy, with COVID-19 patients often deferred to the end of an endoscopy list, or indeed their procedure undertaken in a different hospital area. Similar guidelines were issued by gastroenterology organisations in other parts of the world,e.g., America[33 ], Europe[17 ] and Asia[34 ]. A multi-centre prospective study of COVID-19 transmission in 6208 patients having outpatient endoscopy, found low prevalence of transmission peri-endoscopy if performed in a ‘COVID-19 -minimised pathway’, which consisted of symptom screening and/or a COVID-19 reverse transcriptase polymerase chain reaction (RTPCR) swab of patients prior to procedure. In total, 2611 patients in the study had a COVID-19 swab pre-procedure, and only 3 tested positive, all of whom were asymptomatic. None of the patients developed symptoms of COVID-19 within two weeks after the procedure based on telephone follow-up[35 ]. It should be noted that data for this study was collected during the recovery phase of the first peak in United Kingdom (Summer 2020 ), when community prevalence of COVID-19 was low. In contrast, Alboraieet al[7 ] found that 25 .8 % of participating centres (from 48 countries)reported positive cases of COVID-19 amongst patients within two weeks of their procedure date, although the percentage of positive cases within each individual centre was not reported. The data, however, included patients requiring urgent endoscopy and was not limited to COVID-19 -minimised sites, which may have accounted for the higher infection rates. GI endoscopic procedures generate significant aerosol[36 ]. Therefore, the importance of air flow was imperative, as it was recognised that post-procedure turnover time or ‘down-time’ was required to let aerosolised particles settle and therefore reduce potential cross-infection. The down-time is dependent on air flow cycles within the procedure room to reduce the particulate burden of air, the procedure type and the Covid status of patient[37 ]. Infection control reviews of some units revealed suboptimal air exchange in endoscopy rooms and a lack of infection prevention training in some units. A survey of 83 institutes by Hungarian Society of Gastroenterology revealed 33 .33 % participants had infection prevention training, less than 1 % said that they have negative pressure procedure rooms, and only 20 % reported that they have some form of mechanical ventilation or air purification system[38 ]. It was not easy to implement all the recommendations quickly with resultant delays in resumption of endoscopic services. These operational issues and others, such as: redeployment of endoscopy staff, reconfiguration of endoscopy units/ service pathways, pre-procedure triage of patients and COVID-19 testing, and enhanced PPE significantly added to the workload of staff.
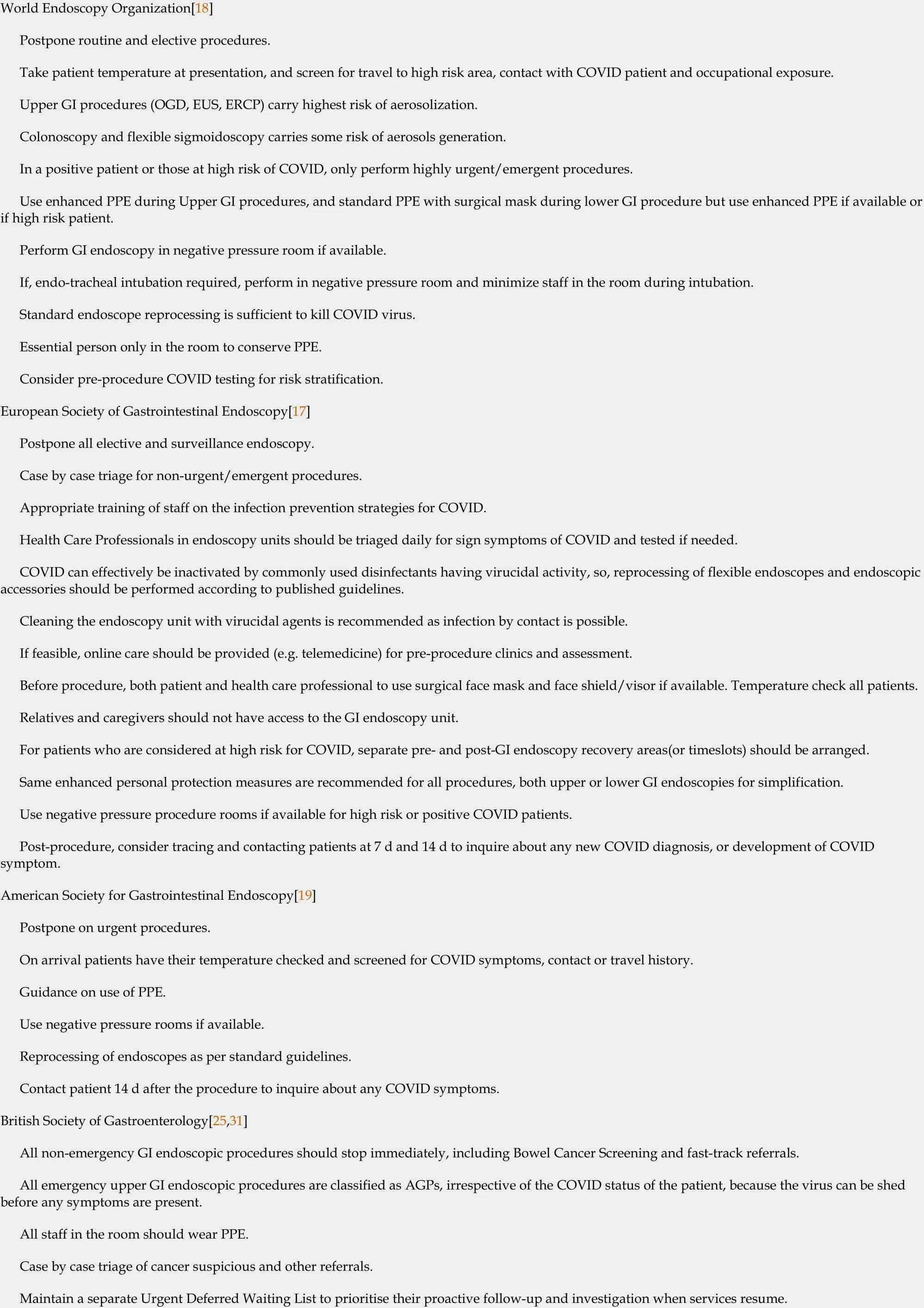
Table 1 Summary of advice on Endoscopy service provision during the peak of COVID-19 pandemic from major societies around the world (March-April, 2020 )
Subsequent guidance recommended to consider pre-procedural symptom screen and COVID testing with separation of high risk COVID sites from COVID minimised sites for low risk patients.Indian Society of Gastroenterology[21 ]Postponed routine non-urgent procedures Screen patients pre-procedures with symptoms screen, travel and contact history.Take temperature of all patients pre-procedure.Minimum number of staff in the procedure room.Use appropriate PPE based on risk assessment and stratification.Standard disinfection processes are effective against COVID.Surgical masks for patients’ use too, if they have respiratory symptoms.AGP: Aerosol-generating procedure; ERCP: Endoscopic retrograde cholangiopancreatography; EUS: Endoscopic ultrasound; GI: Gastro-intestinal; OGD:Oesophago-Gastro-Duodenoscopy; PPE: personal protective equipment.
Colorectal cancer services
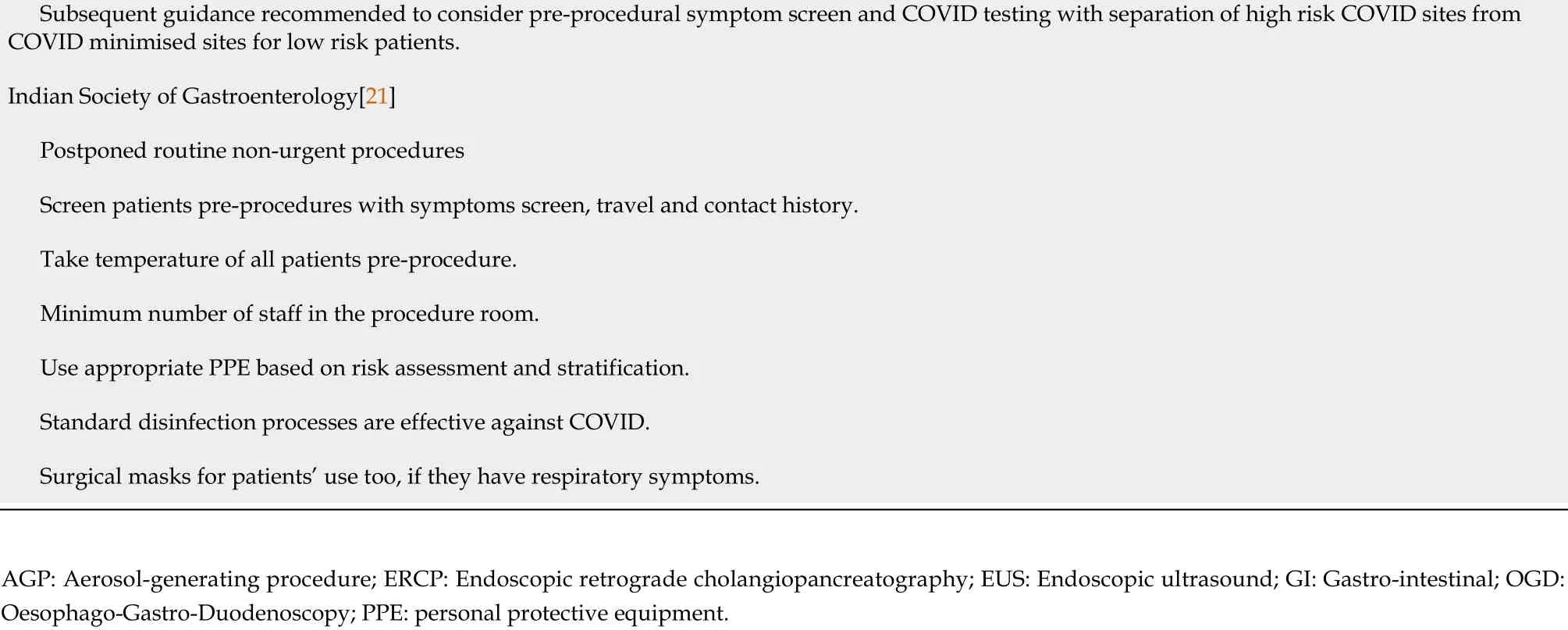
The COVID-19 pandemic has had a major disruptive impact on colorectal cancer service provision. Deviation from the national guidelines was observed at every point in the patient care pathway including referrals, endoscopy/colonoscopy, surgery provision, surveillance and patient follow-up[39 ]. The degree of disruption varied between units both in the United Kingdom[40 ] and internationally[39 ,41 ]. Following cessation of non-emergency endoscopy and BCSP during the first wave of COVID-19 ,Rutteret al[42 ] analysed the United Kingdom’s ‘National Endoscopy Database’[42 ],and demonstrated that endoscopic activity reduced significantly compared to pre-COVID-19 Levels by an average of 12 %, but declining to 5 % at the lowest point(Figure 1 ). The authors reported an increase in the per-procedure cancer detection rate,owing to labour-intensive triage of the existing endoscopy waiting lists and of new referrals by senior clinicians. Despite this, the weekly number of cancers detected decreased by an average of 58 % compared to pre-COVID, suggesting 72 % of colorectal, 37 % of oesophageal, 52 % of gastric, and 19 % of pancreato-biliary cancers may have been missed. This was a substantial and concerning reduction in cancer detection due to decreased endoscopic activity. Reduced procedure rates were confirmed by other studies, with reports of decreased adherence to colorectal screening programmes[39 ], and an 81 % drop in colonoscopic activity, during the pandemic[7 ]. Maringe et al[43 ], modelled the impact of diagnostic delays on patient survival in the United Kingdom, and estimated that there would be 15 .3 %-16 .6 %additional deaths in colorectal cancer patients, and an increase of 5 .8 %-6 .0 % in deaths by oesophageal cancers. This data highlighted the severe consequences of reduced endoscopy services during the COVID- 19 pandemic, with substantial foreseeable increases in the number of avoidable cancer deaths, as a result of these diagnostic delays. A cross-sectional study from the United States assessed the weekly number of newly identified breast, colorectal, lung, pancreatic, gastric and oesophageal cancers during the COVID-19 pandemic. The authors found that detection fell 46 .4 % (from 4310 to 2310 ) for the 6 cancers combined[44 ].
Management of liver diseases and liver transplantation
COVID-19 affected liver transplant services throughout the world. In the United Kingdom, 7 adult and 3 paediatric centres performed 8740 Liver transplants performed in the United Kingdom in the last ten-year period[45 ]. National Health Service Blood and Transplant and the United Kingdom Liver Advisory Group updated and reviewed guidance throughout the pandemic. Liver transplantation centres were advised to continue procedures on a case-by-case basis - largely for patients in a clinically urgent category [based on high ‘United Kingdom Model for End-Stage Liver Disease’ scores or hepatocellular carcinoma (HCC) on verge of going out of transplant criteria]. Where possible, activity was continued for all super-urgent liver transplantation. Age for donation after brainstem death was restricted to 60 years and donation after circulatory death restricted to 50 years on March 23 , 2020 , with a projected transplant reduction of 51 %[46 ]. After further appraisals, these donor criteria were relaxed later in the 2020 . During the peaks of COVID-19 , some centres temporarily suspended all liver transplant activity (except for extremely super-urgent cases) due to a surges in hospital admissions, shortages of ICU beds, and organ procurement restrictions implemented by the organ donation authority[47 ,48 ]. The number of liver transplantations in the United Kingdom fell by 84 % (3 nationally per week) during the first COVID-19 peak[46 ]. On average, the number of patients on the United Kingdom liver transplant waiting list at the end of each month between January 2019 to March 2020 , was above 400 . This number fell rapidly to 109 during the first peak, by May 2020 , with only clinically urgent patients being left on the waiting list and the remaining patients temporarily suspended[46 ]. At the time of writing, the United Kingdom again has severe restrictions in place for liver transplantation activity, due to a further surge of COVID-19 infections (February 2021 ). Analyses from the National Organ Procurement Agency in France, and the United Network for Organ Sharing in the United States, in April 2020 , demonstrated a reduction in solidorgan donor transplantations by 90 .6 % and 51 .1 % respectively[49 ]; this was predominantly due to fewer kidney transplants, but there was also a substantial decrease in liver, lung and heart transplants. The American Association for the Study of Liver Diseases (AASLD) recommended postponing liver transplantation, advising each programme to consider its capability regarding ICU beds, ventilator availability and blood donation[50 ]. The Saudi Association for the Study of Liver Diseases and Transplantation published a position statement, advising that efforts should be made to persevere with normal transplant activity, but with the adoption and flexibility of individual transplant pathways, including virtual tele-medicine consultation to avoid patient contact and stricter preventive measures[51 ]. The European Association for the Study of the Liver (EASL) advised that centres should prioritise patients who have a poor short-term prognosis without liver transplant, including those with acute liver failure, high MELD score and HCC[52 ]. The liver transplant society of India recommended a moratorium on all non-urgent transplants during the initial COVID-19 peak[53 ]; similarly, the Pan-Arab Association of Gastroenterology recommended that non-urgent transplants should be postponed[54 ]. Hepatology societies across the world provided guidance for the management of patients with liver diseases in both inpatient and outpatient settings, and on liver transplant (Figure 2 ). The AASLD[55 ],EASL[56 ] and the European Society of Clinical Microbiology and Infectious Diseases(ESCMID)[13 ] all advised: To separate COVID-19 positive and negative in-patient cohorts with liver disease, minimise contacts by reducing staff levels during ward rounds, limit the number of investigations performed and have restrictions on visitors.Similarly, for outpatients, the societies recommended that units offer remote consultation for appointments and only perform essential investigations. Bollipoet al[10 ] summarised these recommendations including advice on the management of liver transplant, endoscopy, liver cancer, and both inpatient and outpatient care. A multicentre, retrospective, cross-sectional study by Amaddeoet al[57 ] found that fewer patients with HCC presented to the multidisciplinary meetings, and had a treatment delay that was longer in the COVID-19 period than in 2019 .
Figure 1 Reduction in United Kingdom wide endoscopic activity (cumulative number of procedures/week) during 1 st peak of COVID-19 infections. Source: United Kingdom’s National Endoscopy Database analysis, Rutter et al[42 ].
IBD services

Figure 2 Summary of recommendations from major Hepatology societies across the world on management of liver diseases during the pandemic. Sources: American Association for the Study of Liver Diseases[55 ]; British Society of Gastroenterology[9 ]; European Association for the Study of the Liver[56 ]; Indian Gastroenterology Society[21 ]; International Liver Transplantation Society[10 ]; Pan-Arab Association of Gastroenterology[54 ]. HCC: Hepatocellular carcinoma.
Outpatient IBD services were severely impacted during the pandemic with cancellations of clinic appointments and subsequent conversion to remote consultations[58 ].IBD surveillance endoscopy services were temporarily halted as a non-urgent endoscopic procedure. This has affected the follow-up of known IBD patients, as well as new IBD cases. With regards to new patients, cases were triaged to assess urgency and consideration made to delay diagnostic endoscopy and imaging in those with mild symptoms and moderate biomarkers[59 ]. It was recommended that initiation of therapy be on a case-by-case basis. Known IBD patients were advised to continue their current medications given the increased risk of infection associated with active disease and hospitalisation. Similar guidelines were issued by other IBD societies around the world. The European Crohn’s and Colitis Organisation advised that centres adopt virtual consultations, use a home faecal calprotectin test for monitoring, and limit endoscopic evaluations to those patients in whom it was felt to be absolutely necessary[60 ]. Recommendations to minimise contact and reduce endoscopic intervention were echoed in guidance from the International Organization for the study of Inflammatory Bowel Disease and Crohn's and Colitis Foundation of America[61 ]. Healthcare providers adopted and modified their IBD unit protocols to minimise both patientpatient and patient-health care worker contact. Centres also screened patients for COVID-19 symptoms before they attended infusion units[62 ]. A significant proportion of new IBD patients were diagnosed and treated without having endoscopic or histological evaluation[63 ]. Based on early observations from China and Italy, IBD patients were felt to be at higher risk of severe COVID-19 , particularly older patients with comorbidities, patients on high doses of systemic corticosteroids, and patients with active disease[64 ,65 ]. The United Kingdom’s BSG issued guidance to stratify IBD patients into low, medium and high-risk of a poor outcome from COVID-19 infection[59 ]. High-risk patients included those on: (1 ) Concomitant therapies (immunomodulator and biologic) who were over 70 and/or had selected co-morbidities; (2 ) Those who were receiving daily steroids (≥ 20 mg prednisolone or equivalent); (3 ) Those who had recently commenced biologics with immunomodulators or systemic steroids; and(4 ) Those who had short bowel syndrome and required nutritional support or were on parenteral nutrition. IBD patients identified as high-risk were advised to shield by the United Kingdom government during the peaks of the pandemic; they were advised to stay home wherever possible and only to leave the house for essential reasons including medical appointments. This risk assessment was consistent with findings from Brenneret al[66 ] of 525 international COVID-19 cases reported to the‘Surveillance Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease’ (SECURE-IBD) registry[66 ]; 50 % of IBD patients with a severe COVID-19 outcome (i.e., ICU admission, ventilator use, and/or death) were over 70 years of age, and 50 % of those who died had cardiovascular co-morbidities. The SECURE-IBD registry was also analysed to assess COVID-19 outcomes with various IBD medications. The major finding from these studies[66 ,67 ], was that thiopurine treatment, as both monotherapy and combination therapy, was associated with an increased risk of severe COVID-19 infection when compared with tumour necrosis factor alpha (TNF-α) antagonist monotherapy. Further findings were that TNF-α antagonist monotherapy may have a protective effect against severe COVID-19 and that no significant differences were observed in outcomes when comparing classes of biologics[67 ]. This data was consistent with previous findings that thiopurines increase the risk of viral infections compared with TNF-α antagonists[68 ]. This was reflected in real-world practice; Sharma and Meade[58 ] assessed prescribing of IBD medications in a United Kingdom tertiary hospital and found increased de-novo biologic therapy compare to pre-pandemic, particularly among thiopurine-naïve patients. The BSG recommended: not to stop current medications (to avoid any flares of IBD), to consider anti-TNF monotherapy if needed and to avoid immunomodulators[59 ]. A panel of 15 IBD experts convened to review the management of acute severe ulcerative colitis(UC) in the context of COVID-19 , recommending that patients with UC flares should be isolated throughout their hospital stay, and Infliximab along with steroids should be considered as a rescue therapy if needed. It was not deemed appropriate to commence thiopurine therapy for maintenance however steroids and Infliximab continuation was considered more appropriate[69 ]. Provision for follow-up and investigations to monitor disease response in IBD patients was impacted throughout the pandemic, providing a further rationale for initiating treatment with more efficacious agents earlier. Kennedyet al[70 ] surveyed 125 IBD services during the first peak of COVID-19 infections and found that there was a significant reduction from baseline in whole-time equivalent gastroenterologists and IBD nurses providing elective outpatient care. Of concern, 27 % of services reported no access to faecal calprotectin, and a further 32 % reported reduced access to faecal calprotectin testing[70 ], making management more challenging. Curtailment in IBD-specific services,e.g.,outpatient services, endoscopic services, regular multidisciplinary meetings to discuss complex patients and re-deployment of specialist nurses was accompanied by an increase in IBD helpline queries from patients[70 ]; 94 % of services reported an increase in IBD helpline activity. In summary, worldwide, organisations made significant changes to ensure safe care provision to the IBD population. These adaptations included: diagnosing IBD clinically in several instances without endoscopic,histological and in most cases radiological investigations, remote prescribing/Laboratory investigations and medicine infusion arrangements outside of high risk COVID-19 main hospital sites along with provisions of tele-consultations for patients[63 ,70 ,71 ]. Due to rapid changes in IBD patient services, governance structures for development of novel ways of working remains a major focus. Changes to IBD delivery structure should be discussed with patients where possible. In a survey of 685 IBD patients[72 ], participants reported that the COVID-19 pandemic has had a negative impact upon their psychological well-being and quality of life. The patients reported an increase in perceived stress with 39 % of respondents worried about their IBD care, but respondents were happy with delivery of care remotely.
(2) 中易发区:面积为1 113.95 km2,占研究区面积的30%,主要包括元城川流域中-上游区域、悦上公路沿线地区、上里塬乡、林镇乡。区内河流侵蚀强烈,相对高差较大,地质环境条件较差,人口较密集,同时也是耕地、公路、桥梁较为密集的区域。人类工程活动较强烈,区内分布地质灾害点59处。
Outpatient gastroenterology and hepatology clinic provision
Outpatient clinics were disrupted by COVID-19 , with temporary suspension of many routine outpatient clinics, and with conversion of standard outpatient face-to-face clinic consultations to telephone or virtual appointments - referred to as“telemedicine”. Emergency clinic appointments were provided depending on clinical urgency, with some centres adopting temporary email addresses or telephone helplines for patients to contact the hospital. As the first wave subsided, face-to-face appointments were re-introduced in some centres, depending on local COVID-19 policies; however, telemedicine has now been adopted and sustained by many gastroenterology and hepatology outpatient services including viral hepatology and IBD clinics. The advent of telemedicine preceded the pandemic[73 ], but its use has increased exponentially in the past year, with a study from New York[74 ] reporting an 8729 % increase in the use of video consultations during COVID-19 , accounting for 21 .9 % of outpatient visits. Worldwide, medical organisations issued guidance regarding the use of telemedicine[75 -77 ] outlining recommendations for establishing telemedicine systems, as well as ethical considerations. Broadly, telemedicine is considered appropriate for patients with straightforward complaints, who do not require physical examination, feel comfortable using the required technology, and who can be provided with all necessary information and prescriptions remotely. Key principles regarding patient identification, capacity, consent and safe information storage hold true for telemedicine as they do for in-person consultations. A multimodal telemedicine network was established in Sichuan Province, Western China, in January 2020 , in response to the COVID-19 pandemic[78 ]. The network synergised a new 5 G service, a smartphone application, and an existing telemedicine system; it was funded in the short-term by disaster funds. An expert group was established to provide education to medical staff. By March 23 , 2020 , the authors reported that 9085 patients had received online consultations or interventions through the application,and 1094viatelephone. Four hundred and twenty-four consultations were conducted for severe and critical COVID-19 patients highlighting the substantial potential of telemedicine. In addition, radiologists used the network to successfully perform remote computed tomography (CT) scanning of 152 patients, allowing quality imaging in areas with a severe shortage of qualified technicians. Various other organization have issued guidelines for remote consultations[79 -81 ]. Key principles include: Correct identification of patient at start of teleconsultation and use of available medical records/referral letters in conjunction with patient history to decide whether a safe management plan can be made remotely, or is face to face consultations required. Any remote examinations requires patient consent, with the United Kingdom’s GMC recommending the use of a chaperone during video consultation in a same way as one would do during face-to-face consultation[82 ]. Medicolegal organizations have also generated their recommendations on tele-consultations on similar basic principles[83 ].Similar recommendations to the United Kingdom GMC guidelines were issued for physicians by Ghoshet al[84 ] in India. The American Telemedicine Association has described similar principals and framework of remote consultations even before the pandemic[85 ]. The impact of telemedicine has been studied by Lee et al[86 ] in the setting of liver transplantation in a randomised prospective trial; 106 patients were randomised to standard of care face-to-face practice, or telemedicine home-based care- utilising tablets, video-calls, and texts. Participation rates, quality of life and 90 -d hospital re-admission rates were compared, with lower re-admission rates at 90 d (28 %vs58 %, P = 0 .004 ) and improved quality of life with regards to physical function and general health in the telemedicine group. Munroeet al[87 ] designed a single-arm,crossover study during the COVID-19 pandemic. A telemedicine consult,viaphone or video call, was offered to patients referred to the practice; patients could accept a virtual consult or request a review in person. The authors reported high levels of patient acceptance of telemedicine, and no discernible changes in outcomes or care-use related to medical decision-making, time to appointment or patient satisfaction. In a retrospective observational study from New York, United States, Ramaswamyet al[74 ]analysed feedback from telemedicine consultations pre- and mid-pandemic; in both cohorts, satisfaction was significantly higher with video consultations vs. in-person visits (94 .9 % vs 92 .5 %, P < 0 .001 ). McKenna et al[88 ] surveyed 212 general neurological patients from Dublin, Ireland who had attended remote consultations and found that 76 % of patients felt remote consultations were either “just as good” (67 .1 %) or “better”(9 .0 %) than face-to-face consultations. Those who reported remote consultations to be‘not as good’ were older (52 .3 years vs 46 .6 years, P = 0 .045 ) and had neurological conditions that required clinical examination (66 .7 %) or an undiagnosed condition awaiting investigation/ review (46 .7 %). The United Kingdom’s Medical Protection Society assessed doctors’ opinions on telemedicine[89 ]; of 1250 respondents 70 %agreed that the benefits of telemedicine were ‘unquestionable’ during the pandemic.However, 80 % feared that the doctor-patient relationship could ‘break down’ or were worried telemedicine might deny some patients’ treatment. Almost three-quarters of doctors expressed concern about medically missing something in a remote consultation and 60 % were worried about a claim or investigation.
THE EFFECT OF COVID-19 ON GASTROENTEROLOGY AND HEPATOLOGY TRAINING
Worldwide, COVID-19 has had a disruptive effect on the training of gastroenterology and hepatology doctors due to redeployment and cancellation of educational activities.This has been compounded in some settings by medical staff exhaustion and burnout.Most routine and non-emergency specialty services have been suspended, including a drastic reduction in endoscopic activity, and hence training opportunities for gastroenterology and hepatology trainees. Global shortages of PPE led to ‘non-essential persons’ being excluded from endoscopic lists[90 ] to conserve the supply in some hospitals. In addition, to minimise risk of infection, centres were advised to consider restricting staffing for procedures, limiting endoscopy to a small number of specialist consultants, and excluding trainees[91 ]. A survey of Australian gastroenterology trainees demonstrated a 75 % reduction in endoscopic activity, with 30 % of trainees prohibited from performing emergency endoscopy; again, to limit staff exposure and to conserve PPE[92 ]. Most training assessments, specialty exams, and continuous professional development (CPD) activities were cancelled during the first peak of COVID-19 . In May 2020 , the BSG surveyed its members and found that 66 % of United Kingdom trainees were not doing any specialty clinics, 29 % were unable to continue their formal research commitments, and 53 % were unlikely to achieve their Annual Review of Competency Progression targets, which would therefore risk prolongation of training[93 ]. In a survey of Canadian gastroenterology trainees[94 ], 94 % were concerned about achieving and/or maintaining clinical competence, and 71 % were concerned about prolongation of training due to the pandemic. During the pandemic,trainees have experienced an increase in workload, often in new clinical environments,leading to exhaustion and burnout. This, alongside missed training opportunities, has generated anxiety and stress amongst specialty trainees. In an international survey of 770 endoscopy trainees from 63 countries[95 ], 52 .4 % of respondents reported anxiety and 18 .8 % reported burnout. Cravero et al[96 ] surveyed 1420 Internal Medicine trainees from the United States, China, Saudi Arabia, Taiwan and other countries[96 ],and found that the trainees caring for COVID-19 patients were more likely to have worked additional hours compared to pre-pandemic, and that the incidence of reported burnout was proportionate to the number of COVID-19 patients that trainees had cared for. Fifty-nine percent trainees expressed concerns about their preparedness for independent practice while 20 % trainees reported that pandemic has negatively effected the progress towards their career goals. Karampekoset al[97 ] surveyed Greek gastroenterology fellows, and fellowship programme directors regarding the impact of COVID-19 on endoscopy training. The two groups broadly agreed on the factors associated with a negative impact: an unknown timeframe of COVID-19 measures,cancellation of endoscopy, and fewer endoscopies performed by fellows. The fellows were significantly more concerned about their ability to acquire and/or maintain endoscopy competence than their programme directors (83 .1 % vs 27 .8 %, P < 0 .001 ). In addition, proposed strategies to address training post-pandemic varied with fellows predominantly suggesting prolongation of training (49 .4 %) and programme directors suggesting an increase in daily workload (44 .4 %). This study highlighted the importance of involving both trainees and programme leaders in planning and decision-making for training during and after the COVID-19 pandemic. Finally,remote working (e.g., telemedicine) has allowed some flexibility in doctors’ working patterns - clinics can be performed from offices or from home with remote access to patient data. This was actively encouraged by some hospitals to reduce clinician footfall within the hospital during the COVID-19 pandemic. However, there was a resultant effect on training with fewer opportunities for direct learning and an inability to gain immediate, face-to-face advice from supervisors.
PROPOSALS FOR GASTROENTEROLOGY AND HEPATOLOGY SERVICEPLANNING AND TRAINING PROVISION DURING THE COVID-19 PANDEMIC AND BEYOND
There has been a significant increase in the caseload of COVID-19 patients in recent months, and it is clear that the pandemic is far from over. In addition to direct COVID-19 -related morbidity and mortality, there has been significant collateral damage, due to disruption in routine and urgent health services, such as cancer workload. After the 1 st wave, the rate of COVID-19 related admissions slowed and the services began to recover. However with mutation of the virus, surges in COVID-19 cases recurred with most countries thereafter experiencing a 2 nd and some 3rdwaves. At time of writing, the delta-variant is on the increase in the United Kingdom. With experience gained in planning for surge capacity in hospitals, reconfiguration of services has been easier for many in the 2 nd wave and now 3rdwave. Services however are constantly running at high volume, often exacerbated by winter pressures (in Europe) meaning healthcare services remain at constant risk of being overwhelmed. In this section, we discuss recommendations to ensure optimal continuity of patient care and gastroenterology/hepatology training during the pandemic (Figure 3 ), and indeed new approaches could continue well after the pandemic has ended. It should be reinforced that general principles of adequate PPE, social-distancing measures, robust contact-tracing systems and the roll-out of COVID-19 vaccines remain crucial pillars for controlling COVID-19 on mass population levels.
Protecting the workforce
Adequate PPE and infection-control measures are essential to allow staff members to remain safe whilst caring for COVID-19 patients. A study of 420 healthcare workers deployed to care for COVID-19 patients in Wuhan, China[98 ], demonstrated that effective infection prevention measures protected the workforce from getting infected -despite working an average of 100 -130 h in the ICU, none of the participants reported symptoms of COVID-19 and all remained antibody negative. The study highlighted the importance of the procurement and distribution of PPE, as well as providing adequate training to healthcare professionals in its use. Thomaset al[99 ] appraised global PPE guidance and the available scientific evidence regarding aerosols, virus transmission, and respiratory protection. The authors concluded that there were shortcomings with the Public Health England’s PPE guidelines and recommended urgent revision to protect the United Kingdom’s NHS workforce during the pandemic.Rising infections and deaths amongst healthcare workers worldwide prompted calls for urgent action and PPE provision[100 -103 ]. In parallel to PPE provisions, the vaccine rollout remains key in protecting the workforce. In many countries, healthcare staff have been identified at a high-risk group and targeted for vaccination early. This is in conjunction with medically at-risk patients and also the elderly. Mental and physical wellbeing of healthcare workers is required for optimal performance, and health care organisations and medical unions should have resources in place. Hospital organisations should ensure where possible, that staff have adequate breaks on shifts,and there are adequate provision of rest facilities, especially given ‘social-distancing’requirements. It is increasingly recognised that the pandemic will have a psychological impact on the majority of healthcare staff, and support must therefore be put in place[104 ]. Early experiences from China[105 ], and more recently from Europe[106 ], suggest that healthcare staff are likely to experience negative mental health outcomes due to the pandemic. In addition, with the increased workload burnout is becoming more common[96 ]. In the United Kingdom, NHS England recommended support and flexibility for staff working during the pandemic[107 ]. Tomlin et al[106 ] proposed a phased model of the mental health burden, in which stressors from different phases of the pandemic are considered and coping strategies were suggested for both the individual and the organisation for each stage. For example, in the preparation phase individuals should be aware of anxiety levels and stress triggers, and the organisation is advised to identify those who may experience challenges to their mental wellbeing.This may be particularly relevant to those with existing mental health difficulties,those with caring responsibilities and those who have recently survived a stressful or traumatic experience. By identifying vulnerable staff members and putting resilience and well-being plans in place, hospital organisations can take a proactive approach to supporting staff thereby minimising harm.
Ring-fence the specialist workforce
During surges of COVID-19 infections, much of the specialist workforce was redeployed to care for COVID-19 inpatients. Initially, it was assumed that a short period of disruption in services would cause minimal harm; however, more recent data has highlighted significant missed and delayed diagnoses as a result[42 ,43 ]. In subsequent waves of infection, a proportion of the specialist workforce where possible should aim to continue working within the specialty; for gastroenterology and hepatology this would include doctors, specialist nurses and endoscopy staff, all of whom are essential to sustain the components of the service - in-patient caseload, outpatient clinics and endoscopy lists. A balance between ongoing service provision for the COVID-19 pandemic and that of existing and ongoing services for gastroenterology and hepatology must be found.
COVID-1 9 -minimised sites
The objective of ‘COVID-19 -minimised’ sites, also known as ‘cold’ sites, is to physically segregate COVID-19 patients from those that are not infected, ideally on separate sites (coldvshot sites). This allows units to provide endoscopic and outpatient services to gastroenterology and hepatology patients while minimising their risk of COVID-19 contacts. The United Kingdom’s BSG proposed a telephone screening questionnaire, termed the ‘SCOTS criteria’[108 ]; 3 -7 d prior to endoscopy,the patient is asked if they have symptoms of COVID-19 or have come into close contact with a known or suspected case in the preceding 14 d. They interviewer should also consider supplementary factors such as the patient’s occupational risk of exposure, recent travel from a known risk area, and if that patient is in a shielded category. For patients reporting any of the SCOTS criteria, clinicians should consider if the procedure can be delayed for 14 d or if an alternative can be offered. If not, level 2 PPE should be used and procedure performed in a ‘hot’ location. Screening should be combined with a COVID-19 test pre-procedure. Kim et al[109 ] performed a metaanalysis of 19 studies, predominantly from China, to assess the diagnostic performance of RT-PCR, the commonly used COVID-19 screening test; they reported a pooled sensitivity of 89 %. The negative predictive value reduced as COVID-19 prevalence increased, ranging from 99 .9 % with 1 % prevalence to 93 .4 % at 39 % prevalence. Despite this variation, the data suggests that combining a screening questionnaire with an RTPCR swab prior to procedure would allow accurate triage of patients to either COVID-19 -minimised or high-risk sites for endoscopy. COVID- 19 -minimised sites ensure safe service provision and enhance patient confidence in attending healthcare facilities during the pandemic. With the advent of vaccinations, COVID-19 passports for visits for endoscopic procedures or to hospital may be considered when risk stratifying patients, however remains to be clarified based on long-term immunity data and risk of infection thereafter.
Training and governance for telemedicine
Despite advances in technology, telemedicine has been a novel concept for a substantial proportion of health care workers. There was no formal training or governance structure in place in many hospitals due to the speed of rollout of this modality during the pandemic. It is recommended, especially for junior trainees, that remote consultations are undertaken at a location where a consultant is available for opinion and supervision (i.e., hospital clinic rather than from home). This would provide the structured approach and will enable trainees and supervisors to have close liaison and immediate contact for questions. Another format proposed could be mixture of face-to-face and remote consultations within a same session. This would ensure social distancing for visiting patients at intervals while having teleconsultations in between in appropriate patients. There are pros and cons to remote clinics[110 ]. The pros include working remotely both for clinician and patient without the need for travel thus minimizing COVID-19 contact risk and preserving PPE used during face to face consultations. Remote clinics also acts as initial triage of patients to identify those who would benefit from face-to-face consultation. Cons include no clinical examination and a lack of visual clues. Issues also may exist contacting patients or conversing with those not speaking native language to the healthcare professional. It is important to consider patients who either can’t use or don’t have access to the internet or telephone resources. Consultation from all stake holders is required before starting a new remote consultation service, otherwise conflicts may arise. One recent example was that Government of India launched the ‘e-sanjeevani’, a national teleconsultation service during the pandemic while Indian Medical Association issued an advisory against the use of telemedicine in most situations, creating confusion amongst medical community[111 ]. Appropriate allocation of time and planning is required for both to face-to-face consultations and remote consultations in terms of time allocations for appointment and job planning[112 ]. Clinical exam might not be performed for remote consultations but other logistic issues like arranging investigation requests and prescriptions are important part of remote consultations and require allotted time.From the patient perspective, these remote consultations should be booked and organized as timed slots as one would expect with face-to-face consultations, rather than them being called at random time or date.
Exploring alternative investigations and practices
Using evidence-based practices, alternative investigations and modified pathways(Figure 4 ) may have a role to replace some of the more resource-intensive services and tests.
Primary care referral triage:Advanced triage of primary care referrals is not a new concept. An example of this was The Royal Wolverhampton Trust, United Kingdom,developing a ‘Clinical Assessment Service’ (CAS) in 2014 -2016 [113 ]. A Gastroenterologist reviewed primary care referrals, arranged investigations if necessary, and either discharged the patient back to primary care with advice, or arranged an outpatient appointment. The authors reported that 32 % of triaged CAS patients were managed without the need for an outpatient appointment. In the first three years of using CAS,3136 fewer outpatient appointments were required, which translated into a 481613 GBP cost saving. A Californian study of Rheumatology referrals reported similar results with 1 /4 of e-referrals being resolved without a clinic appointment over a 4 -year period[114 ]. The COVID-19 pandemic has demonstrated a need for widespread development of such services. During the pandemic, triaging has been used for 2 WW and USC referrals; there is scope for this to be expanded to include many other primary care gastroenterology and hepatology referrals. Another concept is ‘patientinitiated’ follow-up or review, which has been pioneered by NHS Scotland (United Kingdom) during the pandemic[115 ]. For certain patients - those who are stable or maintained on long-term treatment, an alternative approach can be offered, in which the patient requests reviews based on their wants and needs, rather than being allocated routine appointments. Caveats exist for this method: patients require clear guidelines for when to request reviews and they must be able to confidently selfmanage their condition. As a result a patient-initiated approach is unlikely to be suitable for certain cohortse.g.alcoholic liver disease patients. In March 2019 , Whearet al[116 ] conducted a meta-analysis of 17 randomised trials assessing patient-initiated follow up in patients with chronic health conditions. The authors demonstrated that patient-initiated appointment approach had little or no effect on patient anxiety/depression and patient satisfaction scores, when compared with consultant-led appointment systems. The need to adopt such frameworks in routine practice has become crucial during the pandemic, to minimise contact and to prioritise service provision for those who need it most urgently.
Endoscopy:Endoscopy services have been disrupted and limited during the COVID-19 pandemic, and since services have resumed, there is added cost to each procedure due to associated infection-control procedures and PPE. Therefore, alternative pathways and resources have been trialled, to triage patients and streamline services.Faecal occult blood or Faecal immunochemical tests (FITs) have been used to triage 2 WW lower GI suspected cancer referrals[117 ]. In 2019 , six United Kingdom ‘FIT pioneer sites’ shared data regarding FIT positive and negative cancers, in a combined 9182 patients[118 ]. The number of FIT negative cancers was 0 .01 %-0 .75 %, with a negative predictive value of at least 99 .05 %. The incidence of FIT-negative cancers was highest in those with iron deficiency anaemia, suggesting that alternative methods of triage may be required in these patients. A pre-pandemic single centre study from Scotland, United Kingdom of 5422 patients[119 ], assessed the use of FITs in significant bowel disease (SBD) including colorectal cancer, high risk adenoma and IBD. The findings suggested that use of FIT in conjunction with a full blood count and clinical assessment correctly identified 93 .9 % of all SBD. There were fewer referrals to secondary care (15 .1 % reduction) and an increased yield of SBD detection (13 .9 % to 20 .5 %), suggesting that patients were appropriately targeted for colonoscopy. Of those not immediately referred, only 0 .7 % were found to subsequently have SBD.Widespread implementation of FIT testing may therefore provide an effective and safe way to identify patients at risk of SBD. Faecal calprotectin is an effective tool to distinguish between IBD and functional GI disorders[120 ]. It also correlates well with endoscopic and histological disease activity in known IBD patients[121 ], and therefore is a suggestion that serial faecal calprotectin measurement could be used to monitor disease activity and to detect relapse early. During the pandemic, CT-colonography(CTC) could be used preferentially to optical colonoscopy to screen patients for colorectal cancer[122 ]. CTC imaging is acquired by a single healthcare worker, and requires only a limited duration of close proximity with the patient. It is performed with disposable equipment and there is minimal exposure to stool. Such radiological alternatives may therefore reduce the risks associated with COVID-19 and preserve PPE. Staffing requirements would be minimised, but it should be noted that radiology services may also see increased caseloads with surges in COVID-19 infections.Validated clinical questionnaires could replace previous initial evaluation pathways and ‘direct to test’ endoscopy referrals during and following the pandemic. The Edinburgh Dysphagia Score[123 ] uses six parameters to stratify patients into high and low risk of cancer: age, sex, weight loss, duration of symptoms, location of dysphagia and acid reflux. In 435 patients, it was found to have a sensitivity of 97 .5 % in correctly stratifying cancer patients to the high-risk group; 30 % of referrals were stratified to the low risk group and could therefore be investigated less urgently. The Eckardt Score could be used for evaluation in achalasia[124 ]. Cytosponge is a nonendoscopic,ingestible, sampling device and may provide a non-AGP alternative for diagnosis of Barrett’s oesophagus[125 ] during the pandemic. It has also been shown to have potential as a triage tool for endoscopy, in patients with mild to moderate dysphagia with suspected oesophageal cancer[126 ]. Similarly, colon capsule endoscopy is an ingestible device that allows visualisation of the bowel without attendance at hospital.It is equally effective when compared to colonoscopy for identifying polyps more than 10 mm in size and more sensitive than radiological investigations in the detection of colorectal cancers[127 ]. It may be an effective and safe alternative to colonoscopy during the pandemic[128 ]. New methods to triage and stratify patients who require endoscopic procedures could significantly reduce the demands on this service.However, the clinical effectiveness of using these new approaches will need to undergo rigorous testing and trials to ensure patients with significant pathology are not experiencing delays to endoscopy, or indeed being missed altogether. The United Kingdom’s BSG updated guidelines on polyp surveillance towards end of 2019 [129 ]that could mean reduction in number of surveillance colonoscopy procedures[130 ].The units needed to validate their existing waiting lists in view of this updated guidance but pandemic hit in early 2020 . It is imperative that validation work continues, especially when there is additional backlog of procedures when the activity was reduced during the pandemic. Non-biopsy protocol for coeliac disease diagnosis could also avoid need for endoscopy in patients who are symptomatic and IgA TTG ≥10 × upper normal limit on two occasions or one positive IgA TTG accompanied by positive endomysial antibodies (especially in children). Clinicians should be mindful of proceeding with requesting endoscopy though, if there are alarm symptoms present or if the patients belong to older age groups (≥ 55 years)[131 ]. It is important to incorporate alternative pathways as much as possible, as a modelling study from United Kingdom suggests that even with mitigation measures, it may take till after 2022 to clear backlog of endoscopic procedures[132 ].
Hepatology:Routine (non-urgent) Fibroscan® services were deferred in many hospitals during the peak of the COVID-19 pandemic[133 ]. Tests such as the Enhanced Liver Fibrosis test[134 ] or AST to Platelet Ratio Index[135 ] could be used as an alternative to assess fibrosis remotely. For patients with cirrhosis for whom endoscopy was recommended prior to the COVID-19 pandemic, for screening and surveillance of varices, it was suggested to initiate non-selective beta blocker (NSBB) therapy based on clinical judgement, taking into account Child Pugh class and platelet count[136 ].Similarly, in patients with advanced fibrosis or cirrhosis, or at high risk of having portal hypertension and varices, the BSG advised to consider starting NSBBs treatment prophylactically during the pandemic[136 ,137 ]. The Baveno criteria[138 ] could be used to identify patients at low risk of having varices, though this would require Fibroscan services to be operational; arguably easier and associated with a reduced risk of COVID-19 transmissionvstraditional endoscopic services. AASLD advised to postpone HCC surveillance from 6 mo to 8 mo in most cirrhotic patients who do not have key risk factors for HCC development[139 ]. The BSG[140 ] and EASL[13 ] also advocated delaying HCC surveillance during the peak of infections. Mehtaet al[141 ]reviewed guidelines from various hepatology societies and provided recommendations on HCC surveillance and monitoring. The authors advised that surveillance should not be performed in patients who are unlikely to benefit, such as those who were not transplant-eligible with Child Pugh Class C cirrhosis or significant, lifelimiting, co-morbidities. Similarly, it was advised against surveillance in low-risk groups such as Hepatitis C and non-alcoholic steatohepatitis patients without cirrhosis given the marginal risk-benefit ratio. Clinicians at NHS Tayside, Scotland, United Kingdom developed an automated ‘intelligent liver function testing’ (iLFT) algorithm in 2018 [142 ]. Abnormal liver function tests (LFTs) were combined with clinical features, diagnostic criteria, investigation ordering and reporting, and a tracked blood sciences system; the algorithm then generated a diagnosis or descriptor of the abnormality, with fibrosis staging. Of 568 abnormal LFTs, two thirds were managed in primary care, reducing the need for secondary care referrals. The iLFT algorithm is currently being assessed in other United Kingdom centres; this and similar systems could be incorporated into healthcare services during and after the pandemic,minimising secondary care burden. COVID-19 infection has worse outcomes in obese patients. Hence it is important to stress the need for enhanced resources to prevent and treat metabolic syndrome and associated conditions including liver disease[143 ],and the need strengthen the pathways for recognition and management more than ever.
Provision for remote laboratory investigations and prescribing
Conventionally when patients attend outpatient appointments, they have laboratory investigations and collect prescriptions during their hospital visit. With the increasing use of telemedicine, it is vital that there are safe mechanisms in place to arrange prescriptions and investigations if required. In order to avoid attendance to hospital for tests, organizations can establish blood-hubs outside main hospital sites, preferably multiple, so patients can have laboratory tests done closer to their home and without coming in contact with high risk patient areas[13 ]. These sites may be able to also provide day-case infusion services including biologics and other intravenous infusions(such as iron infusions) away from main hospitals,i.e., ‘hot’ sites. In the current digital age, healthcare providers may aim to setup a smart phone apps or a website link for patients to book appointments for tests at convenient times to them which may also avoid overcrowding at these hubs. There should also be a more conventional system (e.g., telephone appointment booking system) in place for patients who may have limited access or knowledge of using online systems or smart-phones. Remote prescribing systems are helpful for patients with chronic liver and GI diseases. A process whereby patient can be posted medication scripts is helpful in institutions that have this in place. Monitoring of medication (e.g., blood tests in patients of immunosuppression agents) is imperative to ensure safe practice. Digital prescribing -whereby the prescriber can send digital prescription to hospital or community pharmacy and these can either by collected by patients or can be posted to them, is an important resource where available. Such E-prescribing provides an auditable trail for governance purposes. These however require robust information technology systems in place and will depend on availability of resources across different parts of the world.
Optimising training opportunities
For endoscopy training there is need to ensure adequate PPE supply so this doesn’t hinder trainees’ attendance to training lists. Simulation endoscopic training can be utilized in the current pandemic, allowing trainees sufficient hands-on time. Various organizations have already adopted provision of CPD activities and have moved to online platforms. With numerous available online GI/Liver teaching resources, there has also been a boom in modalities for education such as Twitter. FitzPatricket al[144 ]reviewed how gastroenterology training can thrive during COVID-19 [144 ]. The authors discussed the challenges in learning environment during COVID-19 pandemic in endoscopy, outpatient and educational settings, and provided proposed solutions.These included adequate PPE supply, use of simulation training along with directed access to limited endoscopic activity for hands-on training opportunities (like involvement in GI bleed management), reinstatement of formal specialty training days, supervisor’s proactive discussion with trainee regarding the remote consultation undertaken. Keswaniet al[145 ] have reviewed the importance of internet-based learning, simulator training, and adoption of new educational models to maximize training during the pandemic[145 ]. Digital learning has flourished during COVID-19 crisis and has provided trainees the option of distanced learning.
CONCLUSION
It is clear there has been a major impact of gastroenterology and hepatology training but also service provision due to COVID-19 . Healthcare teams throughout the world have attempted to continue care for patients with pre-existing and new presentations of GI and liver conditions; however this provision has been extensively modified and impacted by the pandemic. Now, with new treatments for COVID-19 along with the vaccines, healthcare professionals are moving forward with a hopeful reduction in burden of the disease for patients. This in turn will allow some manoeuvrability with regards to the ongoing required non-COVID-19 service provision. A balance must exist in the fight against COVID-19 , but also ensuring ongoing high levels of care to patients with non-COVID-19 diseases. The training of the specialists of tomorrow remains vital, allowing trainees where possible a safe environment to hone their skills gaining relevant expertise but also providing high quality care to patients in the current pandemic. Whilst the COVID-19 pandemic has had a significant impact upon services and patients, novel approaches of service reconfigurations along with optimisation of existing pathways/protocols have been implemented worldwide in an attempt to maintain optimal care for gastroenterology and hepatology patients and service providers.
猜你喜欢
杂志排行
World Journal of Gastroenterology的其它文章
- Proton pump inhibitors and colorectal cancer: A systematic review
- Orexins: A promising target to digestive cancers, inflammation, obesity and metabolism dysfunctions
- Calycosin attenuates severe acute pancreatitis-associated acute lung injury by curtailing high mobility group box 1 - induced inflammation
- Prediction of genetic alterations from gastric cancer histopathology images using a fully automated deep learning approach
- Endoscopic management of difficult common bile duct stones: Where are we now? A comprehensive review
- Role of early transjugular intrahepatic portosystemic stent-shunt in acute variceal bleeding: An update of the evidence and future directions
